After childbirth, all individuals should have access to patient-centered counseling about birth spacing, and, if desired, contraceptive methods to help fulfill their personal reproductive goals. Promoting patient-centered contraceptive care and equitable access to contraceptive methods for those who desire them may improve population health outcomes.
Researchers and medical professionals are increasingly recognizing the impact of social determinants of health (SDOH) on individuals’ access to care and overall health outcomes. Unmet social needs may affect contraceptive initiation after childbirth by influencing individuals’ preferences for future childbearing, as well as individuals’ access to high-quality contraceptive care. To better understand this relationship, a group of clinician investigators used MVC data in a paper published in the American Journal of Obstetrics and Gynecology to evaluate the association between living in a neighborhood with high social vulnerability and the use of long-acting reversible contraception (LARC) and sterilization methods during the postpartum period.
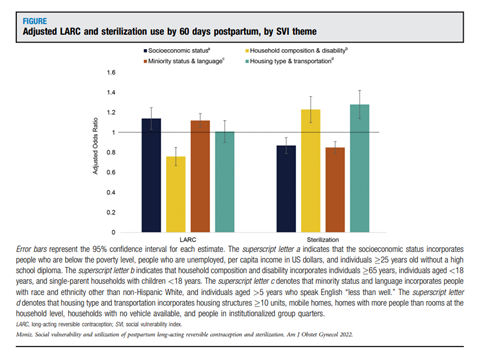
Lead author Michelle H. Moniz, MD, MSc, Program Director of the Obstetric Initiative (OBI), and her colleagues utilized MVC administrative claims data to identify childbirth episodes from Jan. 2016 to Dec. 2019 with outcomes including LARC and sterilization use by 60 days into the postpartum period. Social vulnerability was determined using the Centers for Disease Control and Prevention’s Social Vulnerability Index (SVI). The SVI measures a community’s economic and social resilience by integrating 15 U.S. Census variables to generate composite scores across 4 themes: socioeconomic status, household composition and disability, minority status and language, and housing type and transportation.
In 140,345 delivery episodes at 79 hospitals, 8% of patients initiated LARC devices, and 8.3% initiated sterilization by 60 days postpartum. Dr. Moniz and colleagues observed independent associations between social vulnerability and postpartum contraceptive use. It appeared that different SVI themes such as socioeconomic status, minority status and language, household composition and disability, and housing type and transportation aligned with varying use of LARCs or sterilization (Figure 1). Individuals living in neighborhoods with the highest socioeconomic vulnerability and minority status/language vulnerability were more likely to utilize LARC methods. Individuals living in neighborhoods with the highest household composition vulnerability were less likely to initiate LARC methods.
Conversely, sterilization was more likely among populations living in neighborhoods with highest housing/transportation vulnerability and less likely among those living in neighborhoods with highest socioeconomic vulnerability and minority status/language vulnerability.
Dr. Moniz and colleagues suggest that “structural factors—such as distance to clinic, fees for parking and transportation, clinic hours, childcare access, ability to miss work to seek healthcare, and out-of-pocket costs for healthcare—may affect postpartum contraceptive use.” They also note that more research is needed to fully understand the means by which SDOHs influence an individual’s healthcare preferences and choices. Additional investigations could shed light on the mechanisms by which unmet social needs influence reproductive wishes and access to patient-centered contraceptive counseling and methods after childbirth.
In all sectors of healthcare and medical research, but especially in maternal health where inequities in health outcomes have worsened in recent years, further studies must be done to better understand the impact of SDOHs. While medical advancements and the pursuit of best practices are critical to ensuring improvement in healthcare delivery, these innovations cannot impact outcomes for all patient populations until we understand the structural factors affecting patient access and goals.
MVC is committed to using data to improve the health of Michigan through sustainable, high-value healthcare. Therefore, one of MVC’s core strategic priorities is intentional partnerships with fellow Collaborative Quality Initiatives (CQIs) and quality improvement collaborators. MVC shares its data with clinical, administrative, and CQI experts for investigative analyses to help identify best practices and innovative interventions that help all members improve the quality and cost of care.
Publication Authors
Michelle H. Moniz, MD, MSc; Alex F. Peahl, MD, MSc; Dawn Zinsser, BA; Giselle E. Kolenic, MA; Molly J. Stout, MD, MS; Daniel M. Morgan, MD
Full Citation
Moniz, M. H., Peahl, A. F., Zinsser, D., Kolenic, G. E., Stout, M. J., & Morgan, D. M. (2022). Social vulnerability and use of postpartum long-acting reversible contraception and sterilization. American Journal of Obstetrics and Gynecology, 227(1). https://doi.org/10.1016/j.ajog.2022.03.031