Today is National Rural Health Day. Since 2010, the National Organization of State Offices of Rural Health set aside the third Thursday of every November to highlight the unique healthcare challenges facing residents within rural communities and celebrate providers who deliver innovative, affordable, and coordinated rural healthcare. MVC’s current membership includes 44 hospitals based in rural communities, 22 of which are designated as Critical Access Hospitals (CAHs). In tribute to National Rural Health Day and the needs of its growing rural membership, MVC hosted a special rural health workgroup yesterday.
The workgroup featured a guest presentation by Stephanie Pins, MSA, CPHQ. Pins is the Director of Quality, Risk, and Compliance for MyMichigan Medical Center Sault, formerly War Memorial Hospital, and is co-leading the Health Equity Council for MyMichigan Health. She led the creation of a transportation program for War Memorial Hospital by working with local transportation companies and applying for grants to cover the cost of the program.
This guest presentation focused on how MyMichigan is supporting rural communities through their Non-Emergency Medical Transportation (NEMT) Project, and the steps their team took to develop this program. Beginning in 2024, CMS will require that hospitals screen admitted patients for five social determinants of health (SDOH) domains. One of those five required domains is transportation needs since access to transportation and distance to care have a significant impact on healthcare outcomes.
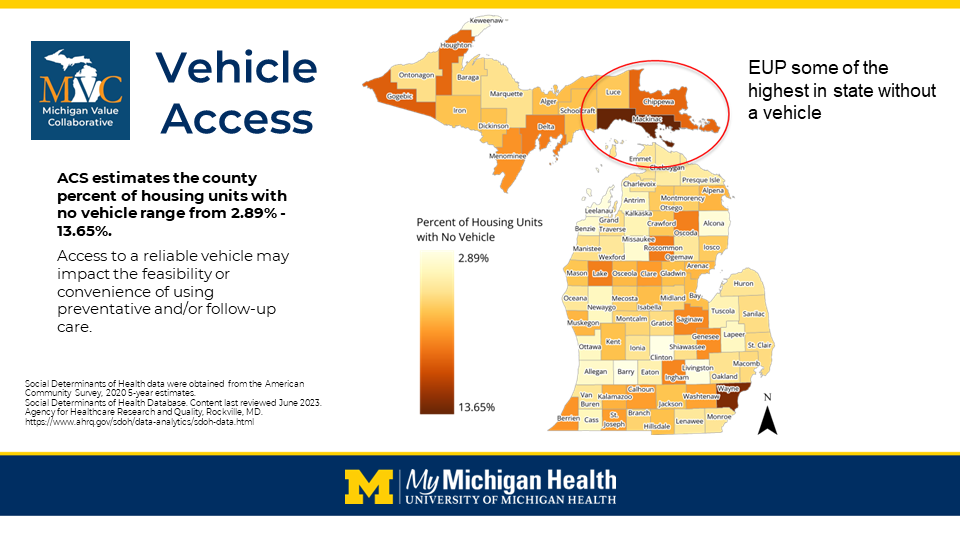
MyMichigan Medical Center Sault primarily services the very rural communities of Chippewa, Luce, and Mackinac counties, located in the eastern Upper Peninsula of Michigan. A resident of Drummond Island—part of Chippewa County—may have to drive as many as 70 miles each way to get to an appointment at MyMichigan Medical Center Sault. Limited vehicle access in this part of the state was highlighted recently at MVC’s fall collaborative-wide meeting; the eastern Upper Peninsula had some of the highest rates in the state for housing units with no vehicle (Figure 1).
While presenting, Pins emphasized that once MyMichigan identifies a need through screening, the next step is to find a way to connect those patients with the assistance they need to access medical care. One transportation solution utilized by MyMichigan Medical Center Sault is the Road-to-Recovery program, offered in partnership with McLaren Northern Michigan in Petoskey. The MyMichigan Medical Center Sault location offers some oncology cancer treatment services, but not radiation, so patients may need to travel to Petoskey—a distance of over 90 miles—to receive radiation therapy as part of their cancer treatment. The fully funded Road-to-Recovery program is available five days a week free of charge to anyone in the eastern Upper Peninsula. A hospital-owned van is driven by a volunteer driver from the MyMichigan Medical Center Sault location to scheduled pick-up locations along the I-75 corridor to Petoskey. Service times are coordinated with McLaren Northern Michigan’s oncology group so all the patients using this service have aligned appointment times. Pins shared that one noteworthy ancillary benefit of this program has been the peer support and relationship building that resulted from patients traveling together for extended periods while going through a similar treatment experience.
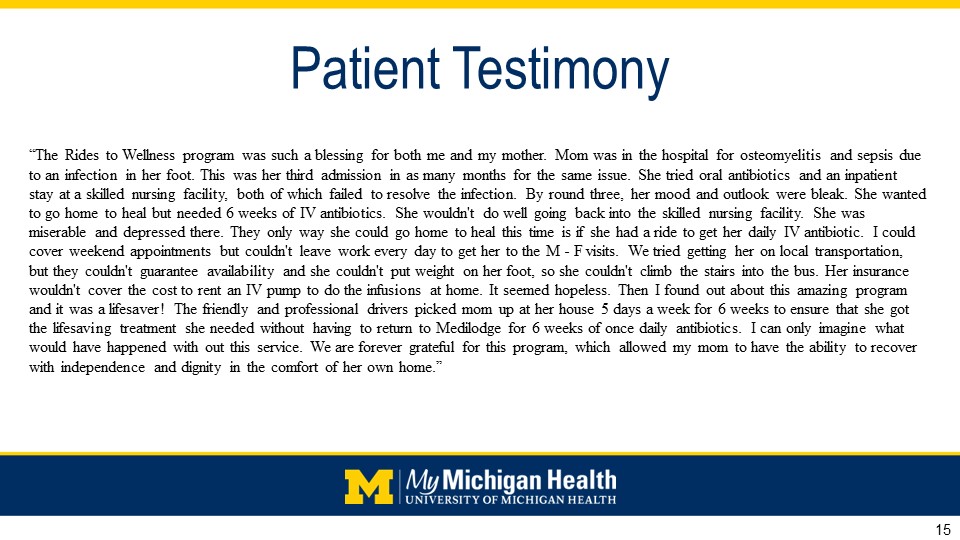
A second transportation solution utilized by MyMichigan Medical Center Sault is the Rides-to-Wellness Program, a partnership effort with local transportation companies and Connect UP. Patients can use this service to travel to other appointments or patient care services and serves as a critical stopgap in ensuring patients have somewhere to turn for time-sensitive transportation needs. Pins shared that the patient testimonials from those utilizing the service are helpful evidence of its value to the eastern Upper Peninsula (Figure 2).
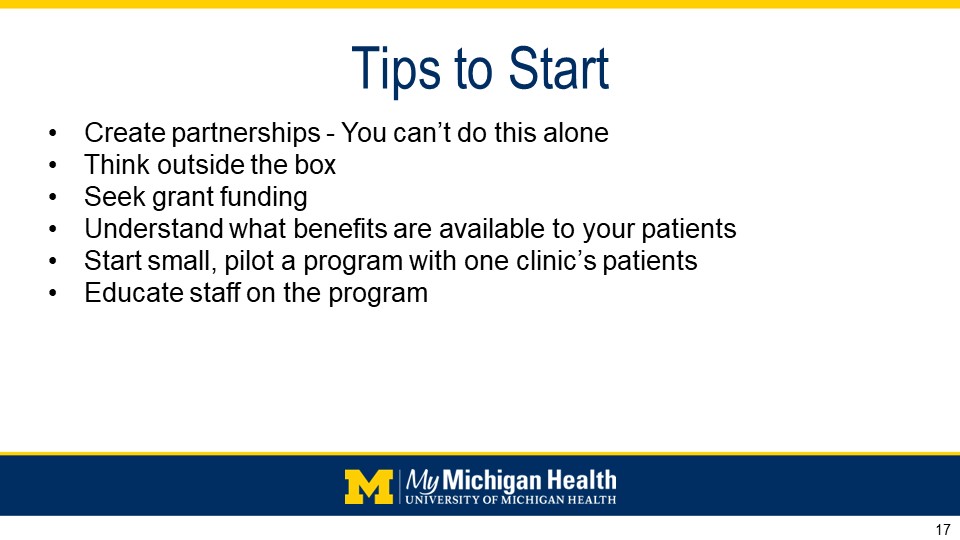
MyMichigan Medical Center Sault identified several lessons learned from delivering its Rides-to-Recovery Program over the last 10 years and applied many of those lessons to the development of its more recent Rides-to-Wellness Program. Pins also shared several tips for starting similar hospital-based transportation support programs at other locations throughout the state (Figure 3).
Those who missed the workgroup and would like to learn more about these two programs, how they are managed, and how they were developed can review the full recording here. MVC is excited to offer a new rural health workgroup series quarterly in 2024. Contact MVC if you are interested in receiving invitations to those workgroups.