Serving a spectrum of functions, emergency departments (EDs) provide essential care and services, operating in the critical space between outpatient and inpatient care. EDs also serve as a safety net within the US healthcare landscape by performing necessary clinical services for populations who may not otherwise have access. Patients visiting the ED may undergo a wide range of rapid diagnostic and treatment options, ranging from unscheduled procedures, laboratory testing, utilization of basic and advanced imaging studies, and admission of patients to the hospital. Despite the ED’s critical role and services, there are few coordinated, scalable efforts to improve care quality in the ED. These realities within emergency medicine made it a prime opportunity for quality improvement (Kocher et al., 2019), which was the impetus for adding an emergency medicine-focused Collaborative Quality Initiative (CQI) to the Blue Cross Blue Shield of Michigan (BCBSM) Value Partnerships portfolio.
The Michigan Emergency Department Improvement Collaborative (MEDIC) was founded in 2015 to address the critical gap in coordinated quality improvement in the ED, including intervention design through implementation and evaluation, at scale, across health systems. Michigan Value Collaborative (MVC) members recently heard about MEDIC and its work as part of the launch of MVC’s new ED-based episodes and reporting; MEDIC and MVC collaborated on the development of this new episode of care data structure.
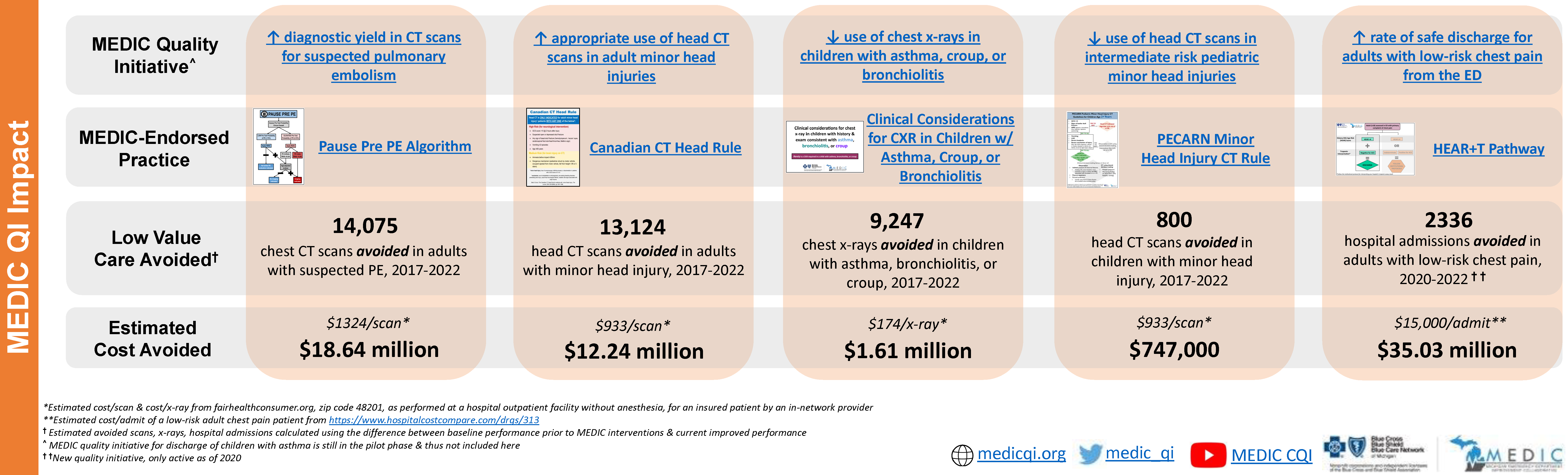
MEDIC’s quality improvement efforts to date have included initiatives such as improved appropriateness of head CT imaging utilization for children and adults with minor head injuries, greater CT diagnostic yield for adults with suspected pulmonary embolism, decreased use of chest x-rays in children with respiratory illness (i.e., asthma, croup, bronchiolitis), higher rates of ED discharge for children with asthma and adults with low-risk chest pain, and increased distribution of take-home naloxone to patients with opioid use disorder (OUD) or who experience opioid overdose or withdrawal.
MEDIC Success Stories
Since 2017, MEDIC participating sites have significantly improved collaborative-wide performance on all MEDIC quality measures. By reducing unnecessary imaging utilization and decreasing unwarranted hospitalization rates from the ED, MEDIC positively impacted the emergency care experience for thousands of patients in Michigan who received more evidence-based care and fewer low-value services. These improvements also contributed to an estimated total reduction in the ED cost burden in the millions of dollars (Figure 1).
Zach Sawaya, MD, an emergency physician at MyMichigan Medical Center, reflected positively on the benefits of partnering with MEDIC on specific quality improvement initiatives. "MEDIC has pushed our group to be more cognizant of our imaging use, in particular in the pediatric population,” he said. “We've seen significant improvements in our rates of pediatric head CTs and chest X-rays that have been driven by MEDIC-provided data and decision-making resources. In particular, we've seen wait times on pediatric head injuries go down as parents have been very open to discussion of PECARN rules and foregoing head imaging.”
The fact that MEDIC’s efforts support patients of all ages within its participating sites is unique; MEDIC is one of only a few CQIs with initiatives focused on pediatric patients. The MEDIC 2023 pay-for-performance incentive program, for example, focused on performance improvement on its pediatric-specific metrics. A key goal of this work was to ensure that children receiving emergency care in community hospital EDs received the same high-quality evidence-based care delivered in a pediatric emergency center. Since there are only three Michigan pediatric centers—all members of MEDIC—most children receive emergency care in community hospital EDs, and MEDIC observed disparities in the quality of emergency care delivered to children treated in community EDs. Children seen in community EDs were less likely to receive evidence-based care, as measured by our quality initiatives, than those seen in pediatric centers. In an emergency, patients can’t often choose which ED to go to, rather they need to go to the closest option. Over time and with participation in MEDIC, the data indicate MEDIC community hospitals improved their collective performance on MEDIC pediatric measures to be nearly on par with that of pediatric specialty hospitals.
The COVID-19 pandemic and its resulting impact on EDs also put MEDIC in a unique position. Within days of the pandemic being declared in the US, the MEDIC team pivoted from its standard work to support the COVID-19 response by leveraging its collaborative-wide learning network to support frontline efforts. MEDIC rapidly assembled a platform for informal and formal discussion between member EDs, which manifested as a series of virtual town halls and Grand Rounds focused on information exchanges among colleagues to rapidly innovate and meet challenges as the situation evolved.
This series began with lessons learned from the experience of its southeast Michigan EDs where the pandemic first unfolded in Michigan. This allowed sites in other areas of Michigan to understand what they would likely experience in the coming weeks or months, giving them valuable preparation time. Over several weeks, these well-attended sessions focused on the following topics: conservation of PPE, management of COVID-19 respiratory failure, special considerations for the pediatric population, and supporting the wellness of the ED workforce.
MEDIC – ED Partnerships
EDs partner with MEDIC in two primary ways: data collection and collaborative engagement in quality improvement. To participate in MEDIC, a partner ED must establish a flow of electronic health data for all ED visits to the MEDIC data registry as well as provide additional abstracted data, facilitated by a data abstractor hired with support from BCBSM. This then allows MEDIC to provide detailed evaluation and performance reporting on all measured quality initiatives, which in turn helps facilitate and inform site quality improvement interventions. MEDIC provides member hospitals with a level of insight into their ED practice patterns that would not be possible without participating in the collaborative.
In addition to being able to understand their data, participating in MEDIC allows hospitals to learn from one another, which significantly shortens the learning curve for improvement. Each site’s emergency medicine physician champion and abstractor(s) lead local intervention design and implementation, participate in MEDIC tri-annual collaborative-wide meetings, and share experiences and lessons learned with collaborative peers. MEDIC provides quality improvement evidence, guidelines, standardized performance measurement, data visualization, evaluation, and support for local intervention efforts.
MEDIC currently partners with hospital EDs across the state. Any sites not currently partnered with MEDIC are encouraged to visit their recruitment page for more information on becoming a member and contacting the team.
As MVC continues to build its offerings for members, the coordinating center is cognizant that hospitals and providers partner with multiple CQIs. MVC posts regular blogs about some of its peer CQIs to showcase their activities and highlight collaborations with MVC. Please reach out to the MVC Coordinating Center with questions.