Throughout February’s American Heart Month, the Michigan Value Collaborative (MVC) has and will continue to provide cardiac rehab resources and information on behalf of the Michigan Cardiac Rehab Network (MiCR). This week, MVC also shared content as part of National Cardiac Rehabilitation Week, joining other organizations across the country to promote the benefits of the program and share information on statewide initiatives. As cardiac rehab week comes to a close, MVC is proud to highlight recent activity.
The MiCR partnership was established by MVC and the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2), who have partnered in recent years to support quality improvement and innovation around cardiac rehabilitation participation. Although the strategies and initiatives have changed and expanded over time, the key goal remains: to equitably increase cardiac rehabilitation utilization among eligible patients across the state of Michigan. This week, MiCR sought to educate providers within the BMC2 and MVC collaborative about the benefits of the program, current statewide participation rates, and novel initiatives in place to support improvement.
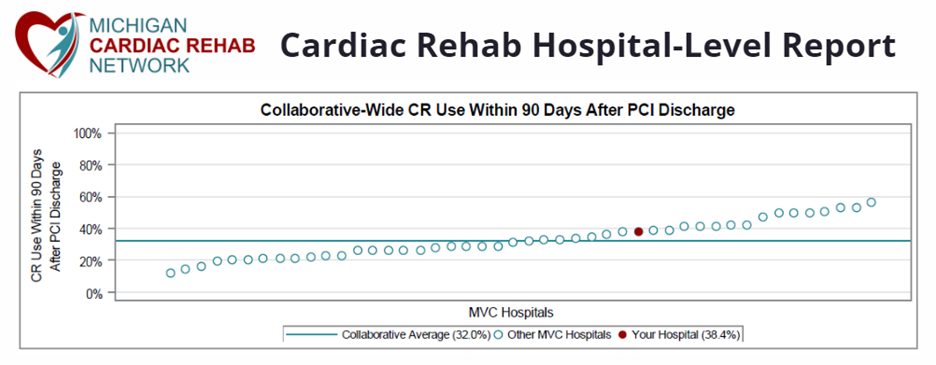
One product highlighted this week was the MiCR cardiac rehab hospital-level push reports, which benchmark cardiac rehabilitation participation across the collaborative. The 2023 report highlighted significant variation in performance and also demonstrated that several hospitals in Michigan are already successfully reaching or exceeding goals for utilization (Figure 1).
Figure 1.
Current MiCR resources, including both hospital-level cardiac rehab benchmarking reports and the MiCR Best Practices Toolkit, were designed to serve members in tracking hospital cardiac rehabilitation utilization and provide guidance to improve enrollment and adherence to the program; however, neither resource specifically investigated patient barriers to participation. To bolster successful referrals to cardiac rehabilitation in Michigan, MiCR recently partnered with Healthy Behavior Optimization for Michigan (HBOM) to launch a new program titled NewBeat. Designed to deliver heartfelt, pragmatic support to new cardiac rehabilitation patients, NewBeat is a multi-component intervention designed to address three common barriers to patient enrollment and participation: lack of education, unclear physician endorsements, and transportation access.
To address the first barrier, MiCR recently launched its website, which houses patient and provider-facing resources, MiCR event dates, and publications in one convenient location. The website already includes features such as a cardiac rehabilitation location finder and unified cardiac rehabilitation resources, but over the coming months will continue to expand.
There is research evidence that strong, personal physician referrals increase the likelihood of cardiac rehabilitation participation. For many patients, in fact, a personal referral is the only reason they sign up. Following the data, NewBeat’s second intervention component is its Cardiac Care Cards, which leverage the influence of cardiovascular providers in encouraging cardiac rehabilitation enrollment in a memorable and personal way. The cards, which can be saved and displayed on kitchen tables and refrigerators, serve as a reminder to patients that the care team understands their recovery process and supports them as they enter cardiac rehabilitation as the next step in their recovery (Figure 2). Hospitals and rehab program staff can request on the MiCR website.
Figure 2.

As the initiative continues to develop, NewBeat will grow to include patient success stories, provider-facing videos, and an informational handout on transportation resources.
One of MiCR’s key strategies in promoting the benefits of cardiac rehabilitation is fostering collaboration between providers and program staff. One of these opportunities is through an MVC workgroup series focused on cardiac rehabilitation, with the next session taking place at noon on Thurs., Feb. 22 (Figure 3). The workgroup will include a guest presentation by Devraj Sukul, MD, MSc, Co-Director of MiCR and Associate Director of BMC2 PCI. The presentation will feature recent findings about cardiac rehabilitation liaisons and their impact on patient enrollment. Register here to participate. MiCR also recently sent a save the date for its next stakeholder meeting, which will take place virtually on Fri., April 5, 10-11 a.m.
Figure 3.

MVC would like to thank everyone who contributed to Cardiac Rehabilitation Week this year. Advocating for cardiac rehabilitation continues to be a high priority for the MVC team, and the Coordinating Center is inspired by the recent growth and interest in this endeavor. Collectively, by promoting cardiac rehabilitation we can save lives and help patients in Michigan get back on their feet faster. Please contact the MVC team with any questions about attending future cardiac rehabilitation events or receiving related materials.