MVC members will receive their next batch of updated push reports in the coming days with a refreshed version of MVC’s common conditions report. These reports provide insight into episodes of care for eight medical and surgical conditions that are commonly a focus for quality improvement efforts at MVC hospitals: acute myocardial infarction (AMI), chronic obstructive pulmonary disease (COPD), colectomy (non-cancer), congestive heart failure (CHF), coronary artery bypass graft (CABG), total knee and hip (joint) replacement, pneumonia, and spine surgery. MVC’s general acute care hospital and Critical Access Hospital (CAH) members will receive tailored versions of the report, with each group receiving benchmark data specific to their own category of hospitals.
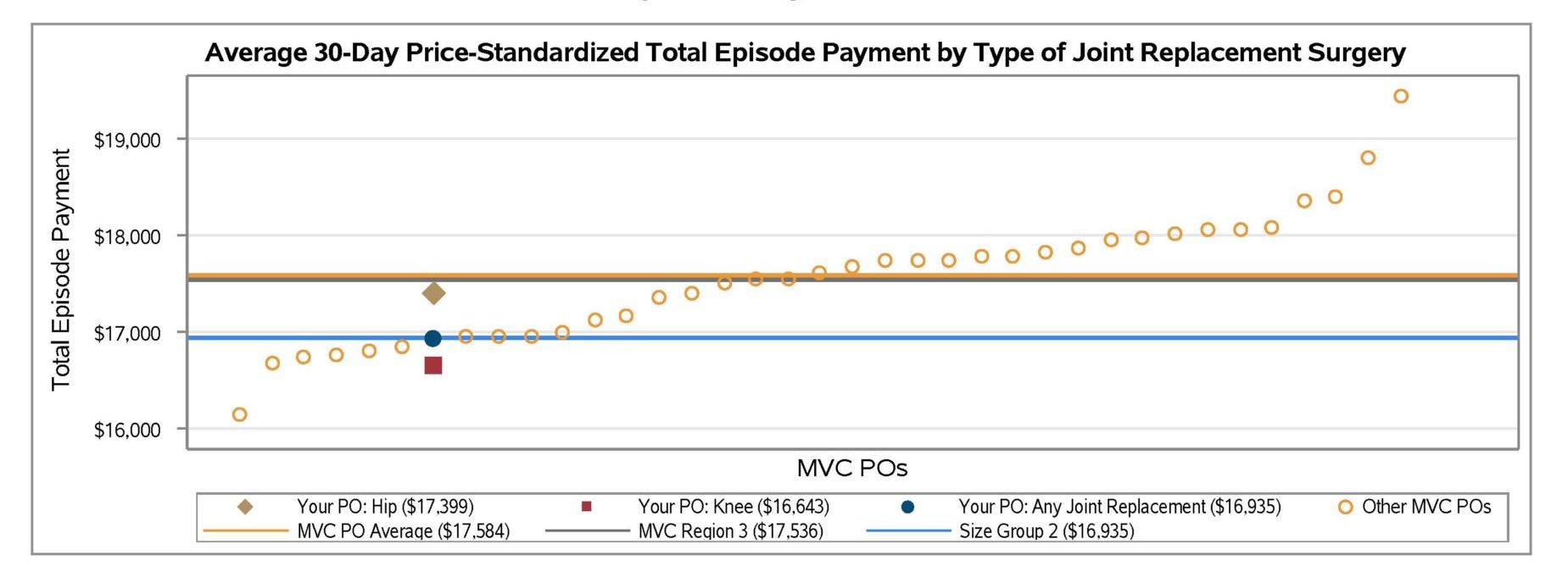
Although the metrics provided vary by condition and case count, report pages generally focus on 30-day total episode payments, readmission rates, common reasons for readmissions, and post-acute care utilization. MVC price standardizes total episode payments to Medicare FFS amounts so that comparisons can be made across hospitals and over time. Payments are risk adjusted for patient age, gender, payer, comorbidities, and high or low prior healthcare utilization/payments.
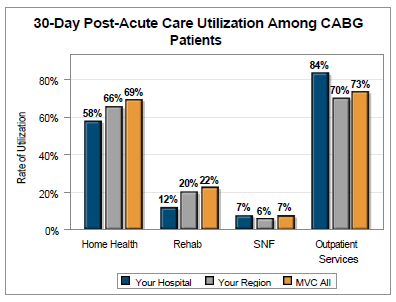
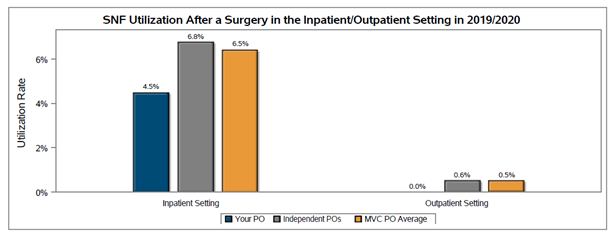
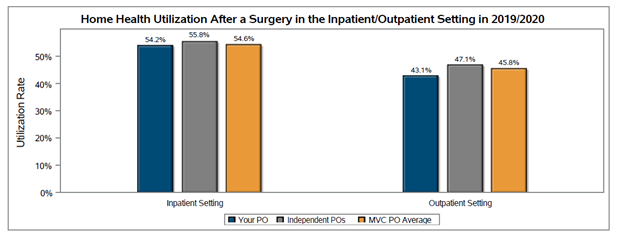
Post-acute care utilization benchmarking for each of the eight medical and surgical conditions includes graphs displaying the percentage of each hospital’s patients who used home health care, inpatient/outpatient rehab, skilled nursing facility care, outpatient services, or emergency department care in the 30 days following their index hospitalization or surgery. Across the collaborative, reports show high use of 30-day home health care and outpatient services for these common conditions. For patients initiating their episode of care at a general acute care hospital within the collaborative, the home health care utilization rate was highest following CABG (69%) and joint replacement (50%).
Patients with a CABG episode were also high utilizers of outpatient services in the 30 days post-index (Figure 1), with a 73% average utilization rate. Patients with episodes for CHF (58%) and AMI (53%) were also high utilizers of outpatient services. Across conditions, use of outpatient services in the 30 days post-index was generally higher among episodes originating at CAHs than among episodes originating at general acute care hospitals.
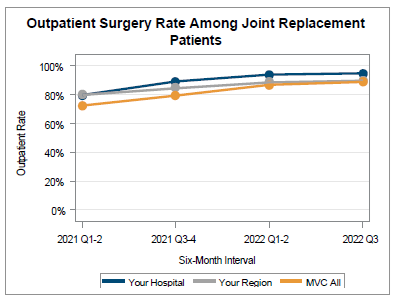
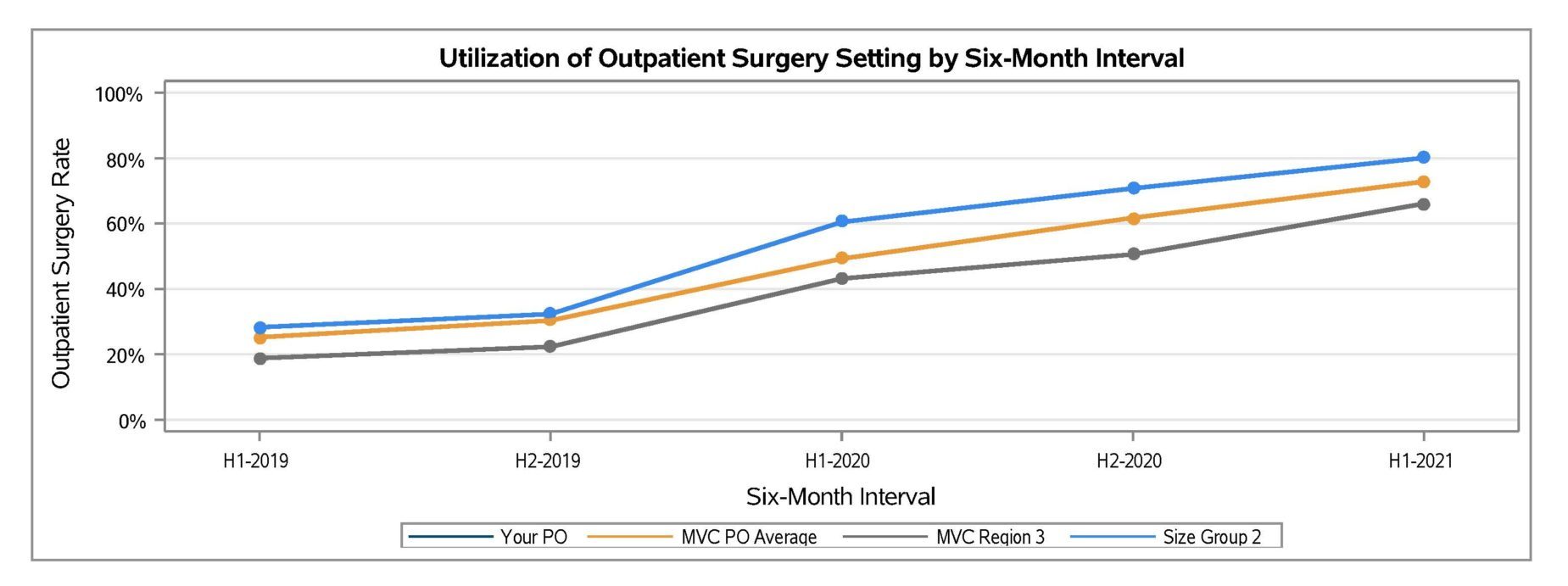
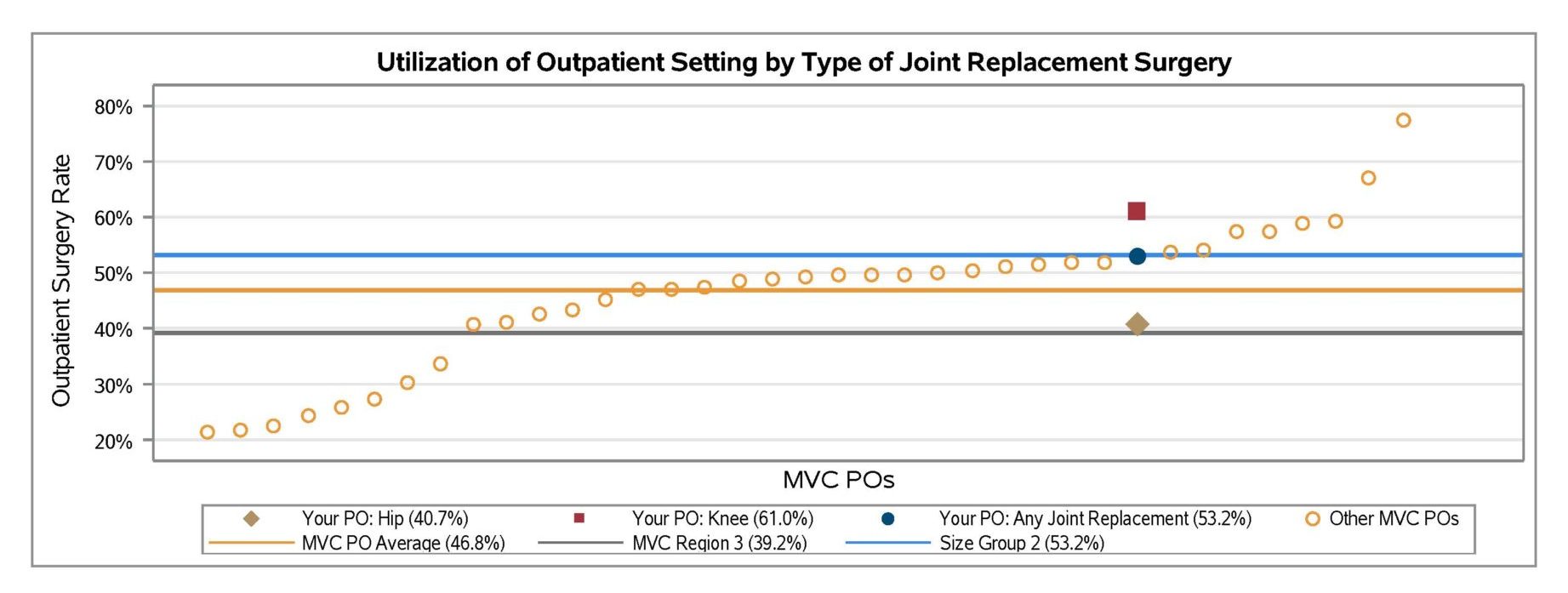
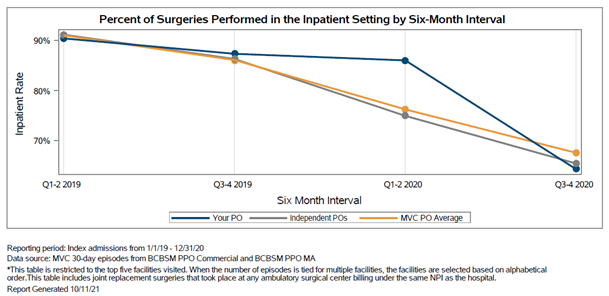
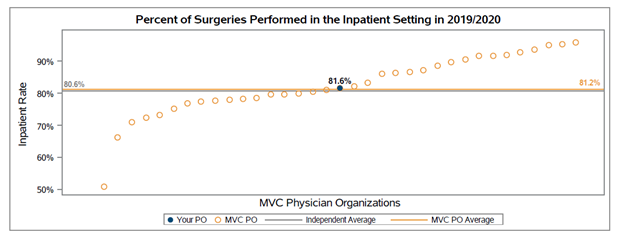
Reports also assess the setting of care for joint replacements and spine surgeries. For total knee and hip replacements, MVC data shows that the percent of joint replacements performed in an outpatient setting at general acute care hospitals across Michigan continued to rise from January 2021 through September 2022 (Figure 2).
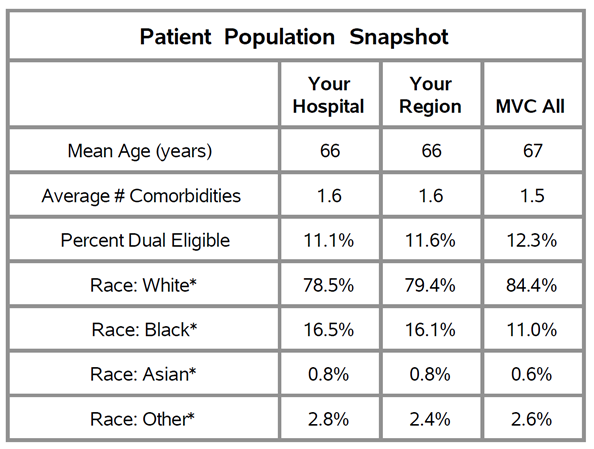
The patient population in these reports comprises adult patients who had surgery or an inpatient hospitalization at an MVC-participating hospital between January 2021 and September 2022. Measures are based on 30-day inpatient and surgical-based episodes of care data, incorporating paid claims from Blue Cross Blue Shield of Michigan and Blue Care Network Commercial and Medicare Advantage plans as well as paid claims from Medicare Fee-for-Service. Episodes meeting any of the following criteria were excluded from calculations: patients transferred to another acute care hospital or to hospice, patients who died during their index stay, and patients with a primary diagnosis of COVID-19 received in an inpatient setting at any point during their 30-day episode.
We hope our collaborative participants find these reports valuable, and as always, we welcome MVC members to contact MVC with any questions or analytic requests.