In November, MVC hosted two virtual workgroup presentations – the first on preoperative testing was led by a fellow Collaborative Quality Initiative (CQI), and the second on cardiac rehabilitation was delivered by an MVC member hospital. MVC hosts two virtual workgroups per month with topics rotating between post-discharge follow-up, sepsis, cardiac rehabilitation, rural health, preoperative testing, and health in action (ad hoc focused topics). Each month, the MVC Coordinating Center publishes key highlights from these presentations to support resource and best practice sharing across the state.
November Preoperative Testing Workgroup: Michigan Surgical Quality Collaborative (MSQC)
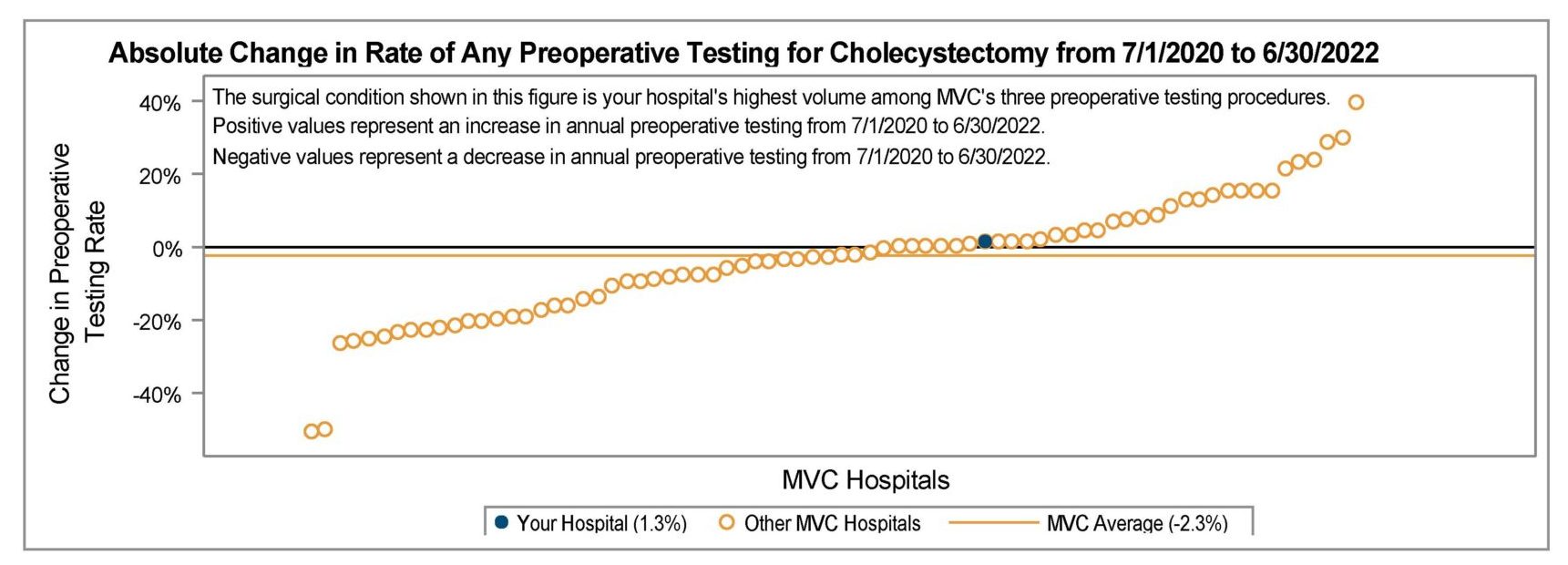
The first workgroup of November focused on preoperative testing and featured a presentation by Pamela Racchi, Clinical Site Coordinator with the Michigan Surgical Quality Collaborative (MSQC), and Susanna Fortney, Clinical Quality Specialist at ProMedica Charles and Virginia Hickman Hospital. To start, Racchi’s presentation provided an update on MSQC’s Preoperative Testing for Low-Risk Surgeries Project, including updated findings for 2024 and plans for 2025. Fortney then presented on ProMedica Charles and Virginia Hickman’s progress with reducing preoperative testing through the lens of participating in both the MSQC preop testing project and the RITE-Size pilot.
MSQC’s preoperative testing project is a continuation of a pilot started in 2022. The goals of the project include:
- To define the extent of routine preoperative testing in low-risk surgeries,
- To identify underlying reasons for overuse of preoperative testing in low-risk surgeries, and
- To implement interventions to heighten awareness and reduce variation among hospitals
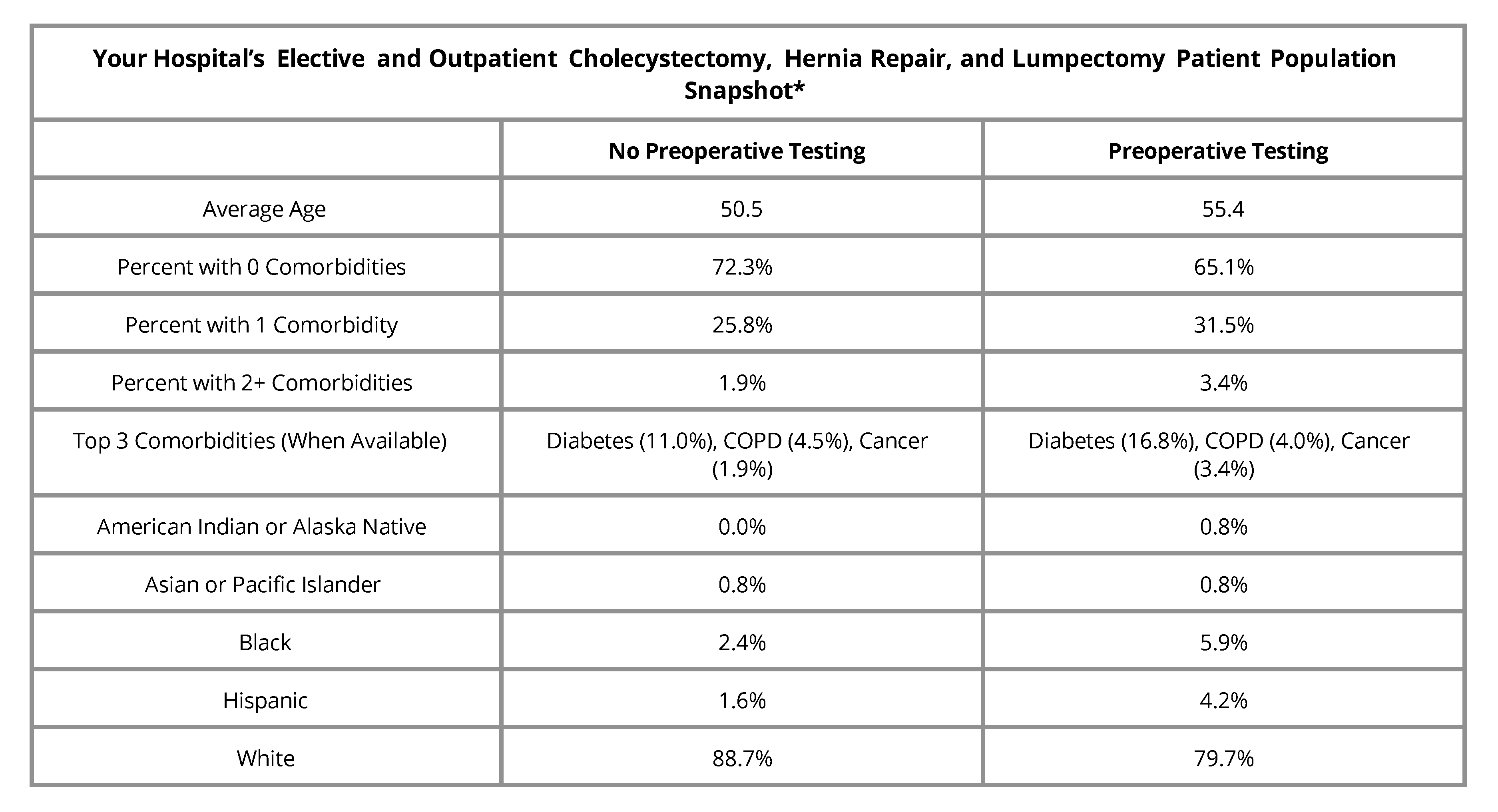
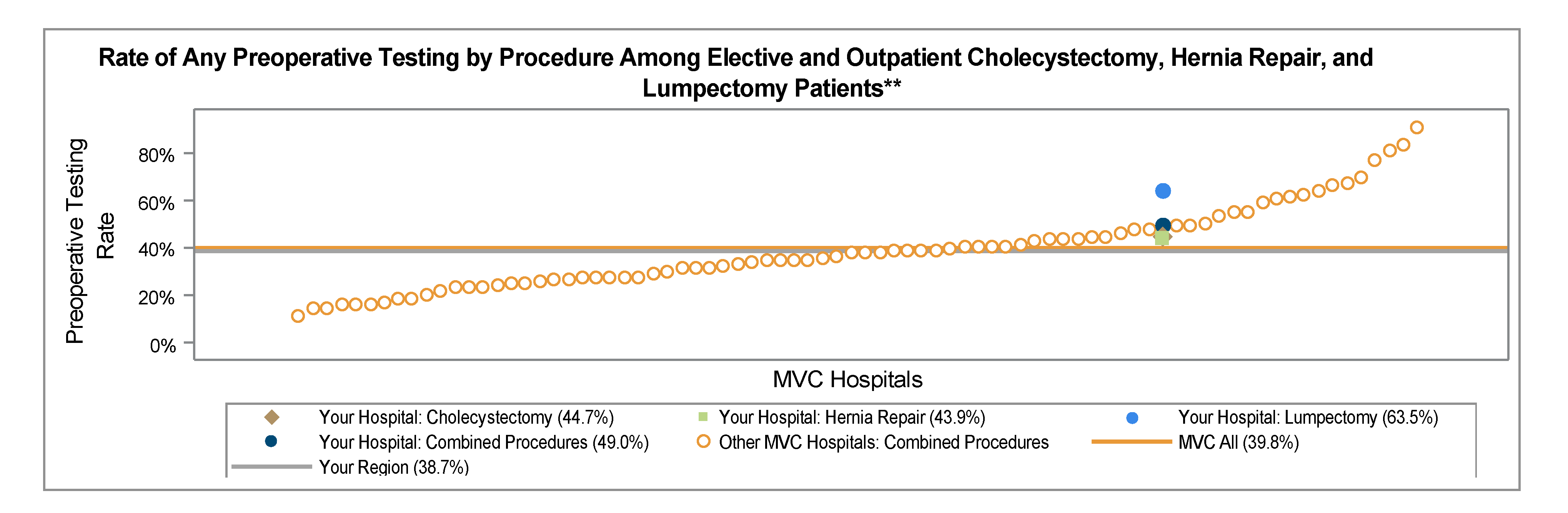
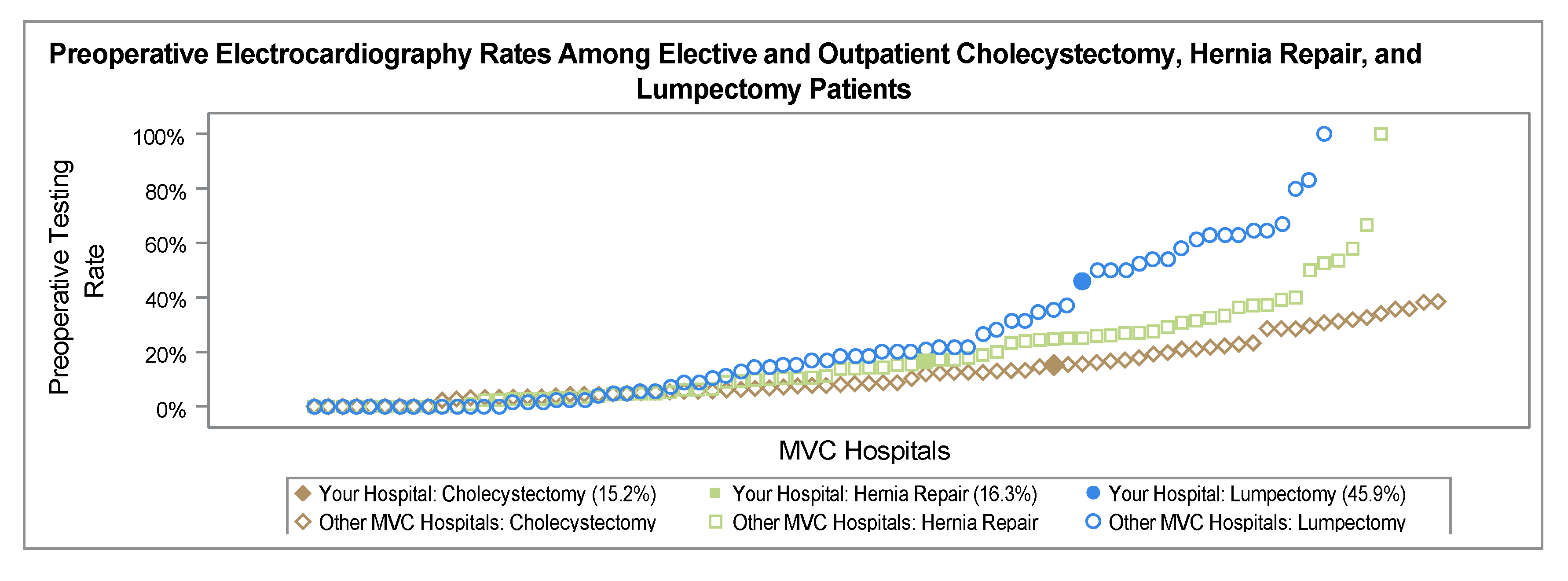
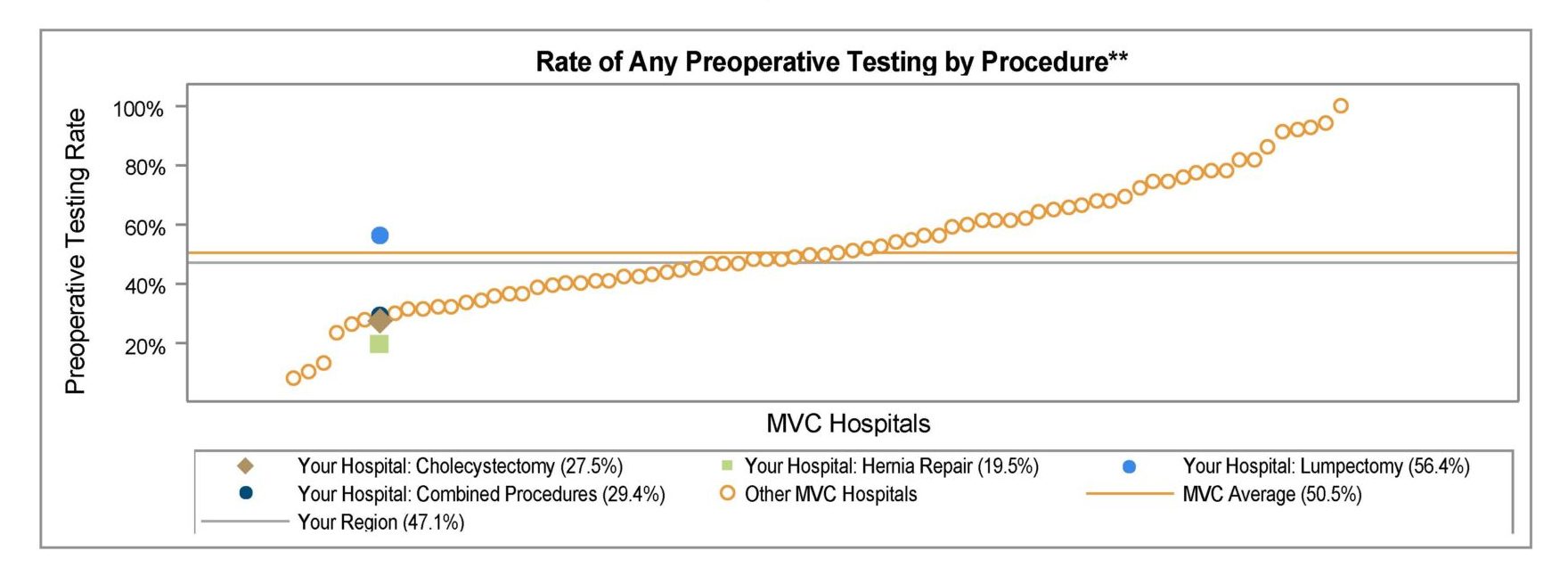
Their project varies slightly from MVC’s preoperative testing offerings in that MSQC includes a slightly broader range of low-risk surgeries. The MSQC preop testing project includes abstraction for cases of minor hernia (abdominal hernias <3 cm and all inguinal/ femoral hernia repairs), laparoscopic cholecystectomy, and breast lumpectomy.
During the pilot, MSQC included all ASA classes in their analysis. Based on feedback from site participants, however, MSQC has since limited their evaluated cases to only ASA class I and II, elective cases, and low-risk surgeries identified as the intended primary procedure (based on CPT codes) for 2024. Patients falling into ASA classes I and II are expected to be stable with their comorbid conditions and therefore require less frequent testing.
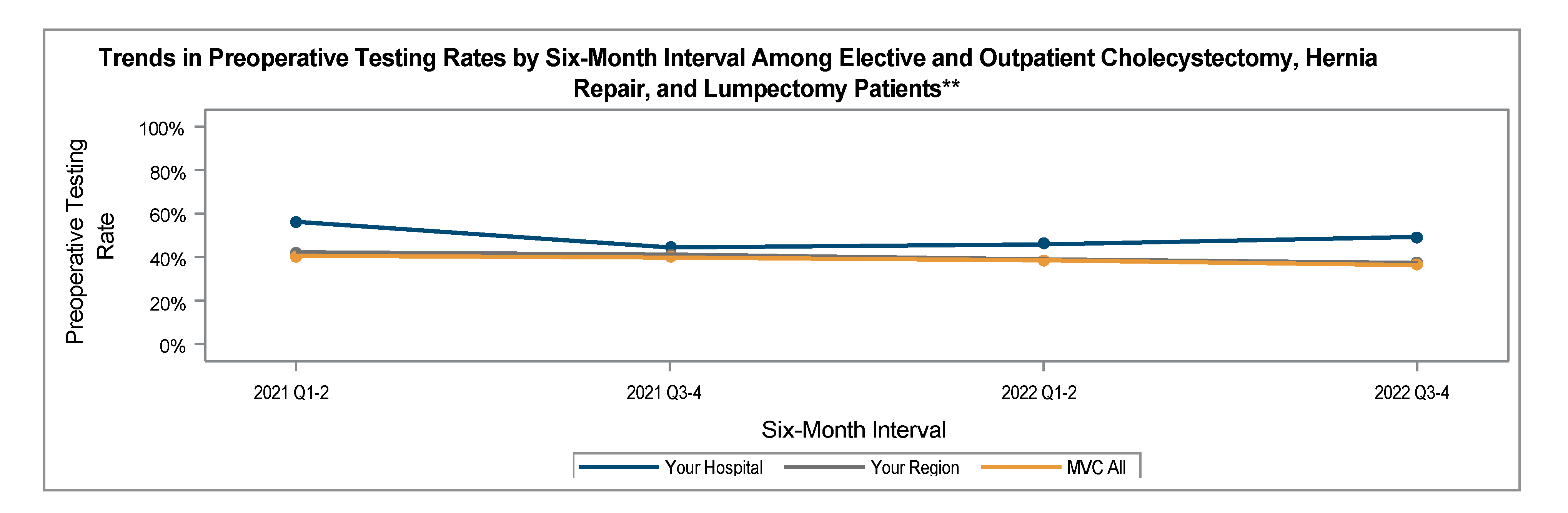
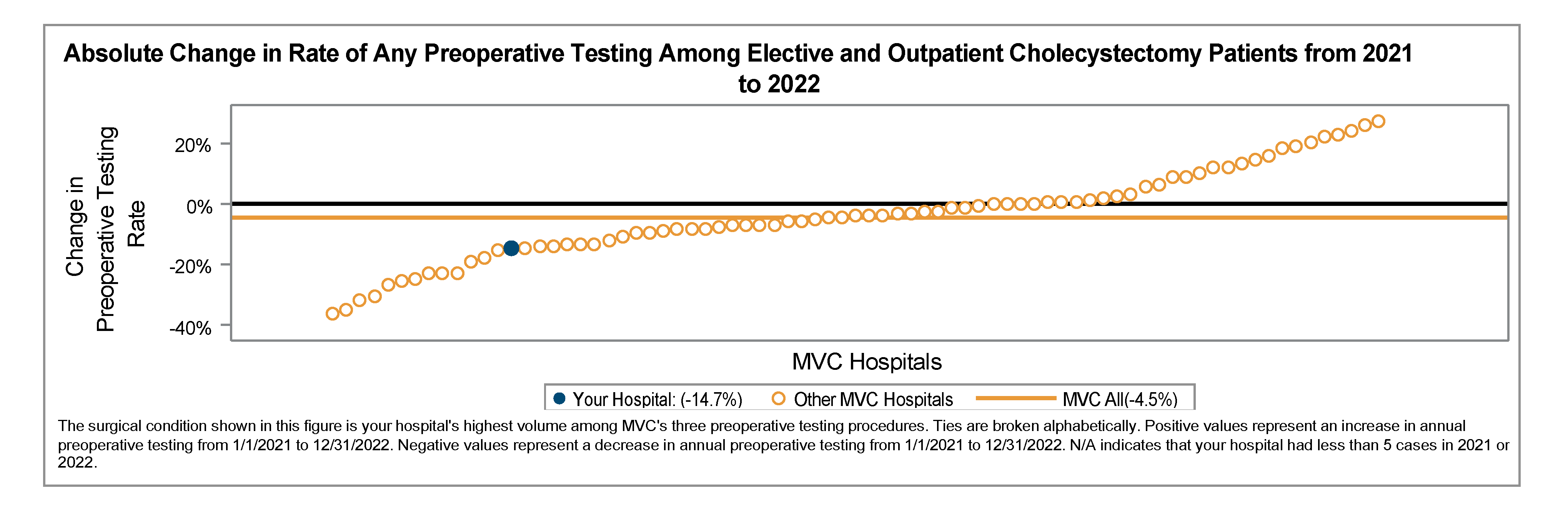
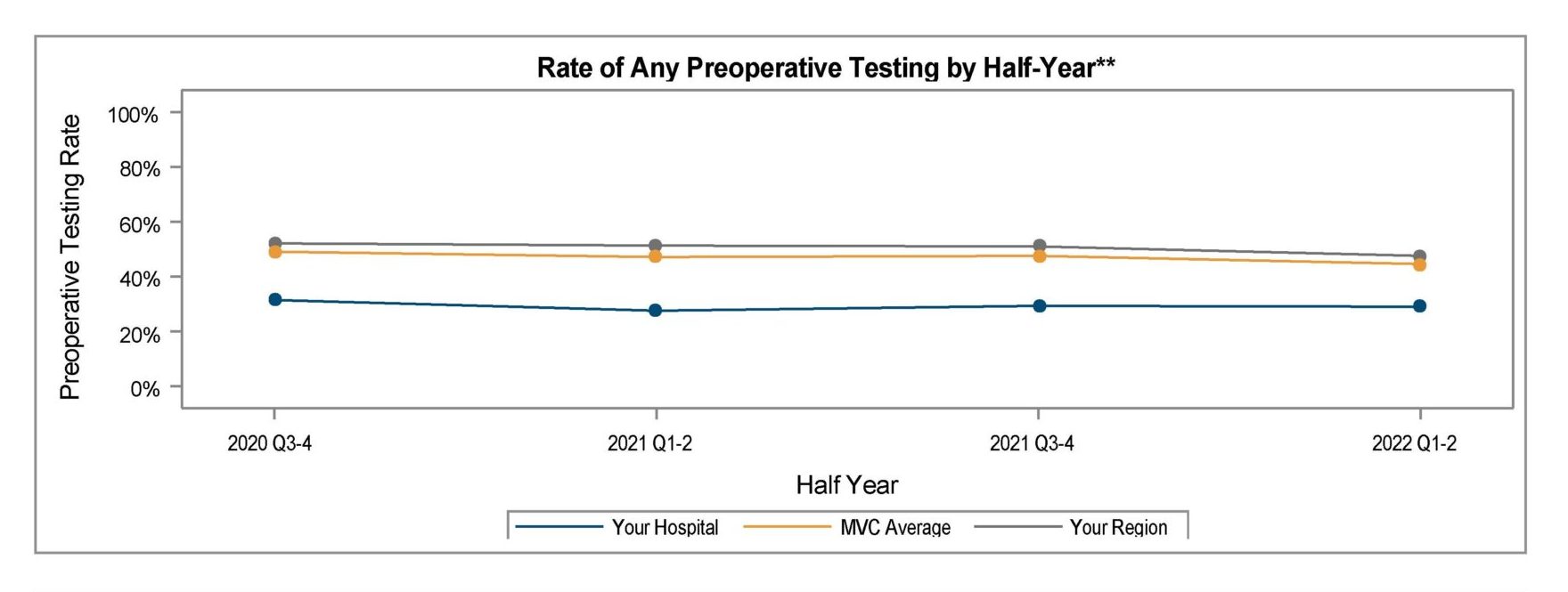
Overall, results since September 2024 suggest ASA I and II cases are all trending in the right direction; abstracted data currently indicates preop testing rates of 18% among ASA I cases (with a goal of 25% or less) and 31% among ASA II cases (with a goal of 32% or less), as shown in Figure 1.
Racchi also noted that the success of reducing preoperative testing is dependent on there being no further increases in unnecessary testing on the day of surgery. Historically, MSQC has calculated preoperative testing rates like MVC, up to 30 days prior to a surgery but not including the day of surgery. However, MSQC’s abstractors can additionally identify testing completed on the day of surgery. In 2024, MSQC abstractors are assessing cases that received testing on the day of surgery as well as those that received testing in the 30 days prior to a surgery. Preliminary performance results suggested there was an increase in day of preoperative testing when compared to baseline for both ASA I and II cases. Racchi noted that these analyses help determine whether testing was clinically necessary versus a result of physician habit.
Racchi and Fortney both spoke to the benefits of increasing engagement between surgery and anesthesiology to streamline preoperative testing protocols and processes. Between 2022 and 2023, ProMedica Charles and Virginia Hickman was able to reduce their preoperative testing rate by nearly 20% with just a few modifications to their testing protocol and additional onboarding of the anesthesiology providers.
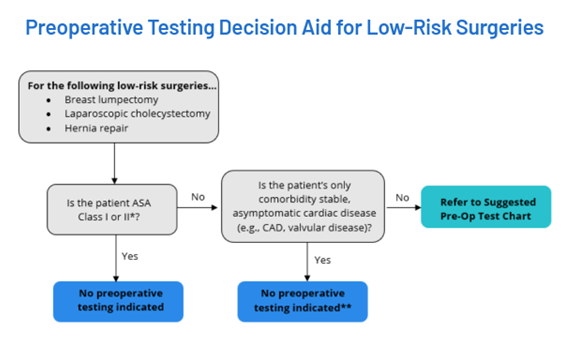
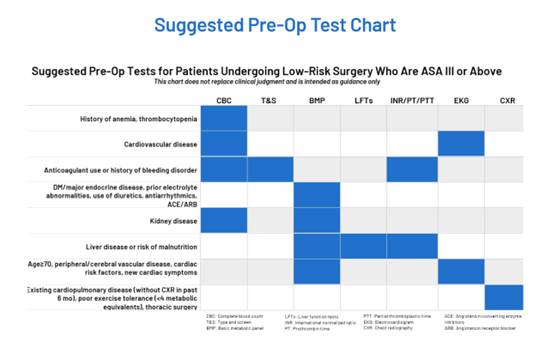
A recent review of preoperative testing cases at ProMedica Hickman that were labeled unnecessary revealed nearly 40% were, in fact, medically justified and another 42% were due to protocol misinterpretation. Interestingly, the greatest rate of unnecessary preoperative testing was found to derive from ProMedica Hickman’s preadmission testing department. Fortney noted they had success embedding an adapted version of the RITE-Size program’s decision aid (Figure 2) within their anesthesiology preoperative protocols, and this helped to provide a more robust visual for their providers to reference when completing preop documentation.
ProMedica Hickman additionally implemented a process for one-on-one training with preadmission testing (PAT) nursing staff, re-education, and the inclusion of case studies. The PAT nurses have also been included in MSQC/RITE-Size project update meetings and are given access to push reports so they can better understand their progress and impact.
The RITE-Size project is a collaboration between several CQI organizations – the Michigan Program on Value Enhancement (MPrOVE), the Michigan Value Collaborative (MVC), MSQC, and the Anesthesiology Performance Improvement and Reporting Exchange (ASPIRE). Each organization has individual projects underway to address unnecessary preoperative testing, but also collaborate under the umbrella of RITE-Size to support de-implementation with additional customized support and coaching. Learn more about RITE-Size by visiting the program website here.
November 5 Preoperative Testing Workgroup
November Cardiac Rehab Workgroup: Marshfield Medical Center – Dickinson
The second November workgroup focused on cardiac rehabilitation – another of MVC’s value-based initiatives. This workgroup featured a joint presentation by Carolyn Hoy, BSN, Director of Quality; Courtney Swanson, BSN, RN, Heart Care Clinic and Cardiopulmonary Rehab Manager; and Lacey Schjoth, BS, Cardiac Rehab Coordinator at Marshfield Medical Center – Dickinson. Hoy, Swanson, and Schjoth’s presentation introduced Marshfield – Dickinson’s cardiac rehab Patient Access Improvement Project, an initiative rooted in one of their core values of patient-centered care.
Although part of a much larger system, Marshfield Medical Center – Dickinson is a relatively small hospital with about 49 general med/surgical beds. To support a significantly rural population in the Upper Peninsula, the Marshfield – Dickinson team identified the need to modify their cardiac rehab program to improve access. Their three main goals included:
- Increase the volume of patients seen,
- Accurately track referrals,
- Expand services to include a supervised exercise therapy (SET) peripheral artery disease (PAD) program
Swanson and Schjoth described how the Northern Michigan landscape and weather contributed to some of the barriers patients faced in accessing cardiac rehab care. Outside of Marshfield – Dickinson’s cardiac rehab center, the next rehabilitation facility is nearly 45 miles away. To support patients driving a long distance to receive cardiac rehab, the team worked to coordinate with their patient’s other appointments. They also flexed their schedules to accommodate earlier or later availability and were willing to shift the appointment times as needed pending weather conditions.
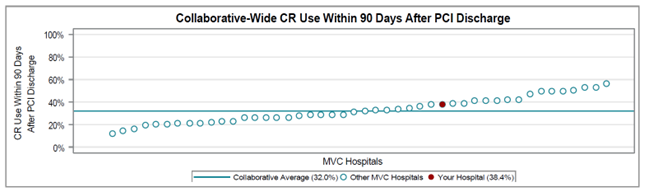
Ultimately, the team was able to increase their class size to five patients per class and increased their class offerings by one cardiac rehab (and one pulmonary rehab) class per day by December 2023. They saw a nearly 27% increase in patient enrollment between 2022 and 2023 (Figure 3). Thus far in 2024, their patient volumes are on track to match or exceed 2023.
Since Marshfield – Dickinson is unable to support a Phase 1 cardiac rehab program, most of their referrals come from outside facilities located in Wisconsin. Connecting with patients quickly after referrals are received is helpful to reduce the duration of time between referral and enrollment. With adjustments to their workflow, the team was able to reduce the average time from referral to initial contact to an average of just 3.5 days as of November 2024. The team also observed a corresponding reduction in the time to first cardiac rehab visit of just 16.5 days on average.
However, rectifying referral documentation from multiple outside sources can slow down this process. Additionally, surveyed patients reported that one of the largest barriers to starting cardiac rehab was a lack of insurance coverage or high copays, with nearly 9% of patients identifying this as the primary reason they did not schedule their initial cardiac rehab appointment in 2024. The team has recently brought on a financial counselor to assist in contacting insurance companies and ensuring adequate and accurate referrals documentation.
Lastly, the Marshfield – Dickinson cardiac rehab team worked to develop close partnerships with local cardiology providers. Ensuring local cardiology providers are aware of and supportive of cardiac rehab is a critical step that generates additional opportunities for program endorsement and patient education by the provider. Marshfield – Dickinson has additionally added Dr. Massabni, an interventional cardiologist specializing in peripheral artery disease, to their staff. This allowed them to further develop their SET PAD program in January 2024 and they are seeing increasing enrollment in this specialized vascular program.
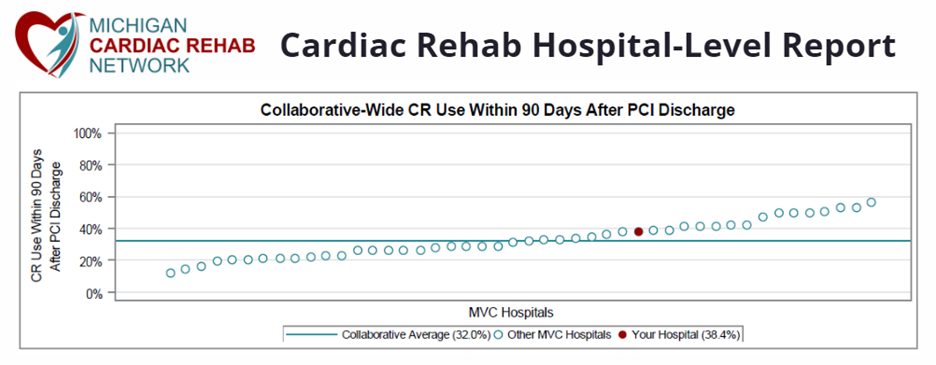
Much of MVC’s work with its members and partners in the space of cardiac rehab is delivered under the umbrella of the Michigan Cardiac Rehab network (MiCR), a collaborative partnership with the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2). You can see the MiCR website and offerings here. MVC also offers a robust registry of medical insurance claims data and data specialists that can help navigate and create custom analytic reports on cardiac rehab utilization metrics. Please reach out to the Coordinating Center by email if you would like to learn more about MVC data or engagement offerings.
November 21 Cardiac Rehab Workgroup
To learn more about the efforts showcased by November’s workgroup presenters, or other past workgroup presentations, please visit MVC’s YouTube Channel here.
December’s workgroups will feature a post-discharge follow-up presentation on December 3 led by Crystal Young of Corewell Health Trenton and Natalie Holland of MDHHS. Additionally, on December 12, Toni Moriarty-Smith of McLaren Northern Michigan will present a rural health presentation. The complete 2024 and 2025 MVC event calendars and workgroup registration links are available here.