The Michigan Value Collaborative distributed refreshed sepsis push reports this week, providing its hospital members with updated figures and measures using the latest MVC episode data. In addition, the latest reports were also distributed to members of the Michigan Hospital Medicine Safety Consortium (HMS), a valued partner in the initial development of this service line within MVC's registry.
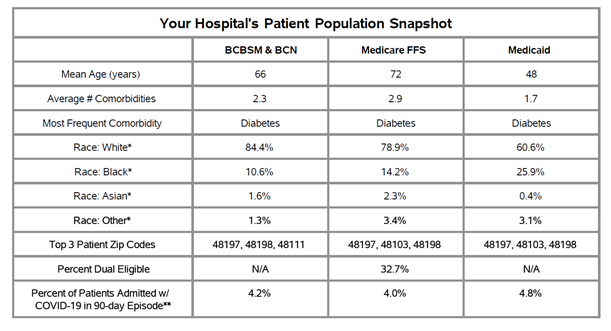
This week’s reports included MVC’s updated race and ethnicity categories, which were modified and expanded to ensure greater inclusivity and accuracy. MVC also recently adopted a methodological change to its identification of patients admitted with COVID-19 that impacted the episode data used in this analysis. MVC episodes were flagged as containing significant COVID-19 care if a COVID-19 diagnosis (U07.1) was found in the primary diagnosis code position on a facility claim during the 90-day episode. Previously, MVC looked for COVID-19 diagnosis in the first three diagnosis code positions. These episodes are often excluded from MVC’s push reports but have historically been included in sepsis reporting to help hospitals gauge the impact of COVID-19 diagnosis on their sepsis metrics. Combined with the natural decline in disease prevalence, there was a significant reduction in the percentage of patients with a COVID-19 diagnosis who were treated for sepsis, compared to the previous reporting period.
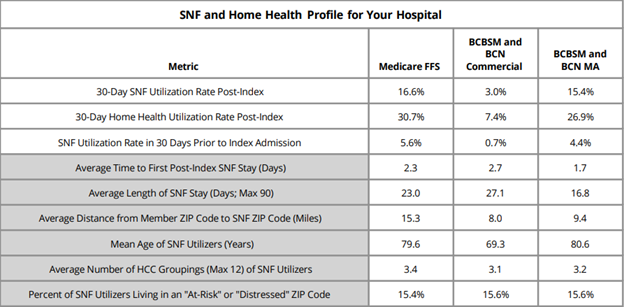
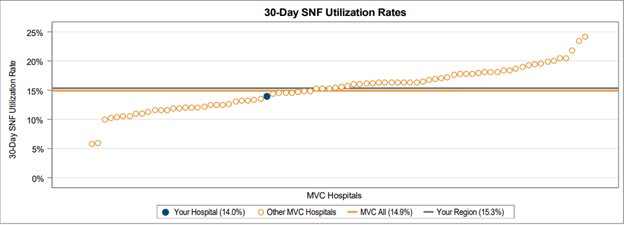
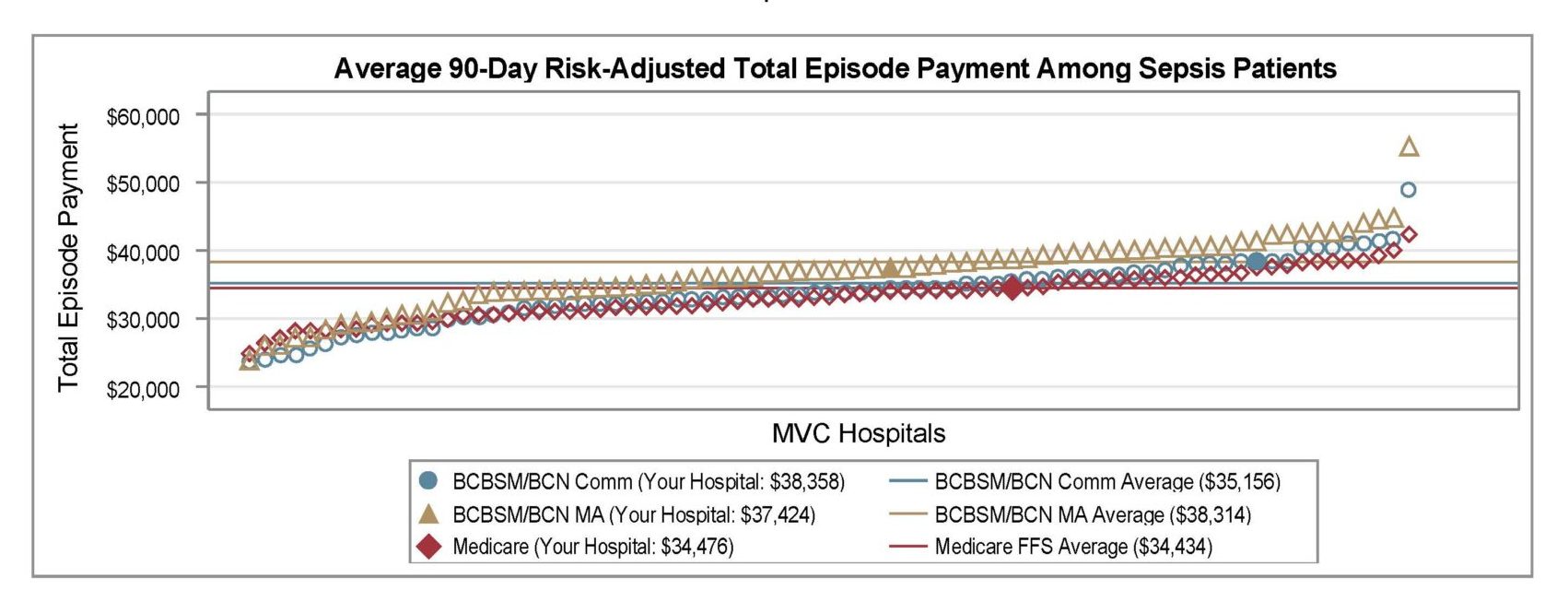
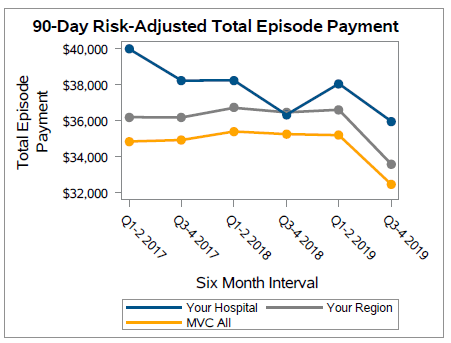
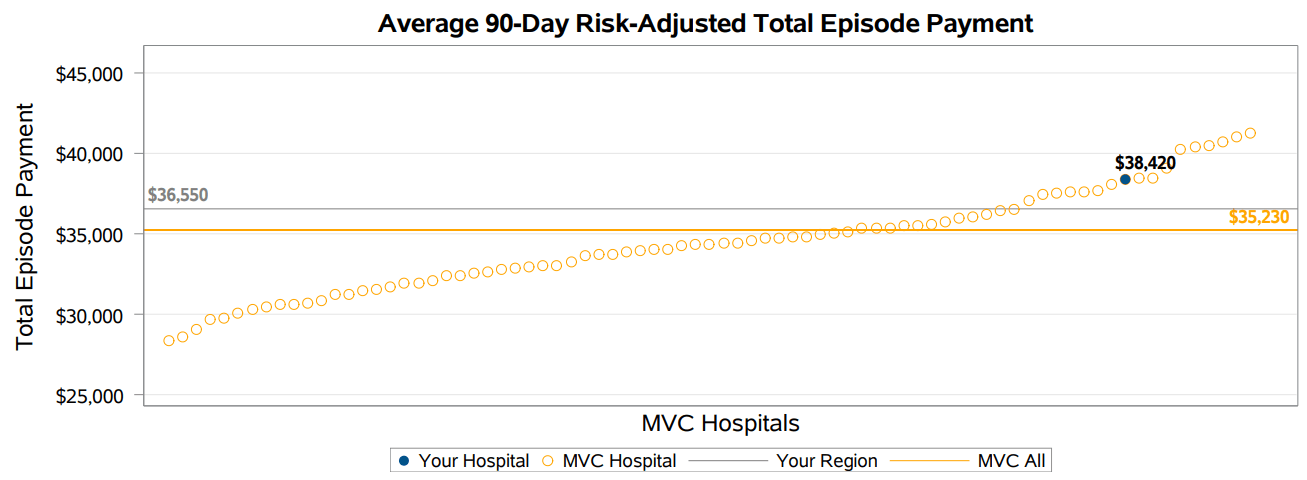
The version shared with MVC members this week continued to provide price-standardized, risk-adjusted benchmarking for total episode payments, as well as length of inpatient stay, Intensive Care Unit (ICU)/Cardiac Care Unit (CCU) utilization, inpatient mortality or discharge to hospice, 90-day post-acute care utilization, and 90-day readmission rates. MVC’s general acute care hospital (GACH) and Critical Access Hospital (CAH) members were provided with tailored versions using comparison groups most suitable to their hospital category.
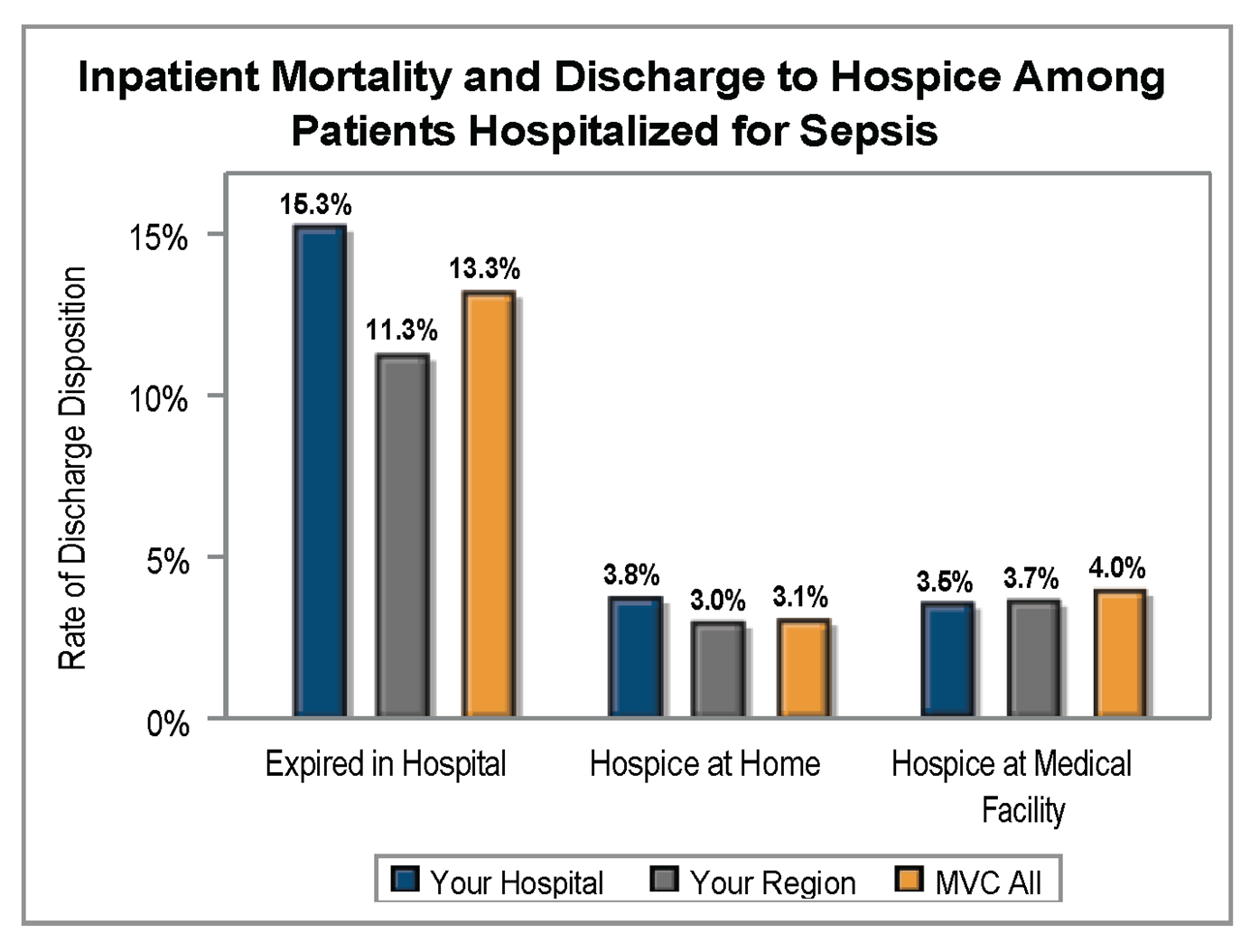
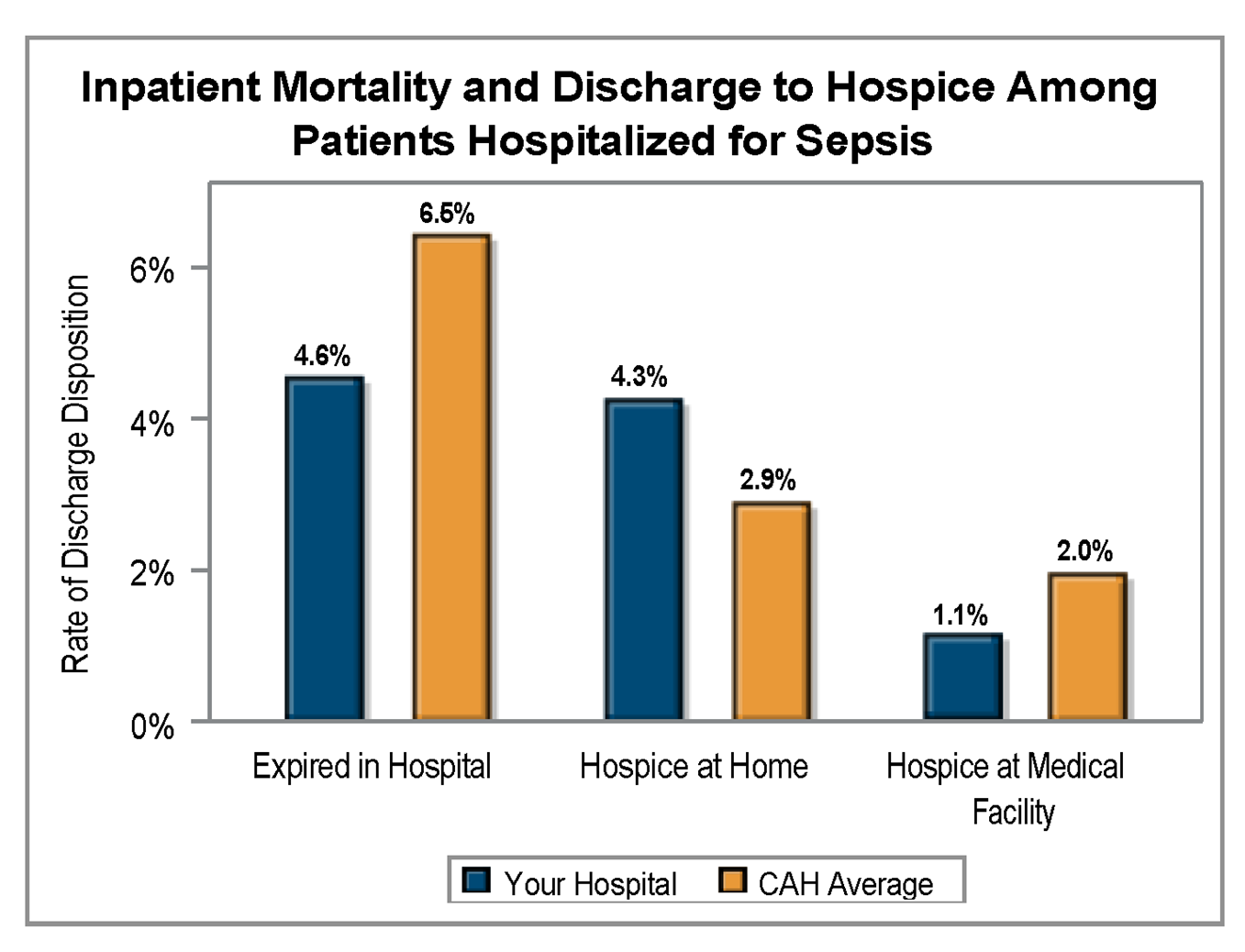
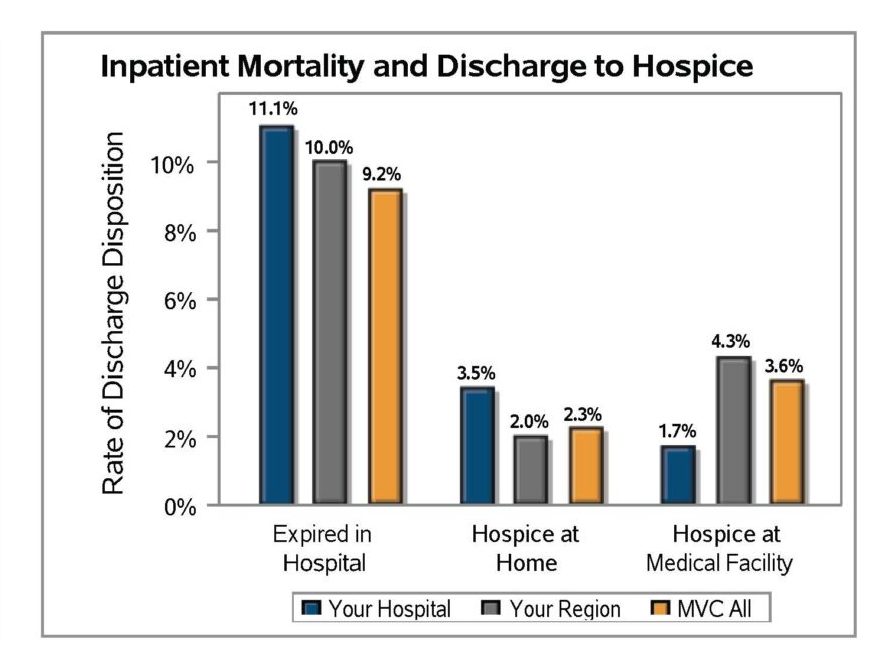
Sepsis is currently the third leading cause of death in U.S. hospitals, so inpatient mortality and discharge or hospice were included in MVC’s sepsis reports as important quality checks. The average inpatient mortality rate among patients hospitalized for sepsis was 13.3% across member GACHs (Figure 1) and 6.5% for CAHs (Figure 2). Rates for discharge to hospice at home or a medical facility were lower.
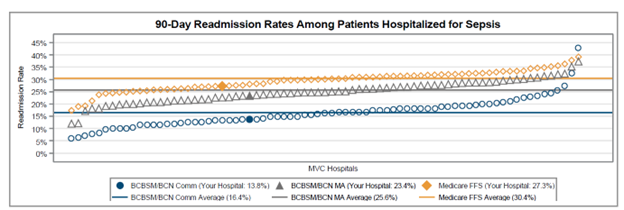
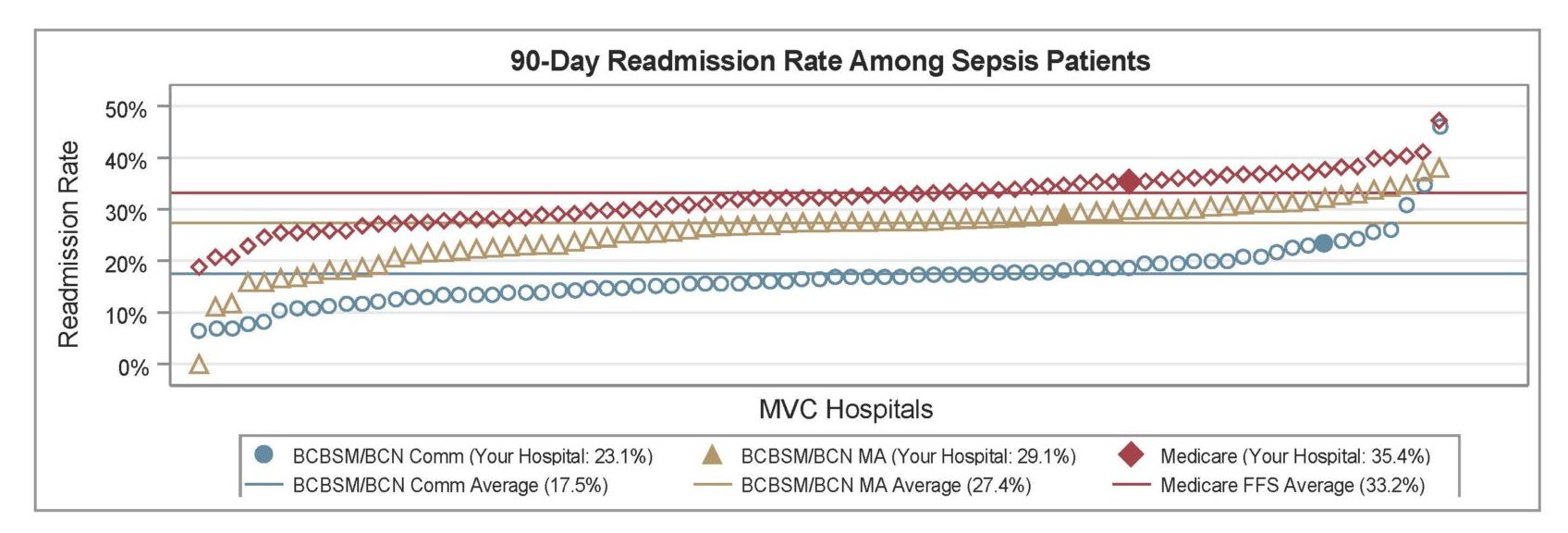
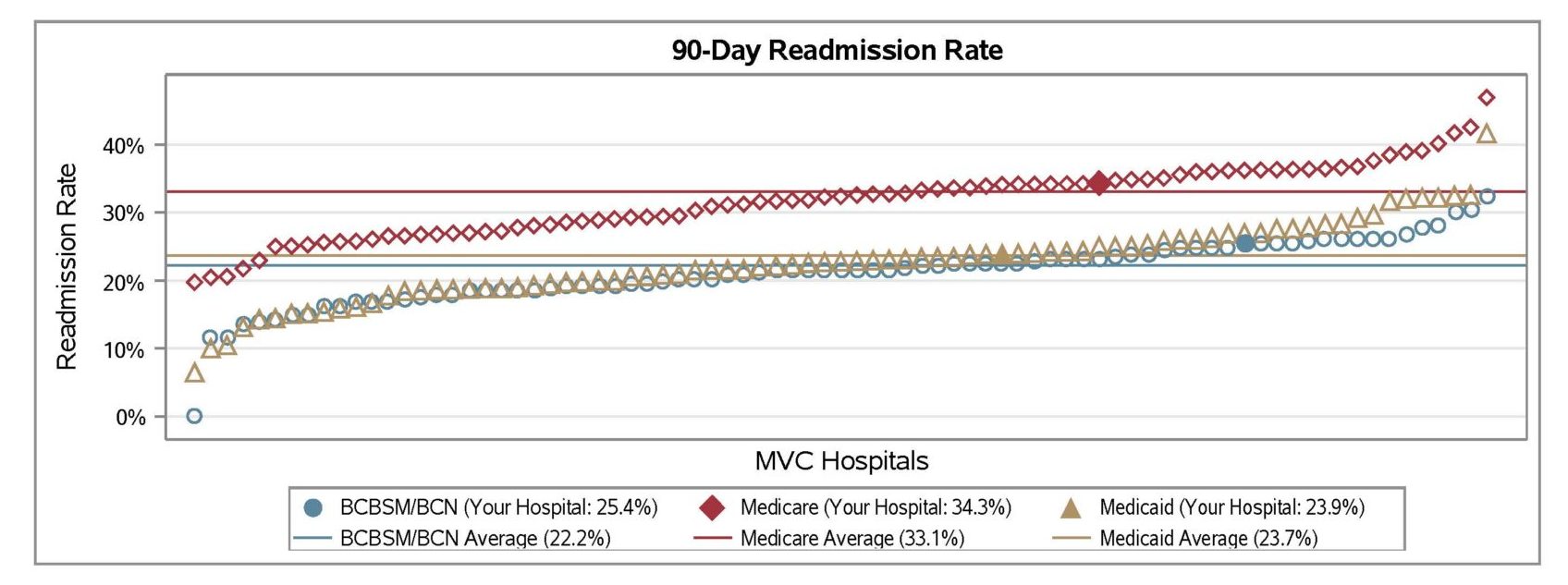
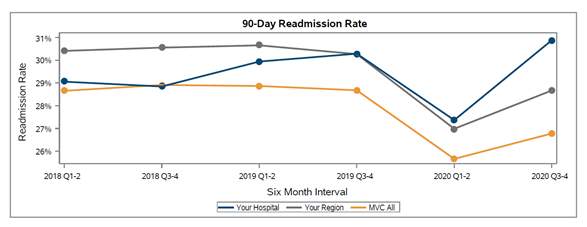
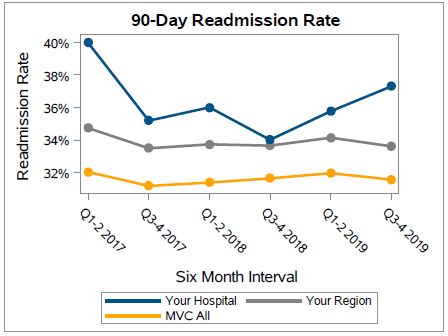
The latest report also investigated differences in 90-day readmission rates for patients hospitalized for sepsis. Within GACH, patients with Medicare FFS coverage exhibited the highest average readmission rate (30.4%), followed by patients insured by BCBSM/BCN MA plans (25.6%) and BCBSM/BCN Commercial plans (16.4%), respectively (Figure 3). BCBSM/BCN Commercial patients had a younger average age and lower average comorbidity count than patients with Medicare or MA plans. Within CAHs, the average 90-day readmission rate was 22.4%.
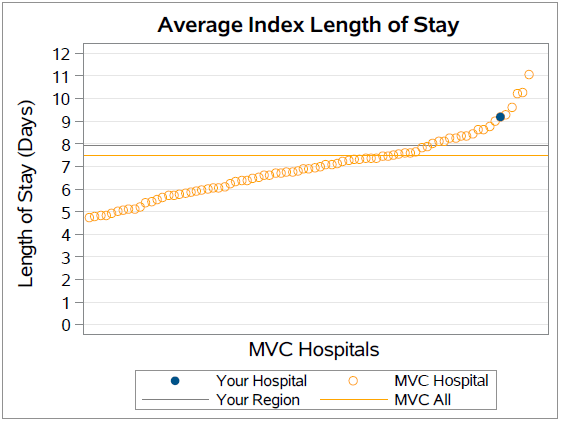
The report also included benchmarking for average index length of stay by specific payer groups as well as for all payers combined. The average index length of stay across all payers was 8.7 among GACH patients and 5.5 among CAH patients.
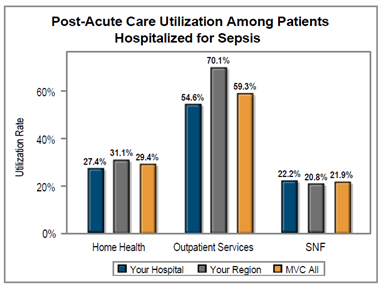
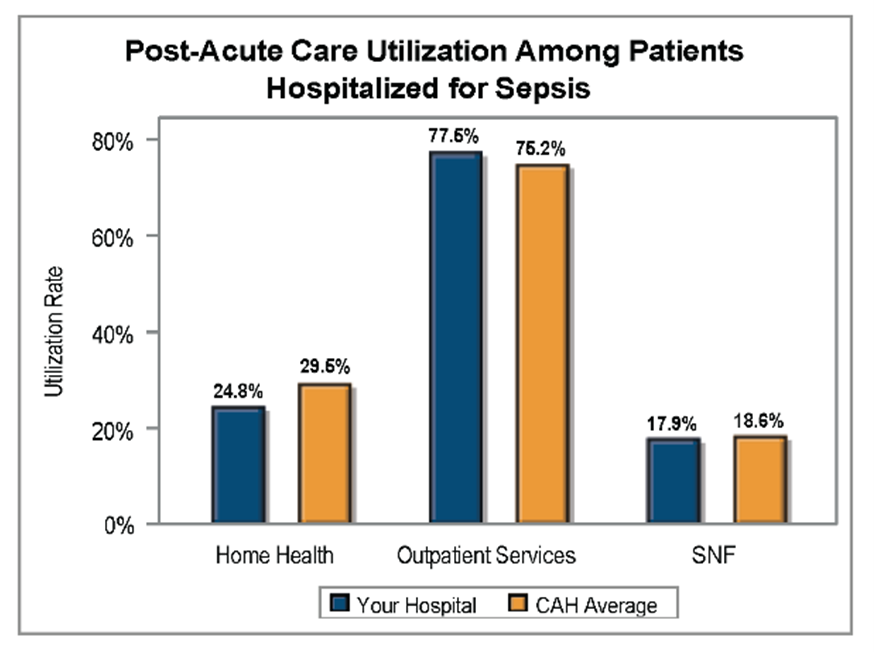
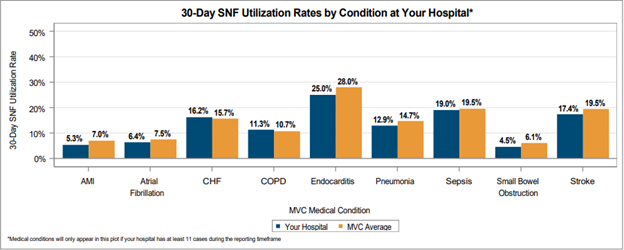
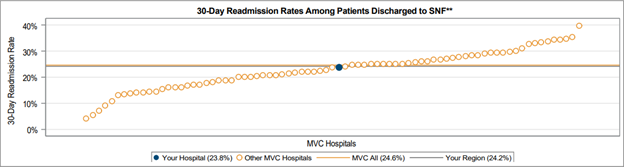
Another significant finding was the difference in post-acute care utilization by service type among patients hospitalized for sepsis (Figure 4). On average across GACHs in the collaborative, outpatient services had a noticeably higher utilization rate (59.3%) compared to home health (29.4%) or skilled nursing facility (21.9%). The same was true for CAHs (Figure 5), with a much higher average utilization rate for outpatient services (75.2%) compared to home health (29.5%) or skilled nursing facilities (18.6%).
These reports were prepared using 90-day MVC episode data with index admissions from 7/1/19 – 6/30/22 for the following insurance plans: Medicare Fee-For-Service (FFS), Blue Cross Blue Shield of Michigan (BCBSM) PPO Commercial, Blue Care Network (BCN) Commercial, BCBSM PPO Medicare Advantage (MA), and BCN MA.
MVC welcomes your recommendations for enhancing these reports and welcomes your feedback on how collaborative members are using these data to support their quality improvement efforts. Please don't hesitate to contact the MVC team at Michigan-Value-Collaborative@med.umich.edu.