In June, MVC hosted two virtual workgroup presentations – the first, a cardiac rehab workgroup focused on how healthcare organizational structures impact the effectiveness of cardiac rehab operations. The second workgroup, health in action, was a continuation of the recent MVC spring collaborative-wide meeting (CWM) presentation and discussion on How Should We Measure System Quality? The MVC Coordinating Center hosts workgroup presentations twice per month, covering a variety of topics including post-discharge follow-up, sepsis, cardiac rehab, rural health, preoperative testing and health in action.
Cardiac Rehab Workgroup June 10, 2025
MVC hosted a cardiac rehab workgroup with a presentation by Gregory Scharf, BS, ACSM-CEP, AACVPR-CCRP from MyMichigan Health System. Scharf is the Cardiopulmonary Rehab System Manager for nine cardiac rehab and eight pulmonary rehab programs that serve 25 counties in Michigan. In addition to his role with MyMichigan, Scharf is also the vice president of the northern region of the Michigan Society for Cardiovascular and Pulmonary Rehabilitation (MSCVPR). With his experience and knowledge, Scharf shared detailed insight into how healthcare organizational structure impacts the effectiveness of cardiac rehabilitation operations.
Organizational Structures & Impact
Many cardiac and pulmonary rehabilitation programs experience disjointed connections within healthcare organization structures. According to a recent MSCVPR state poll, up to 20% of the state’s cardiac rehab (CR) programs were structured under a non-cardiovascular related service. Scharf polled the MVC workgroup audience to see where their cardiac rehab programs fell within their organizational structure and found that out of the 21 responses, 11 sites had their CR program under Cardiology/Cardiovascular service, three under respiratory service, four under cardiopulmonary service, one under diagnostic imaging, one under cardiovascular/neurology, and one did not have an onsite CR program.
Scharf noted that in his experience, many of the structures and managerial roles of cardiac rehab programs varied across sites. Cardiac rehab managers included an obstetrics/emergency room nurse manager, physical therapy manager, respiratory services supervisor, and a cardiovascular services manager who was also the echocardiogram technician. The lack of consistency in who should manage a cardiac rehabilitation program adds to the challenges within the healthcare organizational structure.
Supporting Cardiac & Pulmonary Rehab Programs
How can cardiac rehab be strategically aligned within a system? Main organizational connections for CR programs can be successful if placed under the umbrella of cardiovascular services (testing, heart failure clinic, open heart surgery, structural heart surgery, electrophysiology, and vascular), and rehabilitation services (occupational/physical therapy, etc.). Misalignment may occur if the organization’s strategies and objectives are disconnected between service areas, for example:
- Communication breaking down across the system
- Advocates for the CR service lack authority for change
- There are conflicts between service resources and access to space based on organizational leadership structure (OT/PT/CR)
A challenge for smaller sites may be that their organization is not large enough to support the typical structure of large health systems. At MyMichigan the CR program functions with 30 clinical staff for all sites whereas PT has more than 1,000 clinicians. These kinds of discrepancies may cause programs like cardiac rehab to be placed under misaligned service structures due to convenience (staff availability, resource availability) versus a more appropriate setting.
Important questions to ask about your site’s cardiac rehab program structure:
- Who is responsible for your cardiac rehab operations?
- Are they responsible for non-cardiac rehab departments as well?
- Who are the cardiac rehab subject matter experts (SME) and do they have authority to make changes?
SMEs may vary in experience and knowledge, especially when looking at smaller healthcare sites. These SMEs may only have secondary or limited experience with cardiac rehab services, which can impact how successful the program is. One way to help support staff in these positions is to encourage continuing education programs and certifications related to cardiac rehabilitation.
Understanding the Anatomy of the Referral
Over the past 10 years, MyMichigan has seen a significant increase in referral rates for cardiac rehab. Unfortunately, an increase in referrals does not always equate to an increase in patient participation. Some examples of why this may happen include referral delays, missing referral information (no qualifying diagnosis, or no co-signing MD/DO), or a referral being sent with the patient information but no signed order (inactionable).
Figure 1. Common Referral Delay Examples

When referrals are completed incorrectly, CR program staff must do the leg work to reconnect with the referring provider and make sure they receive a complete referral for their patient. MyMichigan faxes a Cardiac Rehabilitation (CR) Referral & Evaluation Order back to the referring provider to complete and return before the patient can be seen for cardiac rehab. This extra step can impact patient recovery and create added strain on the workforce for multiple healthcare sites.
MVC Data Analytics Resources & Support
Wanting to take a deeper look at cardiac rehab claims data, MyMichigan Health System collaborated with the MVC team including Emily Bair, Site Engagement Coordinator, Julia Mantey, Sr. Data Analyst, and Jiaying Zhang, Data Analyst. The MVC analysts created custom reports that helped visualize where MyMichigan’s CR patients were being referred to and which patients were being referred to their CR program from external sites.
Looking at MyMichigan sites they found that approximately 94% of the patients that discharged from the MyMichigan Midland Medical Center for any of the Michigan Cardiac Rehab Network (MiCR) Main five Conditions (AMI, PCI, CABG, SAVR, TAVR) ended up staying within the MyMichigan system cardiac rehab program. Additionally, they looked at what locations MyMichigan cardiac rehab patients come from across the state. Approximately 58% of CR patients are internal referrals and 41% are from external referrals, almost doubling patient population in MyMichigan’s cardiac rehab program. This also put a spotlight on how much this system’s cardiac rehab program impacted patient populations of external healthcare sites/systems in the state.
Key Take Aways
- What internal barriers exist due to your organizational structure?
- Is communication getting to those that impact change?
- Understand what steps need to be completed between referral and scheduling the patient appointment
- Understand the process for referrals that leave the system/site
June 10, 2025, Cardiac Rehab Workgroup
Health in Action Workgroup 6.26.25
In late June MVC Director Hari Nathan, MD, PhD presented on how quality could be measured at a system level. This was a continuation from his interactive presentation at our spring CWM earlier this year, How Should We Measure System Quality? This “Part 2” workgroup included breakout groups and focused topics for discussion.
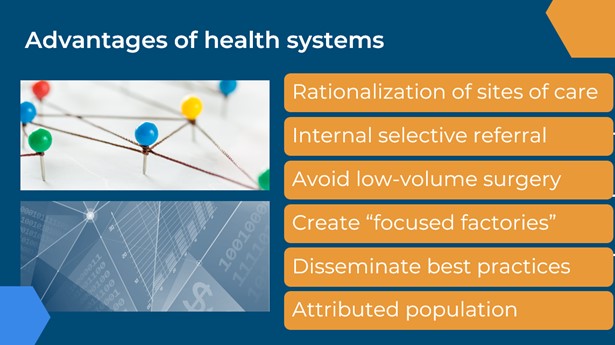
Advantages of Health Systems
Dr. Nathan shared several advantages that health systems have in the world of quality improvement that could be utilized, such as being able to right-size care and services at sites, having internal selective referrals as an option, avoiding low-volume surgeries, creating “focused factories,” disseminating best practices, and being able to have a big impact on attributed populations.
Health systems have the ability to address barriers to care on a larger scale, for example improving electronic health record integration between sites and being able to integrate telehealth across the system. Or by collecting data on various patient populations, a system has the potential to develop and expand its population health program. Utilizing the strengths of a system can benefit individual healthcare sites and improve patient care.
It is important to begin challenging systems to become more than just a sum of their parts – rather, to function as a cohesive unit. How do we create the right incentives for hospital systems to improve quality and costs? What metrics should be measured? These are just a few of the questions posed by Dr. Nathan as the workgroup audience prepared to go into breakout session discussions.
At MVC’s spring CWM in May of this year, audience members were asked “What is your organization doing at a system-level that you would want to be measured on and/or receive credit for improving?”. The most popular responses included: CMS 5 Star Measures, balancing length of stay (LOS) and readmissions, infection prevention, and sepsis outcomes (LOS, readmissions, mortality/end of life care).
Based on the CWM responses, four breakout session topics were chosen (readmissions & balancing LOS, safety, infection prevention, sepsis outcomes), and participants were asked to think about and discuss “What is YOUR organization working on at a system level that you would want to be measured on and/or receive credit for improving?”. Based on their poll responses, participants were sent into breakout groups to discuss their topic more in depth.
Readmissions & Balancing LOS
Members expressed great interest in identifying opportunities to incentivize process measures. Currently tracked metrics that were shared included order set utilization, care coordination, evaluating daily readmission risk reports, and transitions to home care. It was noted however, that these metrics may be difficult to track via claims data. Another system-wide metric discussed was the percentage of patients being seen by their primary care physician one week post discharge. The measure of success could be either achievement (outperform MVC All) or improvement (improve on system metric compared to previous measure).
Some barriers to implementing these processes as a system would be system-wide financial support for care coordination and nurse navigators. These positions are typically site specific and funded through the site’s individual budget.
Safety
During this breakout session members discussed some of the interests their sites/systems had around tracking safety metrics across the system. Sometimes a system can be different than just multiple hospitals under the same umbrella. Oaklawn Hospital, for example, is a single hospital site, but their goal is to align better with their primary care offices which requires a systems approach.
When looking at safety measures, Henry Ford Health shared ideas on how measuring or tracking a patient’s nutritional status might be valuable, as well as physical or occupational therapy consults for falls. Patients with a hip fracture from a fall tend to have longer hospital stays, this could be tracked by LOS codes such as weakness or loss of balance.
Infection Prevention
Members discussed some of the successful methods they have been implementing so far with their infection prevention initiatives. ProMedica Charles & Virginia Hickman shared they use a hub and spoke model where the sites have a system level clinical risk department that helps oversee essential hospital acquired infection data (using PowerBI, a data visualization program). This program enables a drill down for the different hospital leaders to design and implement quality improvement initiatives at their site.
At the system level leaders review data to identify opportunities and coordinate with hospital quality leads to implement improvement strategies, maintaining an upstream and downstream approach. In the UP Health system, they use a collaborative model involving regular reporting and discussion of quality markers among hospitals under the LifePoint organization, with resource sharing and active discussion facilitated by calls that include Duke University Health System partners.
Sepsis Outcomes
Members shared that their health systems have hospital level sepsis committees that meet once per month to review sepsis cases, as well as system level sepsis committees that include a representative from each site that meet monthly or quarterly to review sepsis cases. One of the ways that members are tracking their sepsis cases across the system is by tracking when sepsis patients go from “door to initial antibiotic received,” since research has shown this to be the biggest impact on reducing sepsis related mortality.
Sepsis compliance is also an important metric that systems are tracking to meet CMS standards. Sites within a system track sepsis compliance metrics and review them monthly both site by site and system wide. Through the group discussion, the idea of tracking the associated order sets for sepsis cases through MVC claims data may be interesting to view at a system level (though singling out order sets in claims data may be difficult).
June 26, 2025, Health in Action Workgroup
Wrap Up
The breakout sessions not only helped to highlight what health systems are currently doing to track quality across their sites but also gave some insight into what metrics could be utilized as performance-based incentives in the future.
MVC welcomes workgroup presenters from across Michigan to share their expertise, success stories, initiatives, and solution-focused ideas with MVC members. Please reach out to us by email if you are interested in being a workgroup presenter or submit a presentation proposal here.