Hospitals across Michigan are increasingly focused on using their available data to assess care delivery gaps, inefficiencies, and areas for improvement. The Michigan Value Collaborative (MVC) developed its 2024 Statewide Health Equity Report to provide a detailed summary of how hospitals across Michigan are approaching this process with a health equity lens. By analyzing MVC claims data along with survey responses from 52 hospitals and 11 health systems, the full report captures how hospitals are leveraging data to evaluate patient care, identify disparities in outcomes, and develop interventions that improve the overall value of care delivery.
Data Collection and Utilization
One of the key highlights of the report was the varied approach and capacity for collecting, measuring, and utilizing data on health equity. Many hospitals utilize readmission rates, clinical quality indicators, and demographic information to identify variations in care. However, the extent to which this data informs hospital-level decisions varies. While some hospitals remain in the early stages of collecting and organizing health equity data, others are beginning to analyze and apply these insights to shape their initiatives. Nearly a third of respondents indicated they were using data to guide funding and program priorities, while a smaller percentage integrated equity metrics into quality improvement strategies.
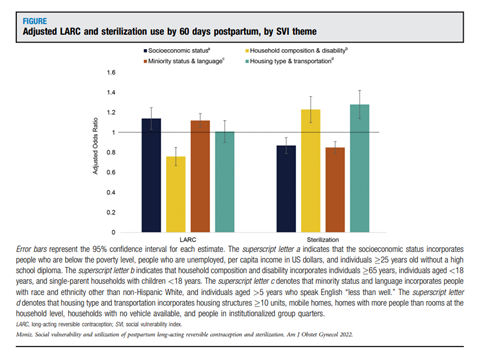
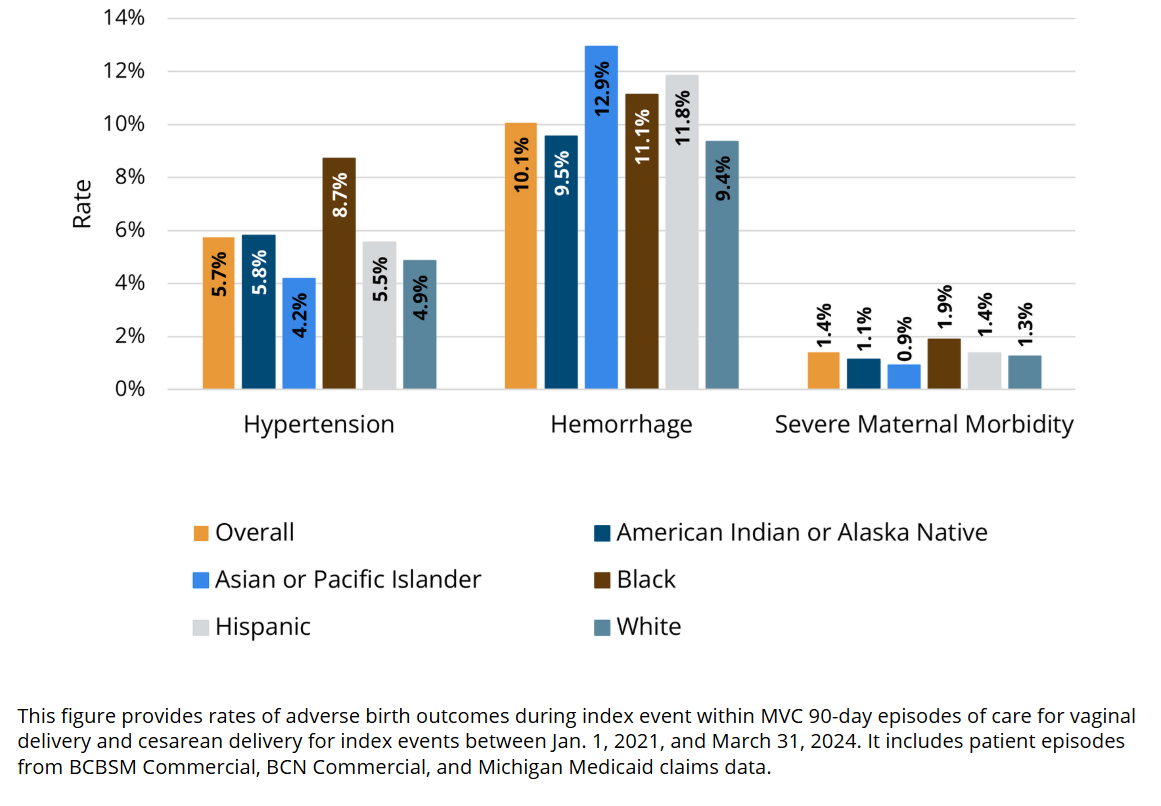
To further support hospitals in taking action, MVC used its robust medical insurance claims-based data to highlight established disparities for specific service lines. A notable finding was the difference in rates of birth complications by race (Figure 1). Women who identify as Asian and/or Pacific Islander had higher rates of postpartum hemorrhage than other race categories, and patients identified as Black had higher rates of hypertension and severe maternal morbidity (SMM) than the overall population.
Figure 1. Rates of Hypertension, Hemorrhage, and Severe Maternal Morbidity During Index Hospitalization, Overall and by Patient Race/Ethnicity, 2021-2024
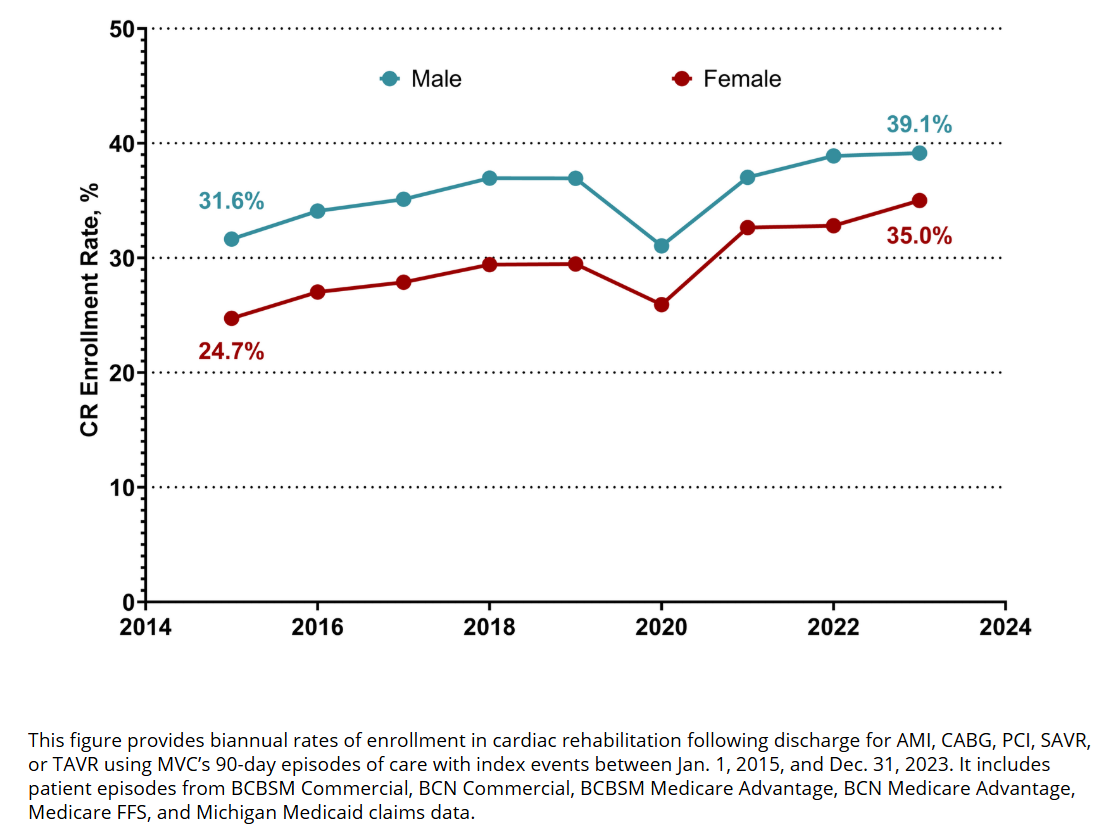
Another notable finding was sex differences in cardiac rehabilitation enrollment (Figure 2). Women are significantly less likely to enroll in cardiac rehab within 90 days of discharge for eligible cardiac procedures, take longer to enroll in their first session, and attend fewer sessions on average than male patients. These patterns point to differences in how patients access and engage with follow-up care, and these gaps are present even among hospitals with strong cardiac rehabilitation enrollment rates.
Figure 2. Rates of Cardiac Rehabilitation Utilization within 90 Days of Discharge from a Qualifying Event by Sex, 2015-2023
These MVC claims-based investigations into healthcare outcomes across populations can assist hospitals in setting or enhancing their health equity goals.
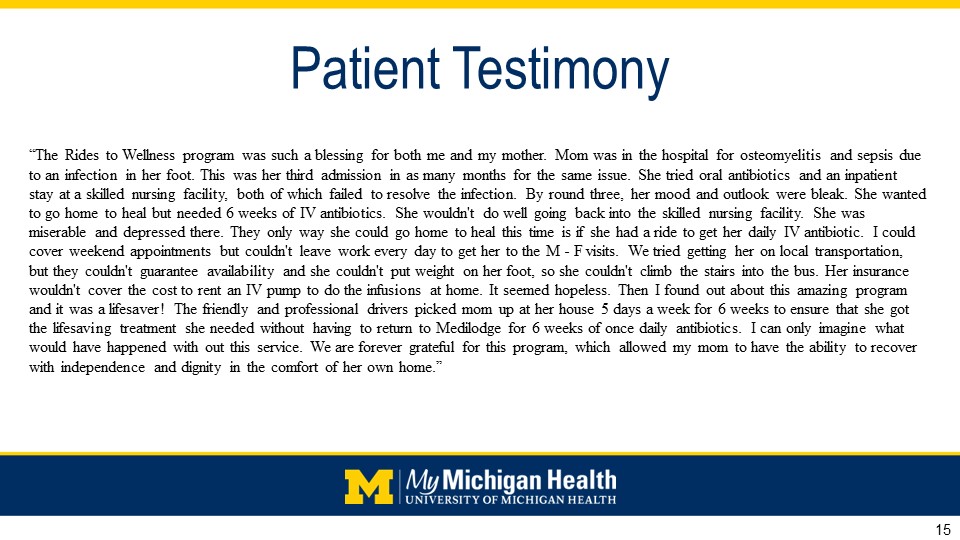
Efforts to Improve Healthcare Access
Beyond data collection and analyses, the report summarized a range of efforts to improve healthcare access. Most hospitals have expanded telemedicine services, increased clinic hours, deployed mobile health units, support non-emergency medical transportation programs, and offer rideshare assistance to reach a variety of patient populations who struggle to access care in their community. Language accessibility has also been a focus, with nearly 90% of hospitals offering translated materials and on-site interpretation services. Financial barriers remain a concern, with 79% of hospitals reporting efforts to support patients dealing with medical debt or lacking insurance coverage.
There were also several hospitals implementing community-based programming and solutions in response to gaps for specific disease impacted communities or underserved groups. The most common types of solutions currently supported by hospitals across the state included:
- Food Security Initiatives: Many hospitals are addressing food insecurity by screening patients for social needs, partnering with community food programs, and even launching hospital-based farms and Healthy Food Rx programs to encourage nutrition-based health interventions.
- Community Health Workers (CHWs): Increasingly, hospitals are integrating CHWs into their care models to bridge the gap between clinical care and community-based support, particularly in rural and underserved areas.
- Incorporating Patient Voices: Hospitals are utilizing Community Health Needs Assessments (CHNAs), patient experience surveys, and community advisory boards to ensure that patient perspectives inform quality improvement initiatives.
Looking Ahead
Although most hospitals have taken steps to improve care delivery across all patient populations, they face significant organizational barriers, such as insufficient funding for dedicated staff and programming, lack of staff training or expertise in community-focused challenges, and difficulty communicating the business case or return on investment of such efforts. These barriers and new ones will likely grow in the coming months and years as the field’s federal funding streams shift.
Amid that uncertainty, MVC hopes to play the role of facilitator by supporting hospitals with actionable equity data, facilitating peer learning opportunities through dedicated meetings and sharing of success stories, and financial incentives through the MVC Component of the BCBSM P4P Program. In addition, the MVC Coordinating Center regularly consults with the Michigan Social Health Interventions to Eliminate Disparities (MSHIELD) team on best practices for data collection and equity-centered quality improvement. MVC will demonstrate this commitment via its quarterly MVC member spotlight blog—which will highlight successful initiatives across MVC’s membership—and via dedicated learning sessions at MVC’s Oct. 10 collaborative-wide meeting in Livonia.
If you are interested in pursuing a health equity initiative, MVC has a robust registry of claims data that can be utilized, as well as site specialists who can help facilitate connections with peers doing similar work. Please reach out to us by email if you have a success story to share or want to learn more about related MVC data.