As we head into the holiday season and final months of calendar year 2025, the MVC Coordinating Center has been planning for its 2026 engagement activities. At MVC's most recent fall collaborative-wide meeting in October, MVC first announced several key dates and updates related to next year’s engagement offerings.
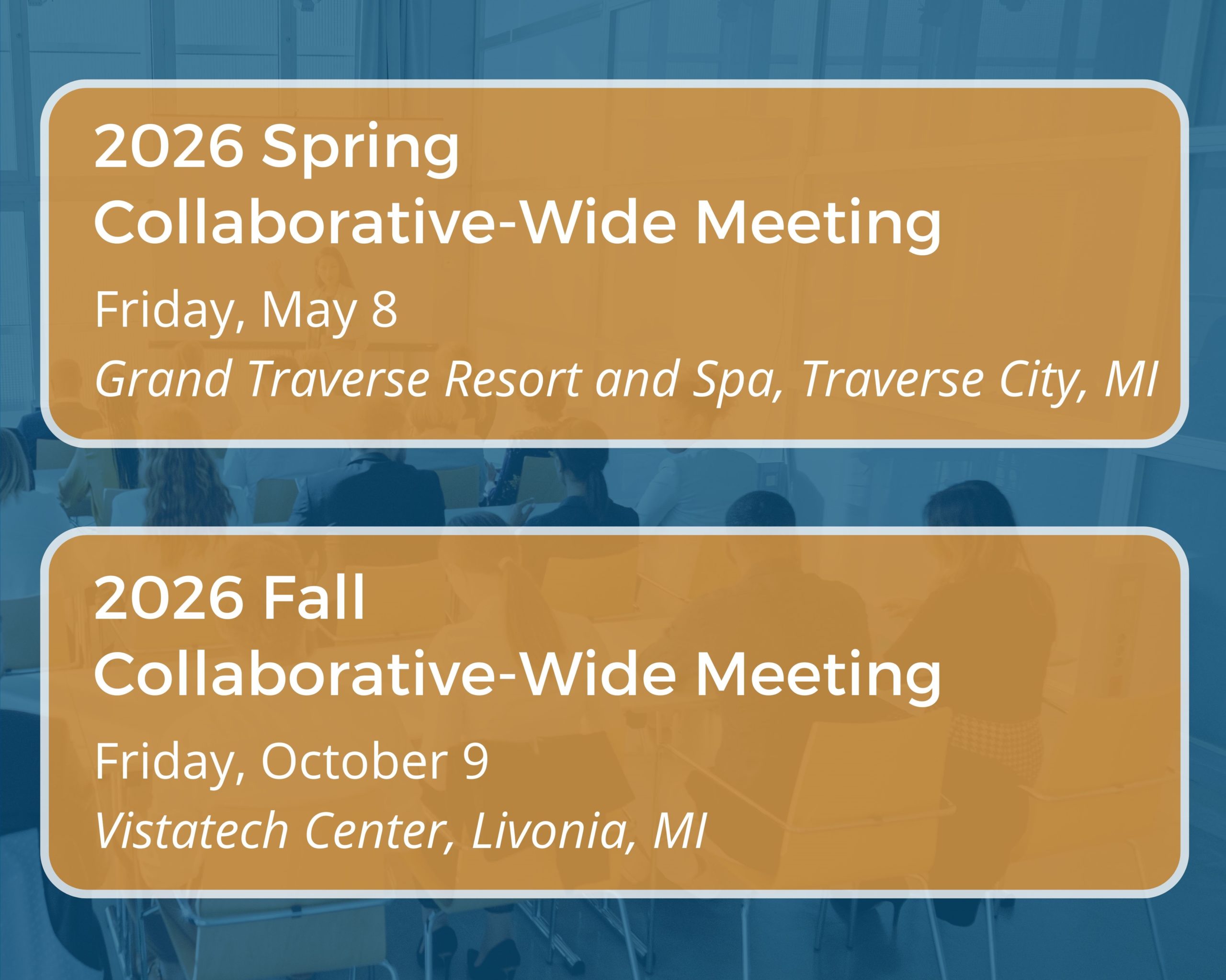
MVC’s 2026 event calendar is available now [PDF]. Of note, MVC site coordinators can see the dates for 2026 collaborative-wide meetings (Figure 1) and workgroups, as well as the months in which MVC will offer in-person or virtual networking events. MVC will head to Traverse City for its spring collaborative-wide meeting on May 8, 2026. MVC will return to Vistatech in Livonia for its fall collaborative-wide meeting on Oct. 9, 2026.
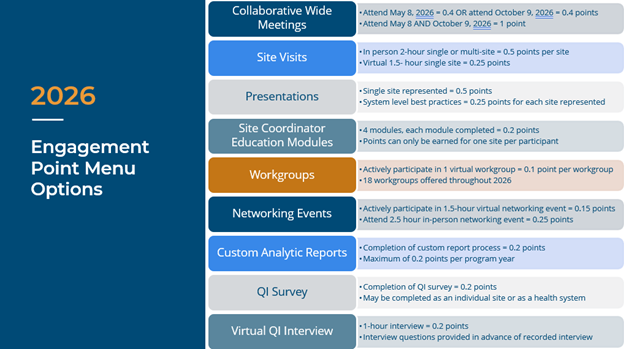
Also available is MVC’s Program Year (PY) 2026 P4P Engagement Point Menu [PDF]. Engagement activities offered in 2025 will largely continue along with some minor changes and new additions.
Earning P4P Engagement Points in 2026
In PY 2026 of the MVC Component of the BCBSM P4P Program, members can continue to earn up to two engagement points by completing eligible MVC activities. Many of the engagement point activities from PY 2025 remain available, such as attending or presenting at eligible MVC events, participating in site visits, utilizing MVC custom analytics, and survey submissions (Figure 2). Some of these offerings will have minor adjustments to their allotted point values. For example, attending a collaborative-wide meeting will now be worth 0.4 points compared to 0.25 points in 2025, and worth 1 point in 2026 for attending both meetings versus 0.75 in 2025.
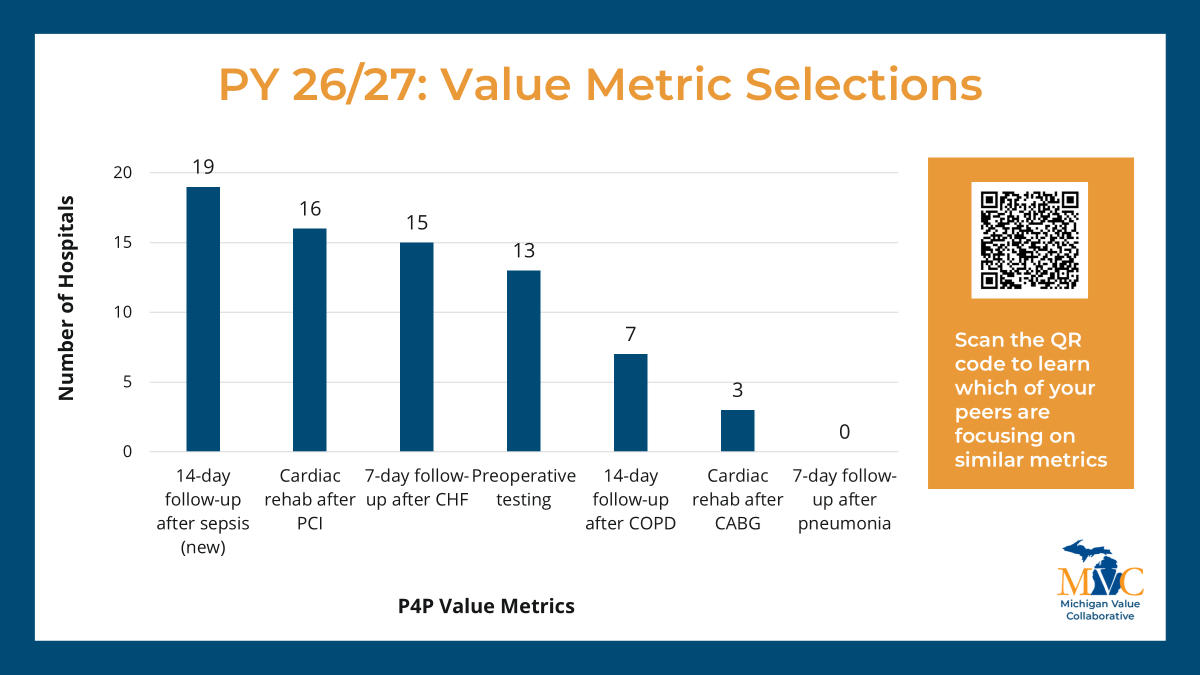
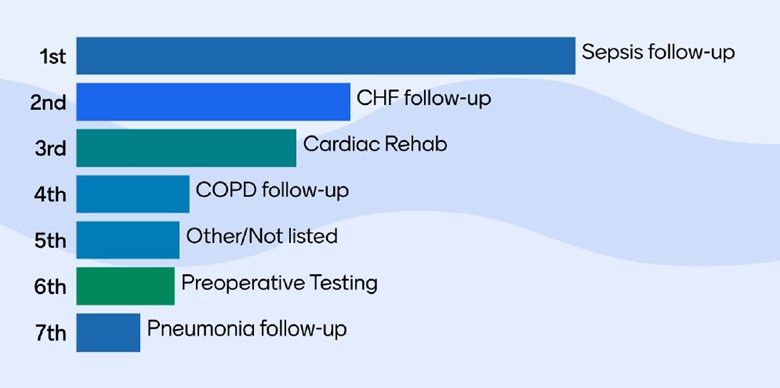
Another minor change is the number of virtual workgroups offered. MVC will offer 18 virtual workgroups in 2026; these workgroups will continue to focus on similar topics and themes, including cardiac rehabilitation, preoperative testing, post-discharge follow-up, rural health, health in action, and sepsis.
New Engagement Offering
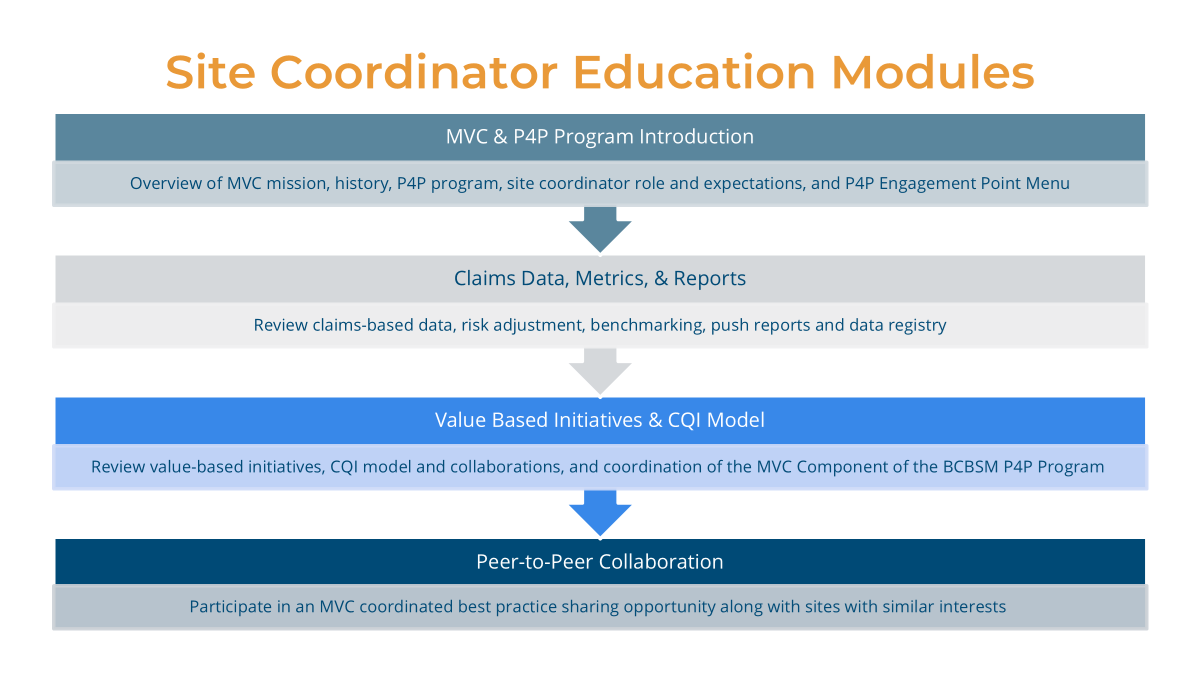
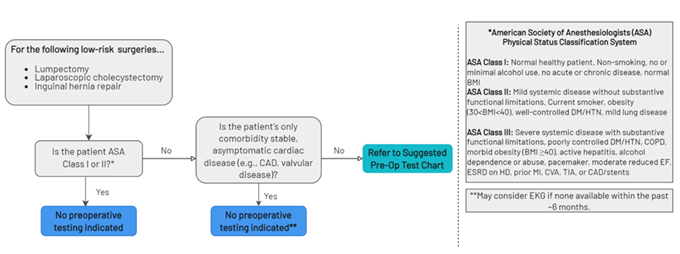
MVC is excited to introduce one new offering in 2026: site coordinator education modules. These modules will support site coordinators via one-on-one tailored training that covers a variety of topics (Figure 3). Site coordinators can receive 0.2 engagement points per module and may participate in as few as one module or all four within the performance year. Each quarter of 2026, MVC will offer limited registration to participate in a module. Registration to begin participating in 2026 Q1 will start in December 2025. Training topics provide a review of:
- Overview of MVC’s mission, history, P4P program, and site coordinator role
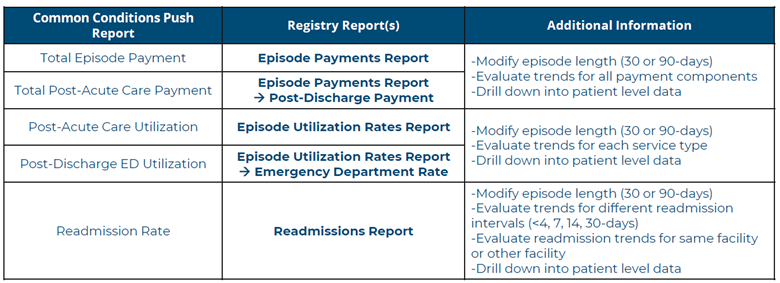
- Training on MVC claims data, metrics, and reports
- Introduction to MVC’s value-based initiatives and the CQI model
- Meeting with other site coordinators to collaborate and discuss practices
Figure 3.
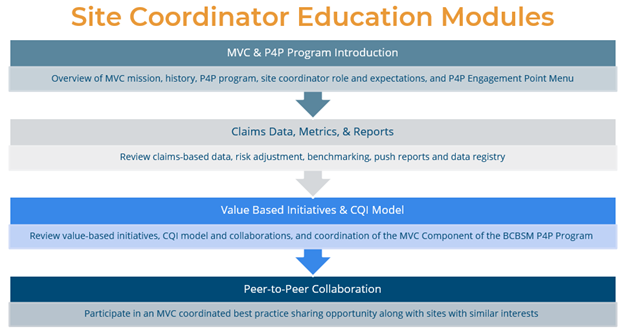
As part of the online training, site coordinators will complete a structured education plan with individualized guidance to deepen understanding of how to get the most value out of MVC’s offerings.
Earn Engagement Points by Being a Presenter
For those sites participating in the MVC Component of the BCBSM P4P Program, being a presenter at an MVC event is an opportunity to earn 0.5 points toward your hospital’s PY26 engagement points. By sharing successes, lessons learned, and helpful tools with members from across the state, presenters play an important role in improving outcomes for all Michigan patients. MVC’s Engagement team is here to support you every step of the way, making the experience of presenting as easy and comfortable as possible. Presentation proposals are accepted on a rolling basis through MVC's online form.
MVC offers a variety of opportunities to engage with the Coordinating Centers and other members of the collaborative to support peer learning, best practice sharing, and networking. These activities and events foster a collaborative learning environment that enables providers to learn from one another in a cooperative, non-competitive space, and is therefore core to MVC’s efforts to support sustainable, high-value healthcare delivery across the state. We look forward to engaging with you and your teams next year. Please contact the Coordinating Center with any questions [EMAIL].