Urological surgery quality improvement is essential for enhancing patient outcomes, ensuring safety, optimizing healthcare costs, and strengthening overall healthcare system performance. To foster patient trust, reduce outcome variation, and drive continuous advancements in urological surgery practices, the Michigan Urological Surgery Improvement Collaborative (MUSIC) was established in 2011.
One of Michigan’s 21 Collaborative Quality Initiatives (CQIs) operating in partnership with Blue Cross Blue Shield of Michigan (BCBSM), MUSIC is a physician-led CQI comprised of a consortium of 44 urology practices (academic, private practice, community) across the state of Michigan, as well as four out-of-state practices. Designed to evaluate and improve the quality and cost efficiency of urologic care, MUSIC aims to improve patients’ lives by inspiring high-quality care through data-driven best practices, education, and innovation.
The initial focus of MUSIC was improving care for patients diagnosed with or at risk of prostate cancer. The earliest quality improvement (QI) initiatives MUSIC undertook focused on decreasing infectious complications following prostate biopsies and decreasing unnecessary imaging for patients with low-risk prostate cancer. Both efforts were very successful with post-biopsy infectious hospitalizations decreasing from 1.1% in 2013 to 0.2% in 2024 and unnecessary bone scans and computed tomography (CT) scans decreasing from 13% and 15% in 2012 to 5% and 4% respectively in 2018. MUSIC has also conducted four randomized clinical trials, two completed and two in-progress, utilizing the MUSIC infrastructure. Since its formation, MUSIC expanded its focus from prostate cancer (MUSIC-Prostate) to a program focused on kidney stones (MUSIC-ROCKS) in 2016 and small kidney tumors (MUSIC-KIDNEY) in 2017, with a plan to begin a new program on benign prostatic hyperplasia (BPH) in the fourth quarter of 2025 (Figure 1).
Figure 1: Michigan Urological Surgery Improvement Collaborative Programs
MUSIC Achievements
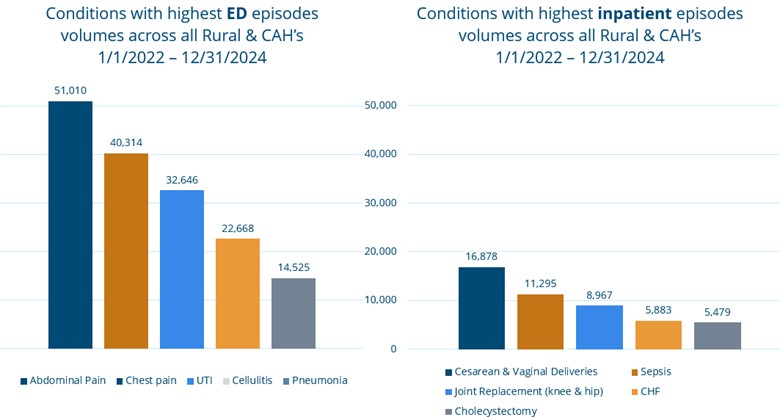
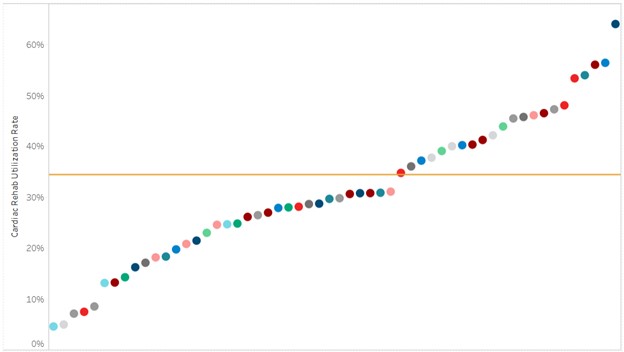
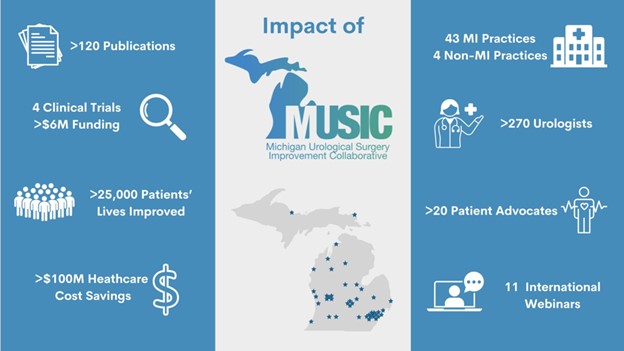
Over the last 14 years, MUSIC has made significant strides in urological care and surgical quality, achieving milestones that greatly advanced the field (Figure 2). Through MUSIC’s efforts, active surveillance (AS) for patients with low-risk prostate cancer – which involves monitoring prostate cancer in its localized stage until the doctor feels that further treatment is needed to halt the disease at a curable stage – increased from about 40% in 2018 to about 80% in 2024. Post-ureteroscopy emergency department (ED) visits, another area of focus, decreased from about 10% in 2016 to about 8% in 2024.
Figure 2: Impact of MUSIC
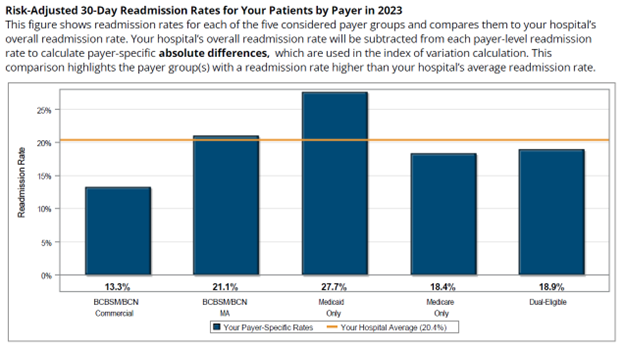
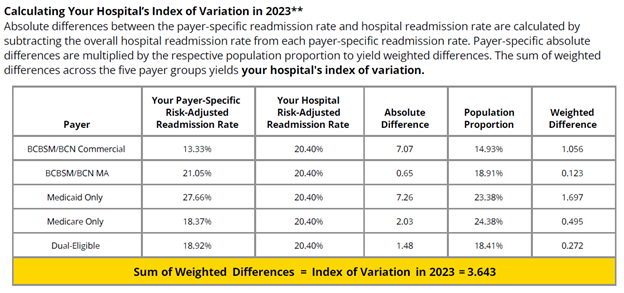
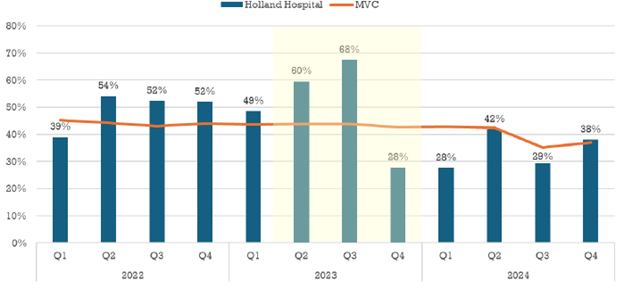
MUSIC initiatives also made a significant impact on the use of evidence-based guidelines for prescribing opioids after surgery. Between 2016 and 2024, the use of opioid prescriptions after kidney stone surgery dropped from about 80% to about 15%. The Michigan Value Collaborative (MVC) helped assess the impact and value of MUSIC's opioid initiatives within both the ROCKS and Prostate programs, resulting in a MUSIC-ROCKS value assessment in 2022 and a MUSIC-Prostate value assessment in 2023 (Figure 3). These MUSIC initiatives had a major impact on opioid prescribing in Michigan, helping to reduce the availability of unused opioids in the community and mitigate their potential for misuse. MVC and MUSIC frequently collaborate on analytic projects and exercises that help evaluate ongoing initiatives as well as identify opportunities for QI in the future.
Current MUSIC Initiatives
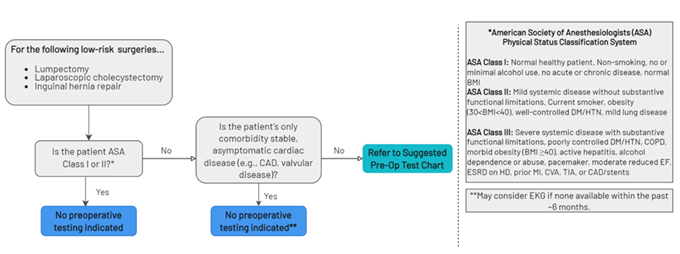
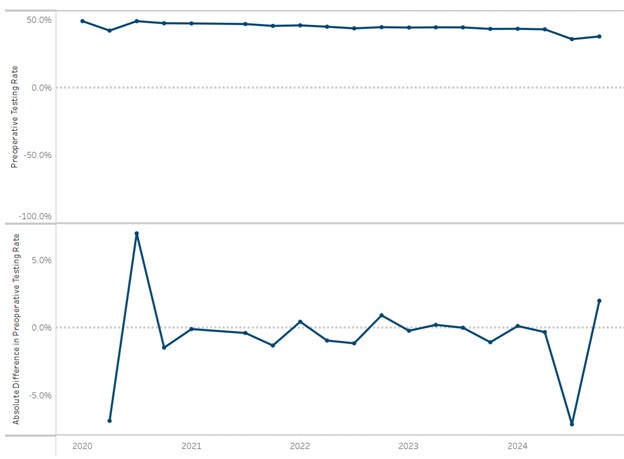
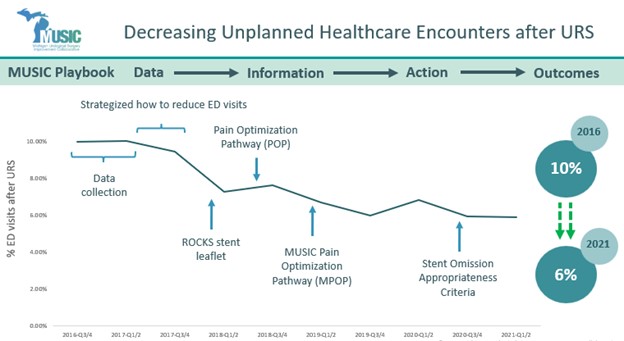
Active surveillance for prostate cancer patients continues to be a goal with additional focus on ensuring patients on AS receive proper follow-up testing. MUSIC aims to build on the successes of previous initiatives by developing updated recommendations for type and frequency of follow-up testing and conducting urologist and primary care physician (PCP) education and feedback reporting. An area of focus for MUSIC’s ROCKS program includes decreasing post-ureteroscopy infectious complications and ED visits after kidney stone surgery. To achieve these goals, MUSIC is developing more specific recommendations for pre- and post-operative antibiotic use, providing better patient education, using non-opioid post-operative pain management, and decreasing the use of ureteral stents (Figure 4).
Figure 4: Decreasing Unplanned Healthcare Encounters after Ureteroscopy (URS)
Services and Benefits for MUSIC Members
MUSIC hosts multiple collaborative-wide meetings and workshops each year to support its ongoing mission to improve urologic care. Other ways MUSIC supports its initiatives and advances QI is by conducting annual site visits to urologists, other providers, and hospitals to review their performance across various metrics, offer provider education, and discuss opportunities for improvement to ensure all patients in Michigan have access to the same quality of care. MUSIC members also receive support for American Board of Urology maintenance of certification.

For patients, MUSIC provides patient education materials that build trust and help improve outcomes, which are often developed with direct input from patients. When asked to comment on the patient education materials and MUSIC program, MUSIC Patient Advocate James Humphries said,
“Guidance provided by my urologist and the MUSIC materials allowed me to make an informed treatment decision regarding my kidney mass and confidently select active surveillance. I am grateful for the continuing opportunity to participate in MUSIC collaborative meetings and provide commentary on patient educational materials. I sincerely believe other patients will benefit if this document is shared. Ultimately, I attribute my improved health and successful surgical outcome to these collaborative efforts.”
MVC is proud to partner with MUSIC in advancing urological care across Michigan. The BCBSM-funded CQIs play a crucial role in driving healthcare quality improvement, and MVC is excited to continue showcasing the innovative contributions of individual CQIs and the ways in which MVC’s data support high-value care initiatives across the portfolio. Please reach out to MVC by email if you are interested in learning more.