Collaboration in Action: Shaping the Future of Healthcare Across Michigan
The Michigan Value Collaborative (MVC) held its spring 2025 collaborative-wide meeting on Friday, May 9, in Midland. A total of 106 attendees representing 62 hospitals, 6 physician organizations, 6 Collaborative Quality Initiatives (CQIs), and 11 healthcare systems from across the state of Michigan came together to build partnerships and collaborate on approaches to healthcare delivery that will have a long-lasting impact.
MVC Director Dr. Hari Nathan kicked off Friday’s meeting with updates on the MVC Coordinating Center [. He introduced MVC’s newest team members, senior analysts Steven Ellinger and Tanima Basu, and Program Assistant Dinah Pollard. Dr. Nathan also announced the promotion of Jana Stewart to Associate Program Manager and welcomed Dr. Jessica Golbus as the new Co-Director of the Michigan Cardiac Rehab network (MiCR). He provided an update on recruitment progress for Phase II of the RITE-Size pilot and encouraged sites interested in participating to reach out to the MVC Coordinating Center. Dr. Nathan concluded the welcome presentation by highlighting MVC reporting updates. These included new multi-payer preoperative testing dashboard reports added to MVC’s data registry in Q4 of 2024, and five hospital-level push reports with data reflecting P4P Program Year (PY) 2026-2027 selections, statewide health equity, process measures, P4P PY 2024 final scorecards, and ED-based episodes.
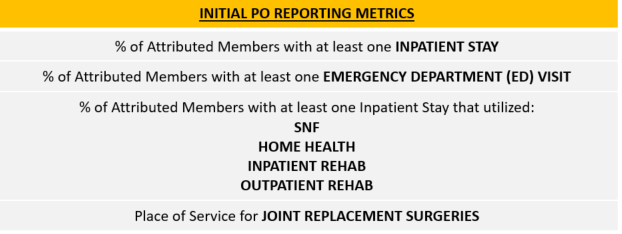
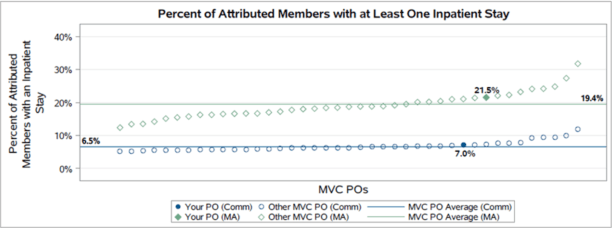
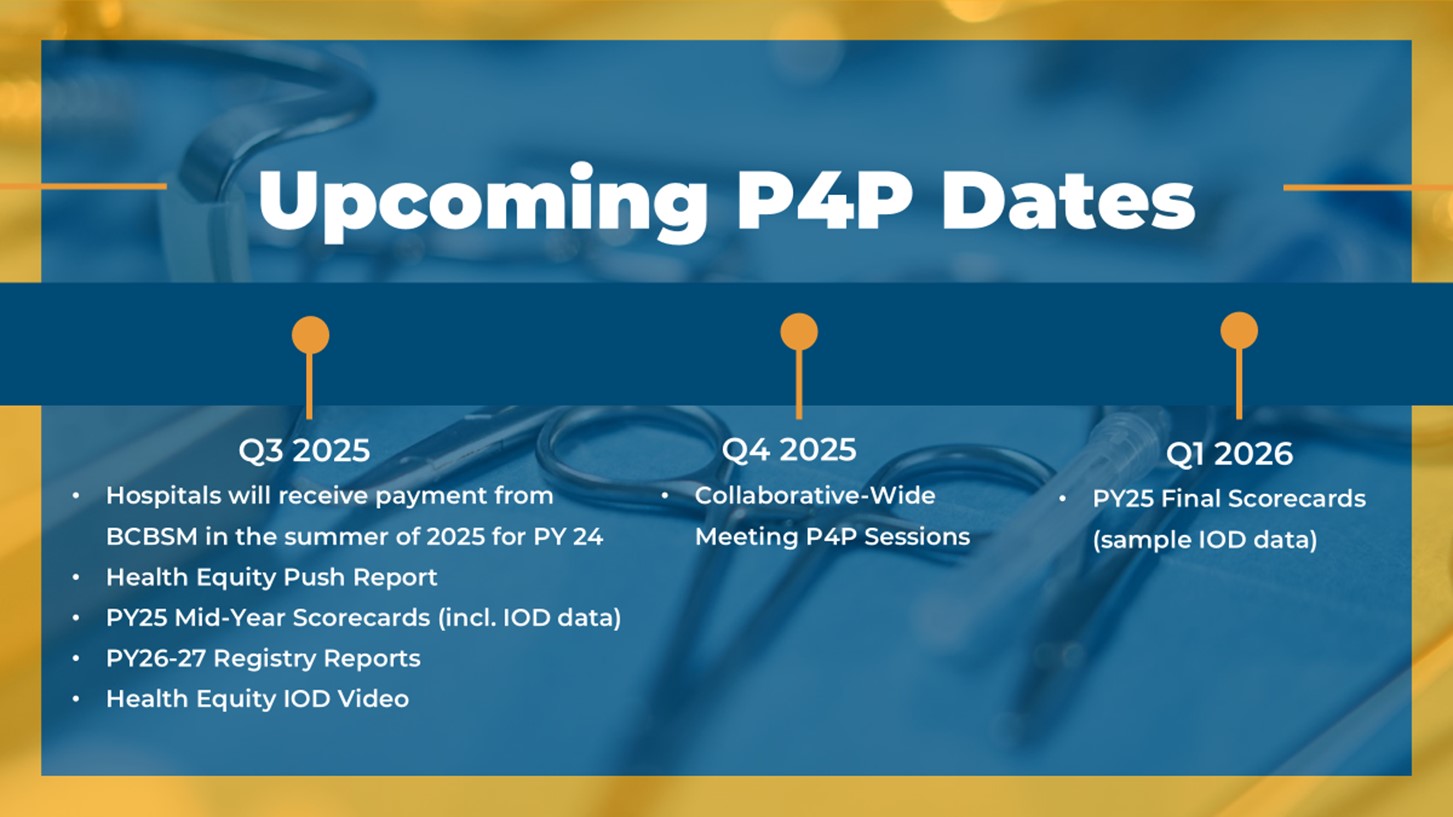
Managing Director Mark Bradshaw, MSc, presented a summary of PY 2024 scoring and PY 2026-2027 selections for the MVC Component of the BCBSM P4P Program [SEE SLIDES]. In his summary of PY 2024 scoring, Bradshaw highlighted opportunities for members to leverage MVC resources to optimize P4P scores via MVC’s engagement point menu options and highlighted some of the value metrics that have seen success after their first year of scoring.
The overview of MVC members’ P4P selections included a comparison of the value metric selections that were made for the PY 2024-2025 vs. the PY 2026-2027 program cycles (Figure 1). Bradshaw also reviewed MVC’s new health equity measure and index of disparity before closing with a reminder about upcoming dates relevant to participating P4P hospitals (Figure 2).
Figure 1.
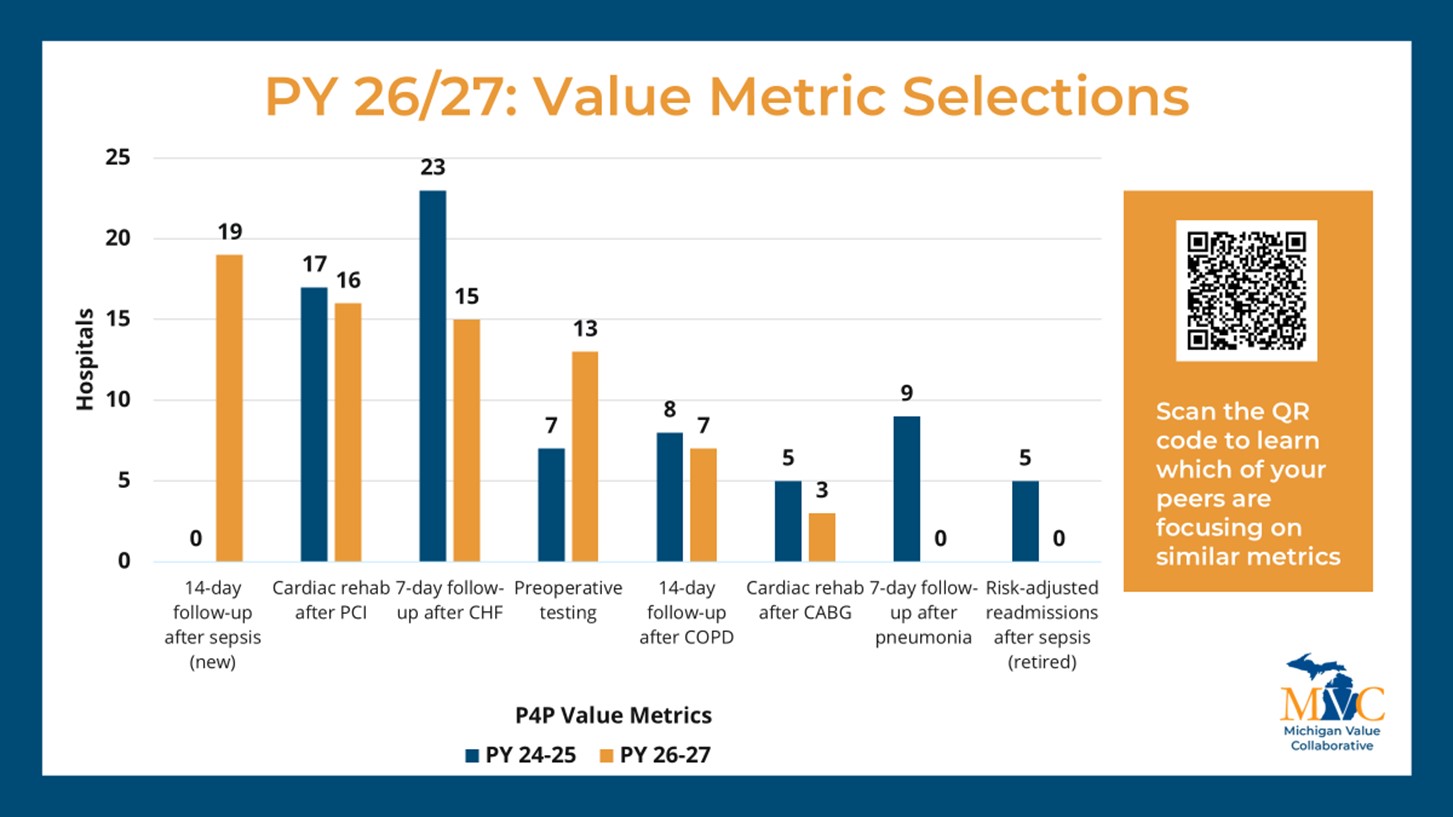
Figure 2.
The meeting then featured MVC’s first Engagement Awards, presented by MVC Engagement Manager Jessica Souva, MSN, RN, C-ONQS. MVC presented the awards to members who went above and beyond in their engagement with MVC to the benefit of the entire MVC membership. Scheurer Health received the award for the most engaged peer group 5 hospital, MyMichigan Collaborative Care organization for the most engaged physician organization (PO), Chelsea Hospital for the most engaged hospital, and Corewell Health for the most engaged health system.
Souva remained at the podium for a presentation on MVC’s 2024 Quality Improvement (QI) survey, sharing details about the survey’s purpose, completion rate, results, and applications [SEE SLIDES]. The four most widely reported QI initiatives included sepsis, health equity, readmissions, and emergency department care, and also aligned with the initiatives reported as highest priority for some of the largest health systems in Michigan (Figure 3). Souva provided specific examples of MVC engagement activities that were developed to specifically support the initiatives reported in the QI survey and address common barriers members reported facing. She urged MVC’s PO members to participate in the 2025 QI survey so that MVC will be better equipped to provide support for PO QI initiatives in the future.
Figure 3.

Before sending meeting attendees to participate in the poster session, Souva shared the responses from the opening virtual ice-breaker question: “What keeps you motivated to continue working in healthcare?” Members credited their teams and making a difference in the lives of patients and families as their motivation to persevere during challenging times. Posters were then presented by partner CQIs such as MEDIC, MOQC, MSHIELD, and MI Mind. Electronic copies of the posters are available on the spring meeting website [LINK]. The MVC Coordinating Center would like to thank all poster presenters for sharing their work.
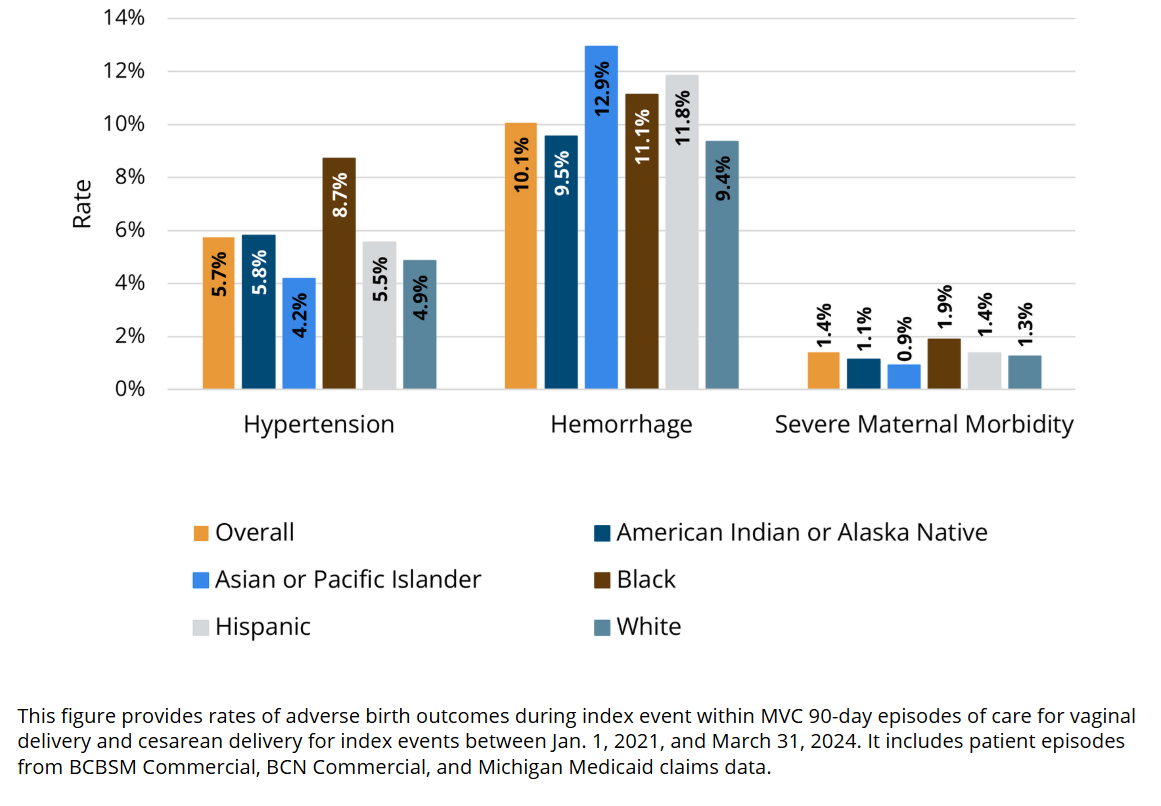
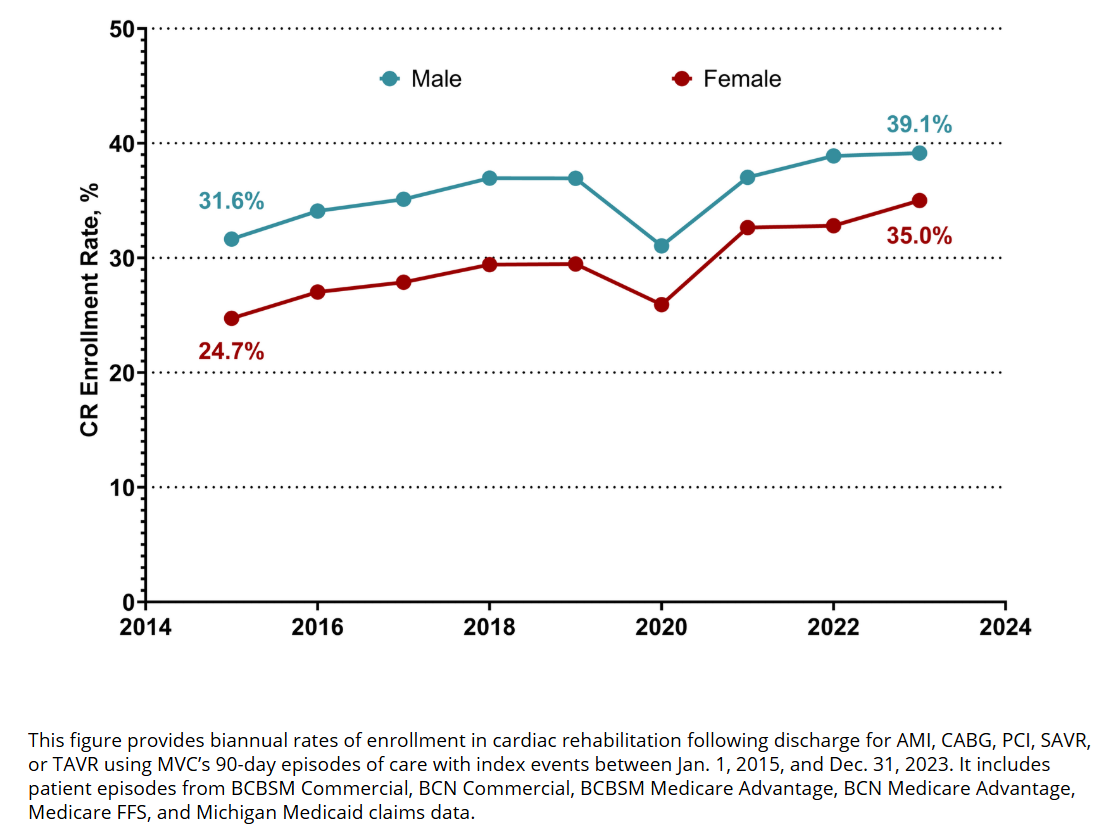
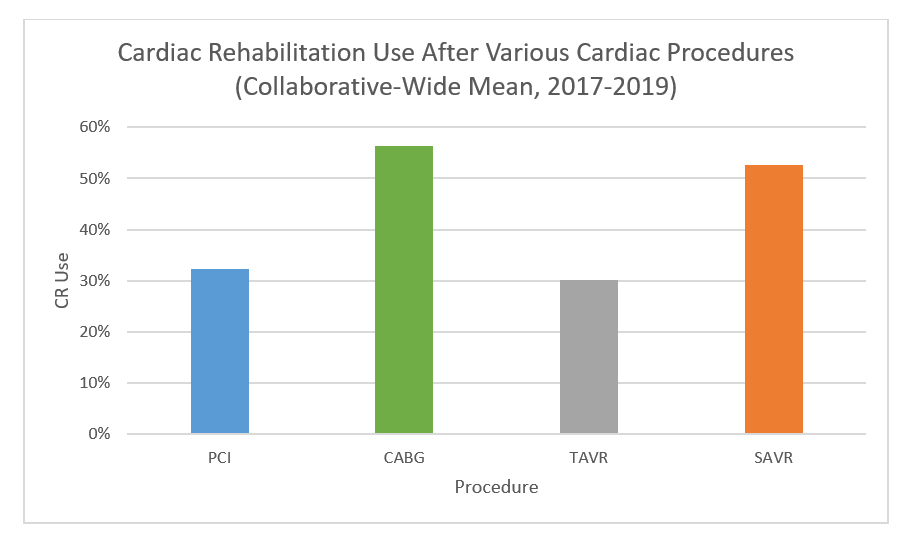
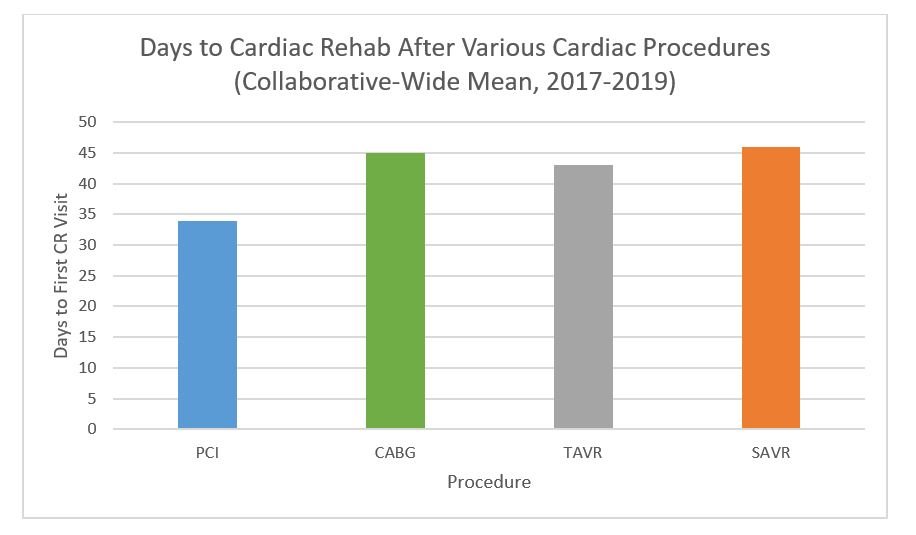
After the poster session, MVC Associate Program Manager Jana Stewart, MPH, provided a presentation highlight the ways in which MVC collaboratives with other CQIs to help drive local quality improvement efforts in hospitals across Michigan. This included two case studies and unblinded data presentations for MVC’s two value-based initiatives: cardiac rehabilitation utilization and preoperative testing de-implementation. She also presented a use case for a new area MVC is exploring within its ED-based episodes of care focused on behavioral health care and outcomes, also with aggregate and hospital-level unblinded data.
Since the launch of MVC's cardiac rehabilitation initiative in 2020, the work has been incorporated into all aspects of MVC’s portfolio, from dedicated workgroup topics to reporting and related P4P metrics, and it also led to the 2022 launch of MiCR in partnership with BMC2 and the NewBeat program in partnership with HBOM. Cardiac rehabilitation enrollment for patients discharged from a “Main 5” condition (e.g., AMI, CABG, PCI, SAVR, and TAVR), has increased across the collaborative from 24% in 2020 to 34% in 2023, amounting to an estimated 145 lives saved and 243 readmissions avoided. Stewart also shared that the mean days to a patient’s first cardiac rehabilitation visit has decreased from 59 days in 2020 to 46 days in 2024.
Highlights from MVC’s preoperative testing efforts included updates on the RITE-Size pilot—a collaboration largely between MVC, MPrOVE, and MSQC—that supported three MVC member hospitals in reducing their low-value preoperative testing rates in 2024 through a variety of strategies. Stewart called out that members interested in participating in Phase II of the pilot in 2025 or 2026 will be well positioned to both reduce their testing rates significantly and also achieve the full two engagement points for 2025. She encouraged anyone interested to reach out to the MVC Coordinating Center for additional information.
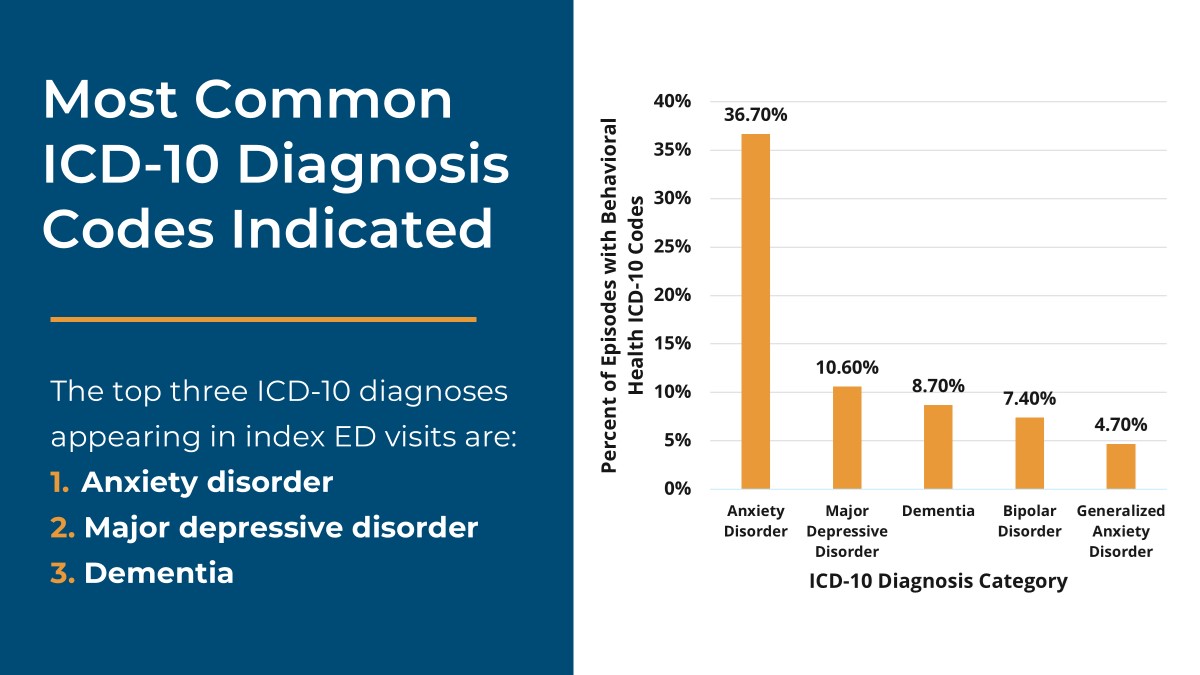
Stewart concluded by sharing aggregate and unblinded data on the prevalence of behavioral health as a co-diagnosis in MVC ED-based episodes, where behavioral health ICD-10 codes such as anxiety disorder, major depressive disorder, and dementia appear as co-diagnoses (Figure 4) in approximately 13% of index ED events. She also shared how those behavioral health rates differ by payer as well as condition and noted that 1 in 3 of ED patients who have a resulting inpatient admission have a behavioral health code noted as a comorbidity.
Figure 4.
After a networking lunch, attendees spent the afternoon participating in roundtable discussions and small group activities on two to three topics [SEE ROUNDTABLE MATERIALS]. During the session, attendees could either join three roundtable discussions or join one roundtable and one small group activity on system approaches to QI. At each table attendees learned about the work of the roundtable facilitator, asked questions, and discussed similar initiatives at their own organizations. In the system activity, MVC members were asked a series of questions about measuring system-level QI, and their responses will help inform MVC’s future work to support health systems across Michigan.
The meeting closed with a reflection of the day spent together, reminders about upcoming meetings, and opportunities for best practice sharing with other MVC members.
If you have questions about any of the topics discussed at MVC’s spring collaborative-wide meeting or are interested in following up for more details, contact the MVC Coordinating Center. MVC’s next collaborative-wide meeting will be in person on Fri., Oct. 10, 2025, in Livonia.