At the end of February, MVC updated its registry with new payer data. MVC adds new data to the registry monthly upon receipt of new claims from included payers. This most recent update included the addition of two new months of Blue Cross Blue Shield of Michigan (BCBSM) and Blue Care Network (BCN) claims, one new quarter of Medicaid claims, and one new quarter of Medicare claims. Following these updates, the MVC registry now has the following data ranges for its data:
- BCBSM PPO (Commercial and Medicare Advantage): 01/01/2015 – 12/31/2024 (index events through 09/30/2024)
- BCN (Commercial and Medicare Advantage): 01/01/2015 – 12/31/2024 (index events through 09/30/2024)
- Medicaid: 01/01/2015 – 12/31/2024 (index events through 09/30/2024)
- Medicare FFS: 01/01/2015 – 06/30/2024 (index events through 03/31/2024)
Anytime MVC publishes new data on its registry, the newest claims for each payer are incorporated throughout the various reports and dashboards where that payer’s data is present, including the interactive multi-payer reports for cardiac rehabilitation utilization and preoperative testing.
Refreshed Multi-Payer Cardiac Rehabilitation Reports
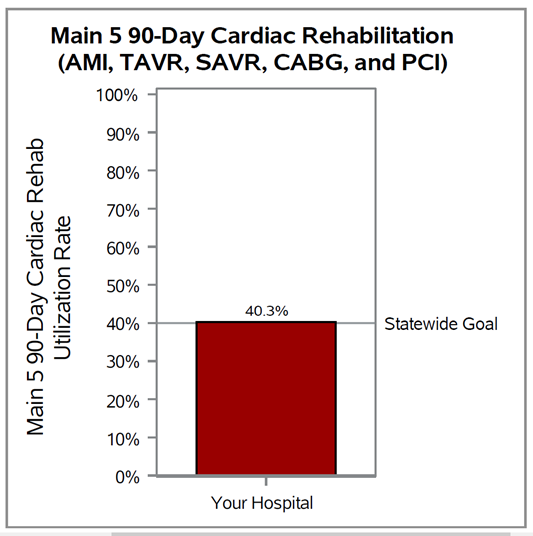
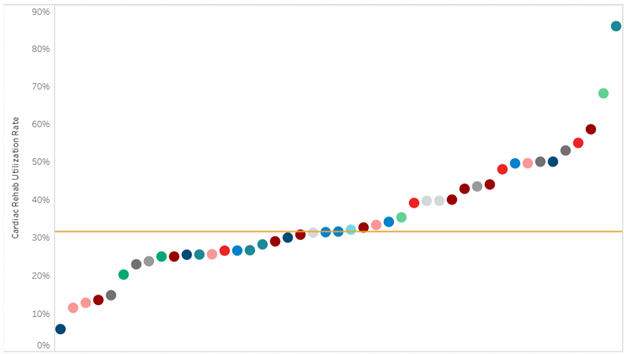
The multi-payer cardiac rehabilitation utilization reports were added to the registry in the first half of 2024 and have replaced the static PDF hospital-level push reports MVC previously distributed biannually. The regular release of new data on the registry, therefore, gives members opportunities throughout the year to check progress on cardiac rehabilitation metrics more regularly and find opportunities for improvement. For example, current data on cardiac rehabilitation enrollment for CABG patients with episode start dates between Jan. 1, 2024, and Sept. 30, 2024, indicates wide variability among hospitals, with many sites observing rates below the recommended 70%. Across the collaborative, enrollment in cardiac rehab after CABG procedures was as low as 28% at one MVC member hospital and as high as 83% at another with a statewide average of 61% (Figure 1). Similarly, cardiac rehab utilization is much lower on average among PCI patients over the same time period (32%), and there is wide inter-hospital variation with rates ranging between 6% and 86% (Figure 2).
Figure 1. Statewide Rankings for Cardiac Rehab Utilization within 90 Days After Discharge from CABG, 1/1/2024-9/30/2024
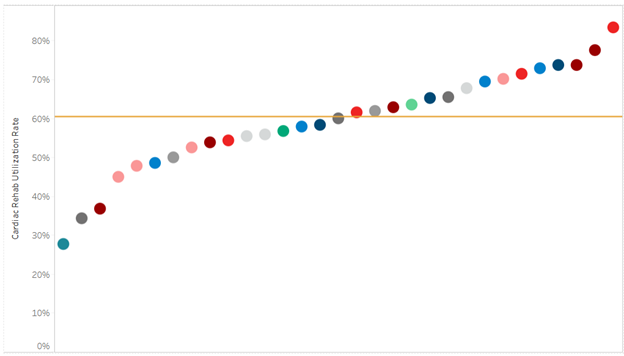
Figure 2. Statewide Rankings for Cardiac Rehab Utilization within 90 Days After Discharge from PCI, 1/1/2024-9/30/2024
This latest registry update also included a methodological change impacting cardiac rehabilitation reporting for attendance. These methodological improvements were meant to increase the accuracy of MVC’s reported mean number of visits attended within a selected time period. MVC noted that this change resulted in increases in the average number of completed cardiac rehabilitation visits overall, and especially among BCN and Medicaid beneficiaries. This increase in the average number of visits reflects the fact that MVC improved the capture of multiple cardiac rehabilitation visits over a longer time period billed on a single claim.
Refreshed Multi-Payer Preoperative Testing Reports
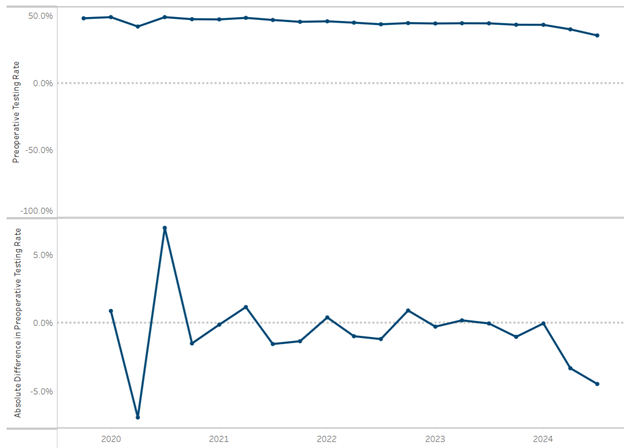
The multi-payer preoperative testing utilization reports were added to the registry at the end of 2024 and have also replaced static hospital-level push reports that were previously distributed as biannual PDF reports to members. Looking at all available 2024 claims across payers, there is evidence of a small decrease in the MVC All rate of preoperative testing prior to low-risk surgery beginning in late 2022 and continuing throughout 2023 and into 2024 (Figure 3). Those members who are working to reduce unnecessary preoperative testing are encouraged to check their updated data. MVC is also able to supplement registry data with custom analytics by an MVC analyst to meet the needs of members. One such site recently utilized MVC’s custom analytics to identify differences in preoperative testing rates by physician NPI to support conversations about intra-hospital variation by provider and service line.
Figure 3. Statewide Rate of Preoperative Testing and Relative Difference in Preoperative Testing by Quarter, 2020-2024
MVC’s registry contains an extensive collection of multi-payer, P4P, and payer-specific views and metrics. If you are newer to the registry or would like a refresher on how best to leverage the information, reach out to the MVC Coordinating Center for information about a custom registry review.