This Wednesday, the Michigan Value Collaborative (MVC) held its first collaborative-wide rural health meeting for members. With over 50 participants representing rural and critical access hospitals (CAH), physician organizations (POs), and participating quality networks, this virtual meeting was dedicated to discussing the unique quality improvement efforts and challenges that exist within rural healthcare.
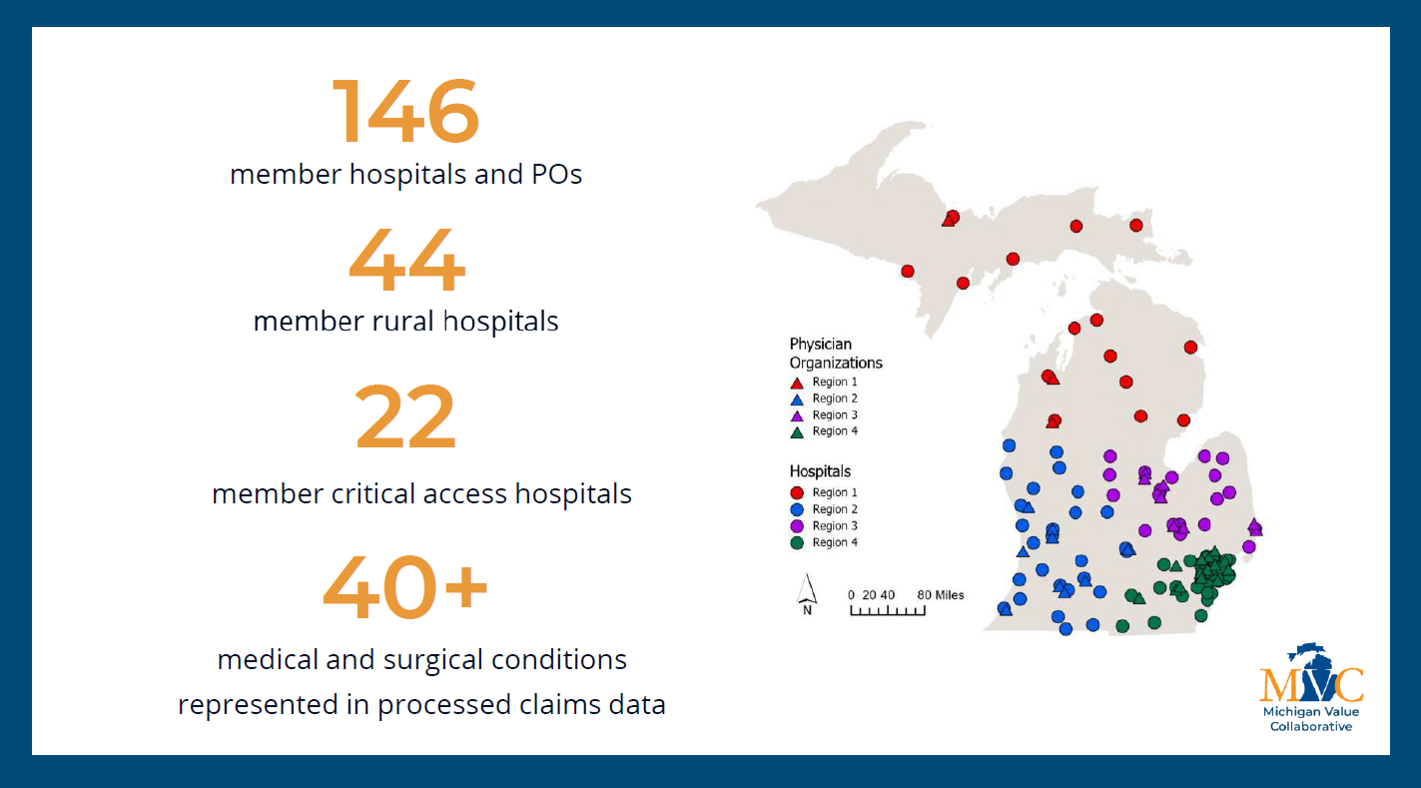
MVC Director Hari Nathan, MD, PhD, kicked off Wednesday’s meeting with an update from the MVC Coordinating Center (see slides). Honoring MVC’s 10-year anniversary, Dr. Nathan highlighted important milestones from the last decade that contributed to MVC’s continued efforts to deliver high-value healthcare in all areas of Michigan. Dr. Nathan shared updates pertaining to the launch of MVC’s new emergency department (ED)-based episodes, the recent addition of a CAH comparison group in its reporting, expanded CAH membership (Figure 1), and MVC’s plan to offer a rural health workgroup series in 2024.
Figure 1.
Following Dr. Nathan’s introduction and collaborative-wide updates, MVC Senior Analyst Julia Mantey, MPH, MUP, provided an in-depth presentation of MVC’s new ED-based episodes, which were developed in collaboration with the Michigan Emergency Department Improvement Collaborative (MEDIC). Read this recent blog post for more information on MVC’s ED-based episode structure and utilization or view Ms. Mantey’s slides here.
After introducing the components of MVC’s ED-based episodes, Ms. Mantey presented an unblinded data session illustrating ED-based episode data for MVC’s rural hospital members. When considering both rural non-CAH ED-based episodes and CAH ED-based episodes, chest pain was the most frequent condition observed. Due to its high volume in the ED, MVC produced unblinded rural hospital data using ED-based episodes for 30-day secondary ED visits among patients with a primary diagnosis of chest pain. In analyzing this data, MVC analysts discovered a correlation between patient follow-up rates and 30-day secondary ED visit rates. Patients who receive follow-up care are less likely to return to the ED in the 30 days following their initial index discharge, and the rate of secondary ED visits is smallest among patients who received follow-up care within one week of discharge (Figure 2).
Figure 2.
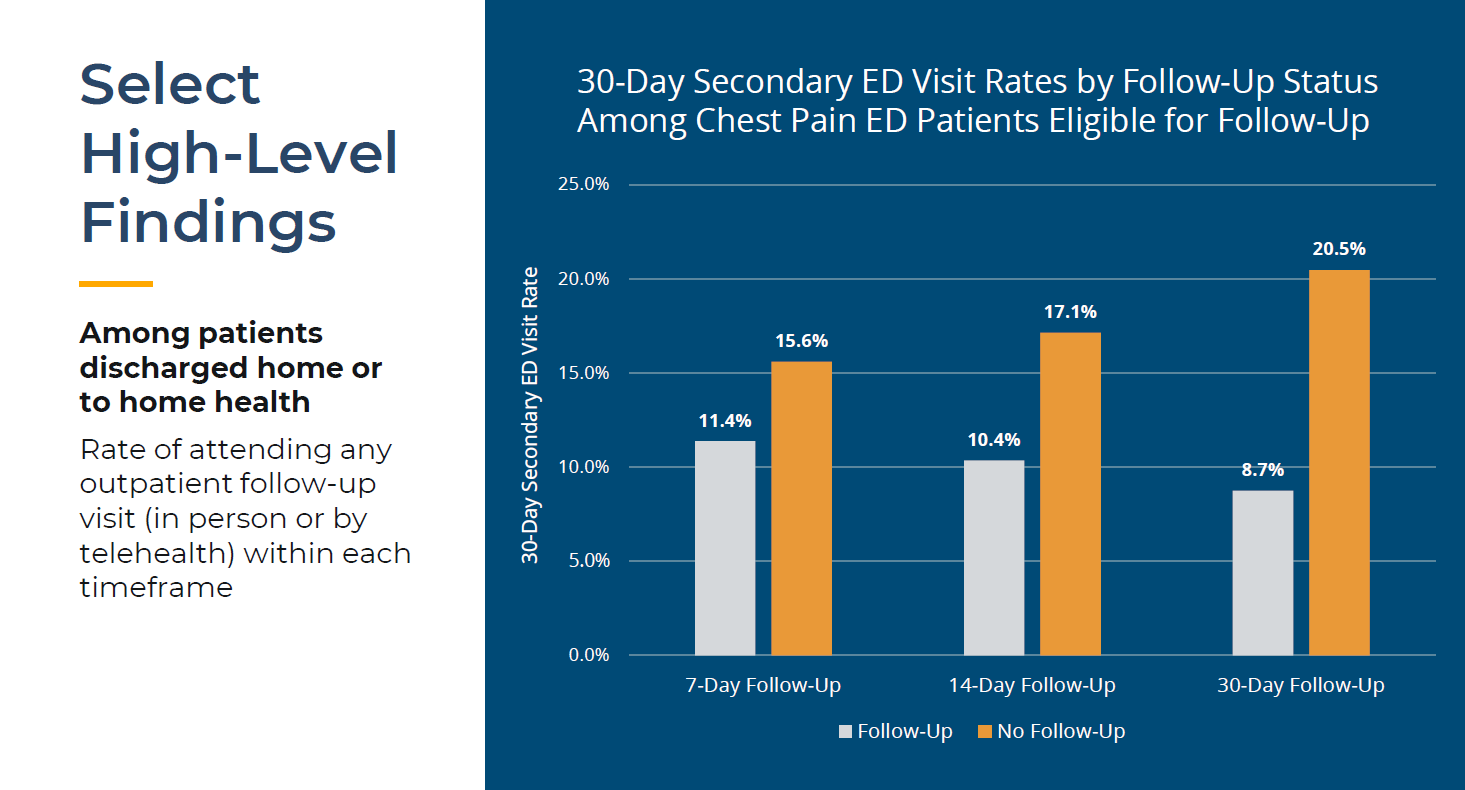
Following the unblinded data presentation, MVC received input from participants about additional analyses that would be useful, such as evaluating the correlation between the availability of nearby urgent care facilities and the rates of primary and secondary ED visits. Such suggestions were noted as MVC works to expand its CAH and ED-based episode data reporting.
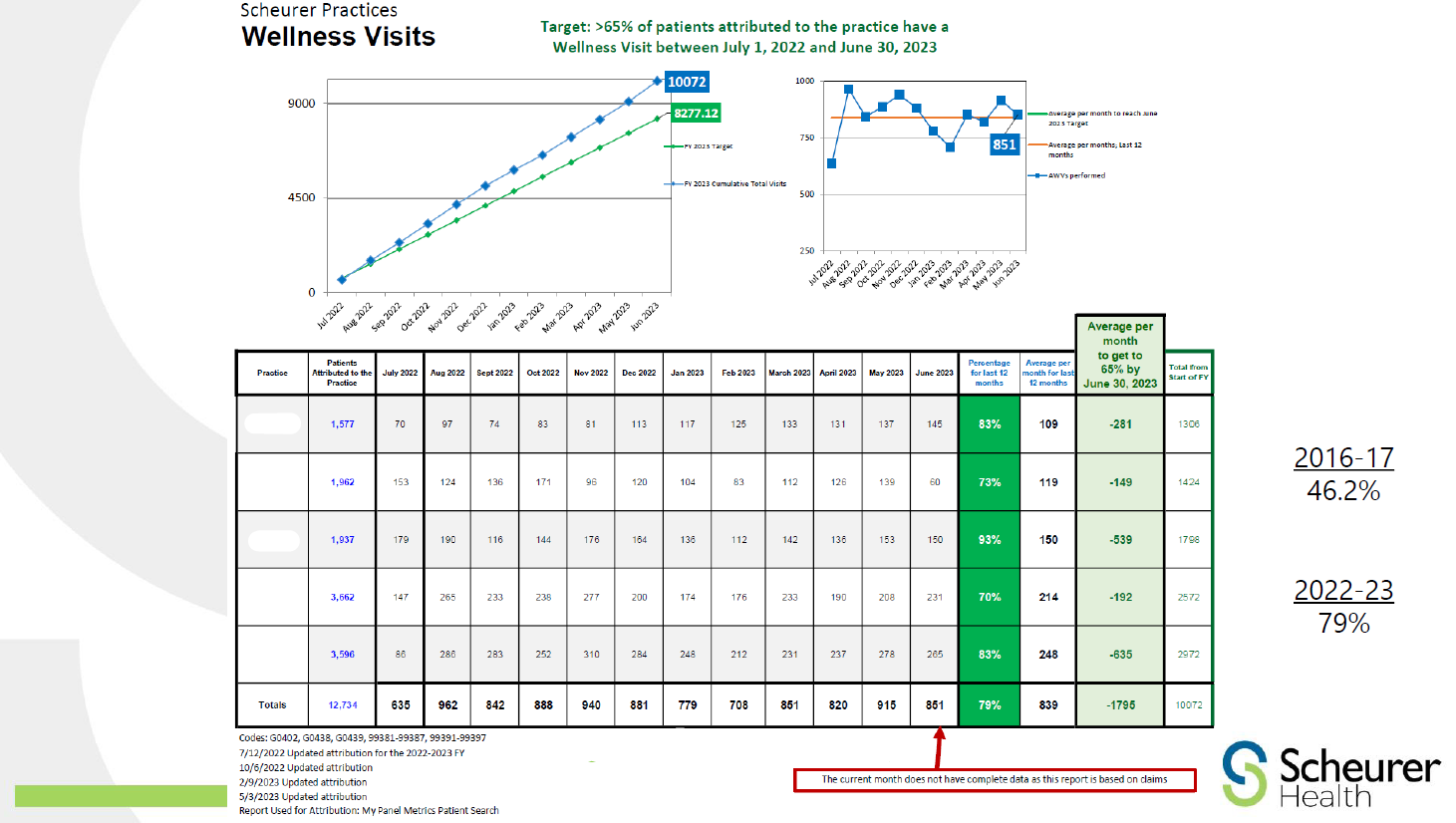
Following the unblinded data session, Ross Ramsey, MD, CPEM, FAAFP, President and Chief Executive Officer of Scheurer Health, delivered a presentation on common rural health challenges and Scheurer Health’s recent efforts to improve the quality of care for its rural population. Dr. Ramsey emphasized that rural areas are associated with higher poverty rates, larger proportions of elderly individuals, a higher percentage of patients who are uninsured, and a higher prevalence of chronic health problems such as substance abuse and illnesses related to environmental exposures. Dr. Ramsey highlighted several focus areas at Scheurer Health to improve the value of care for its patients: wellness visits, transitional care management, remote patient monitoring, and ED follow up. As seen in Figure 3, Scheurer Health increased wellness visit participation by 32.8% over the last six years. For more details about Scheurer Health’s strategies and success stories, view Dr. Ramsey’s slides here.
Figure 3.
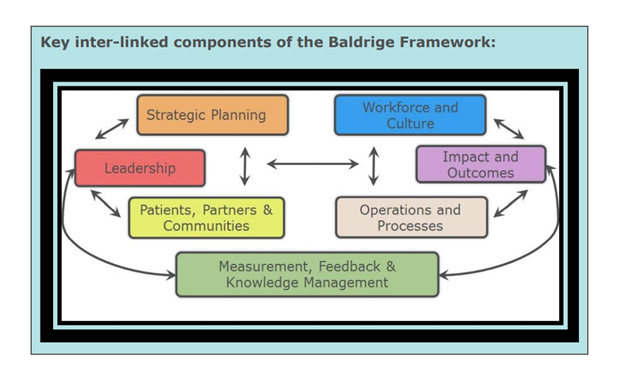
After Dr. Ramsey’s insightful presentation, MVC welcomed Mariah Hesse, MSN, CENP, President of the Michigan Critical Access Hospital Quality Network (MICAH QN) and Chief Nursing Officer at Sparrow Clinton Hospital. Her presentation (see slides) provided an overview of core components of the quality network, highlighting its foundational pillars of success (Figure 4), in addition to featuring the network’s accomplishments and the benefits of participation by Michigan’s 37 CAHs. MICAH QN ensures representation for CAHs on national and state committees and serves as a resource to Michigan CAHs on performance improvement tools and measures. Her presentation also referenced several key priorities for healthcare in rural Michigan, such as meaningful benchmarking focused on outpatient care, recovery from challenges experienced during the pandemic, and improving healthcare access and equity.
Figure 4.
MVC looks forward to continued partnership with members based in rural communities to support the delivery of sustainable, high-value care through high-quality data analytics, collaboration, and innovation.
The slides from Wednesday’s meeting have been posted to the MVC website and a recording of the meeting is available here. If you have questions about any of the topics, contact the MVC Coordinating Center. MVC’s next collaborative-wide meeting will be in person on Friday, October 20, 2023, in Lansing, MI.