Michigan Value Collaborative data and efforts were on display this week as Coordinating Center staff attended the Learning Health System (LHS) Collaboratory Seminar Series Poster Session on Thursday and the Michigan Bariatric Surgery Collaborative (MBSC) / Blue Cross Blue Shield of Michigan 2022 Obesity Management Summit on Friday. At each event, MVC was able to highlight some of its recent work.
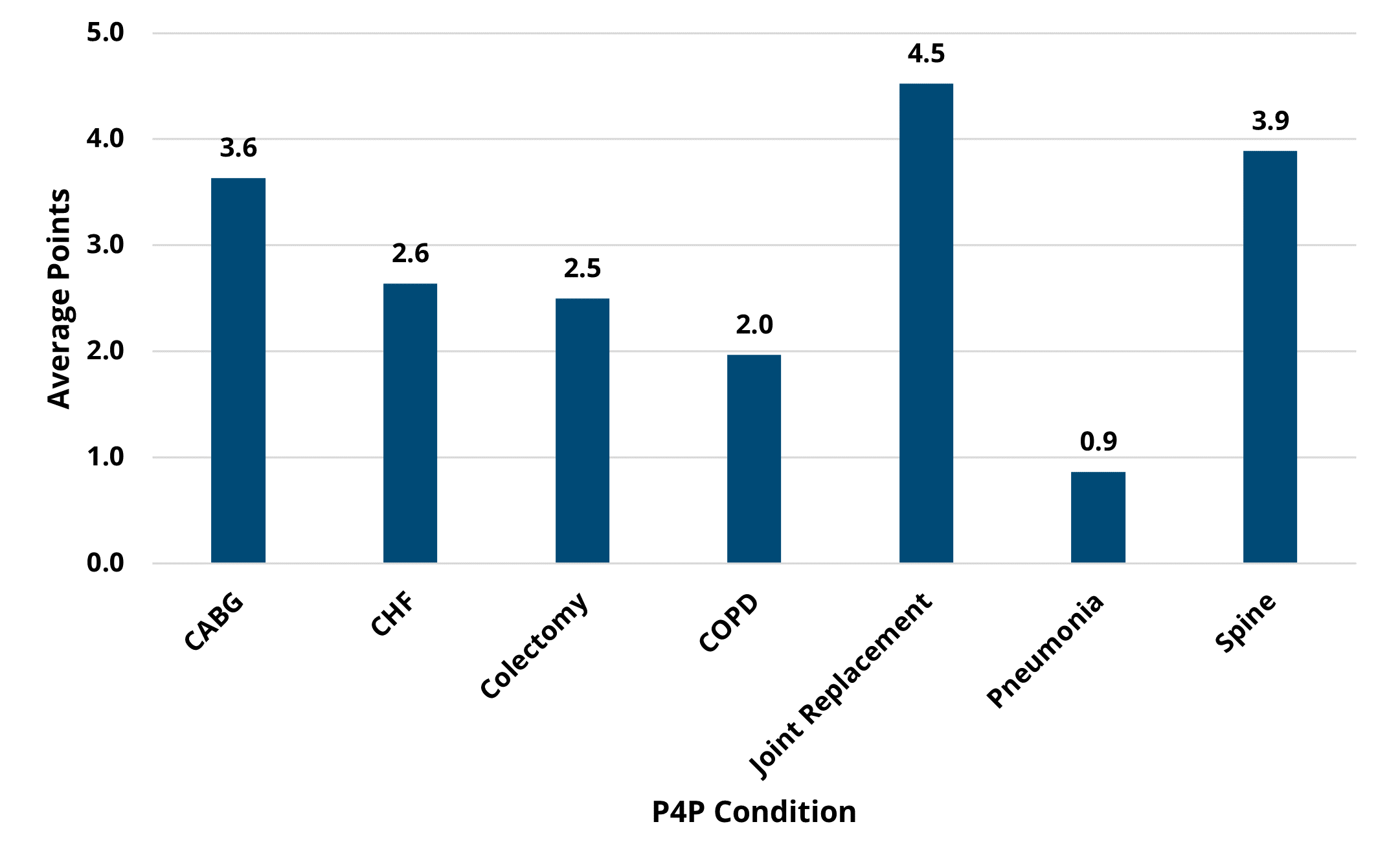
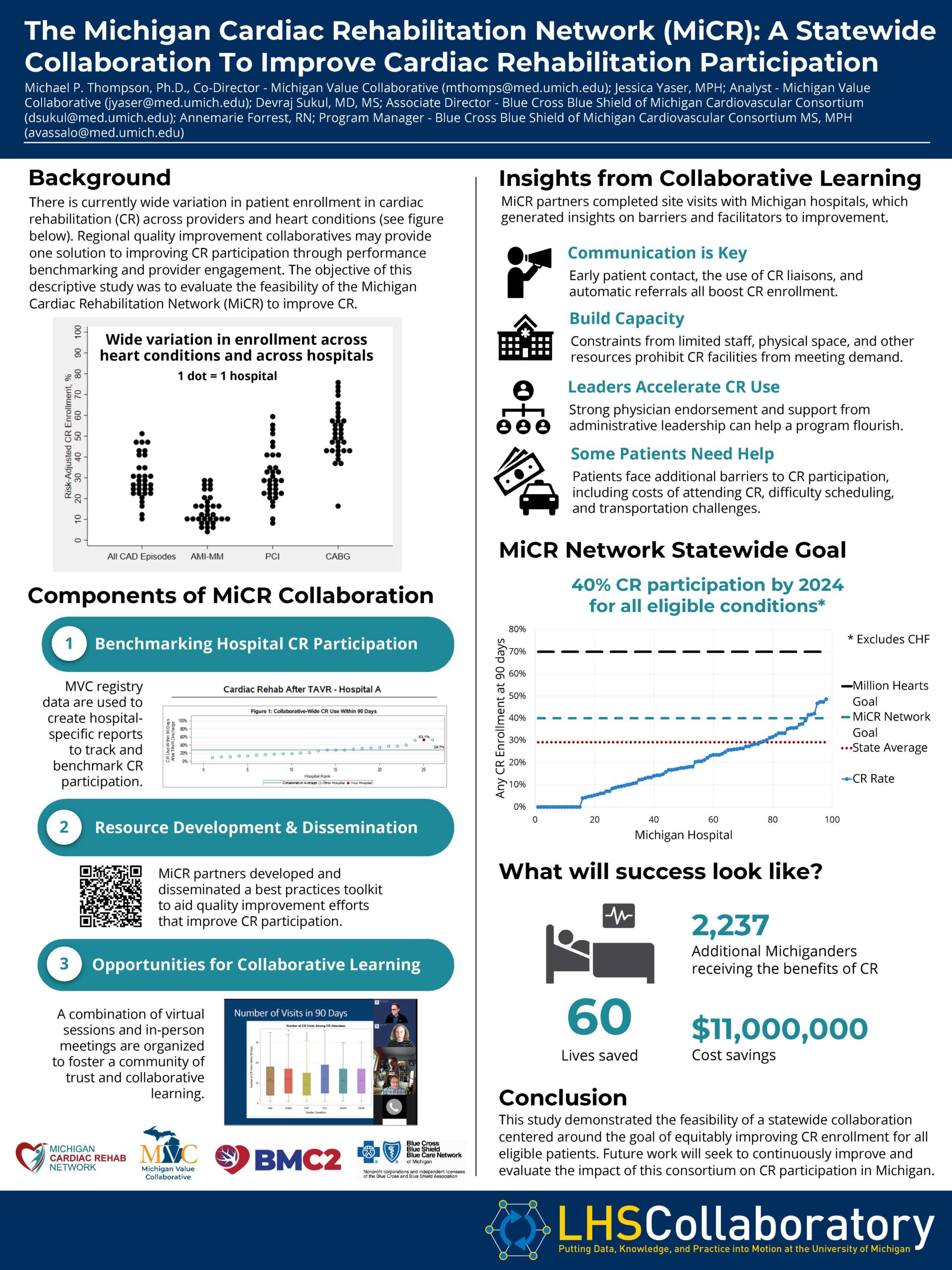
At the LHS Collaboratory poster session, MVC presented on behalf of the Michigan Cardiac Rehabilitation Network (MiCR), a partnership recently established by MVC and the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2) with the aim to equitably increase cardiac rehabilitation participation for all eligible individuals in Michigan. Cardiac rehabilitation is highly beneficial to patients and cost-saving for the healthcare system, yet it is significantly underutilized in Michigan with only about 30% of eligible patients enrolling following a cardiac procedure. Using claims data, MVC can assess whether and when someone enrolls, and how long they keep going. There is wide variability in enrollment between MVC’s member hospitals as well as across cardiac conditions. The focus of the poster (see Figure 1) was a recent publication co-authored by MVC and BMC2 staff, which evaluated the feasibility of a statewide collaboration to improve cardiac rehabilitation participation. The poster summarized the key services provided by the MiCR collaboration and some of the lessons learned thus far about barriers to and facilitators of improvement. It also promoted the new statewide goal of 40% cardiac rehabilitation participation by 2024 for all eligible conditions - a goal set by MVC and BMC2. More details on this statewide goal and MiCR’s activities are summarized here.
Figure 1.
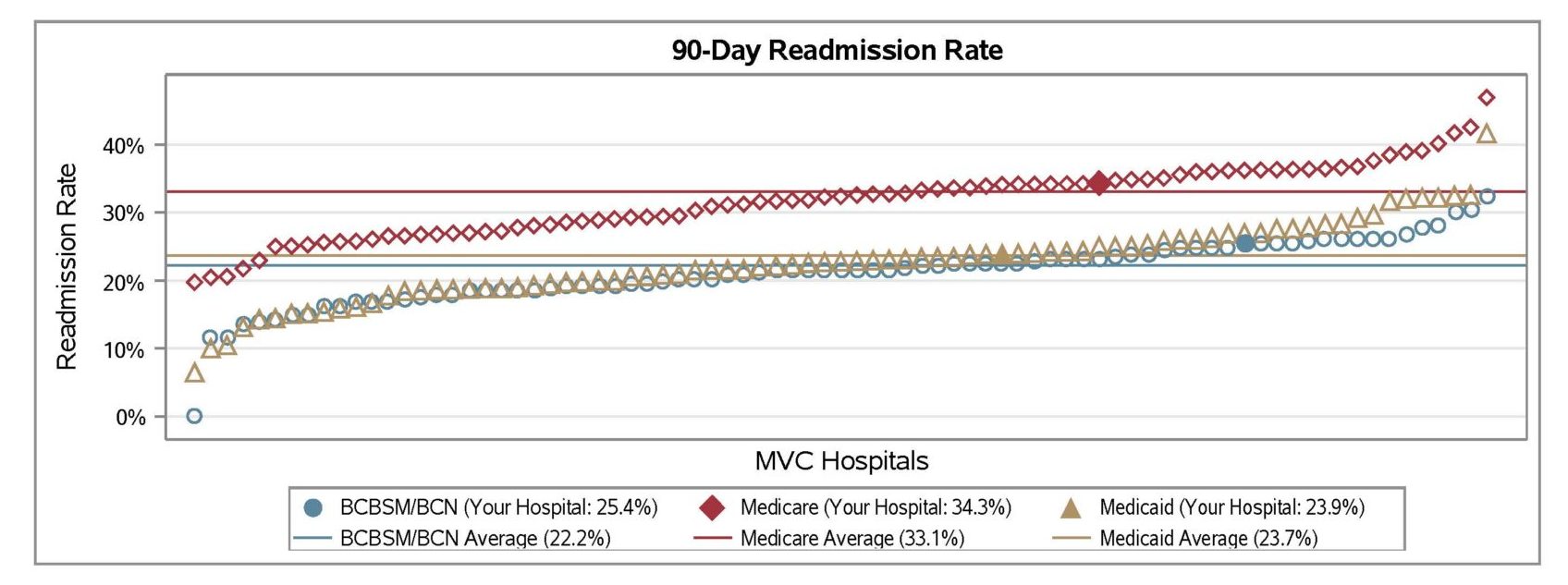
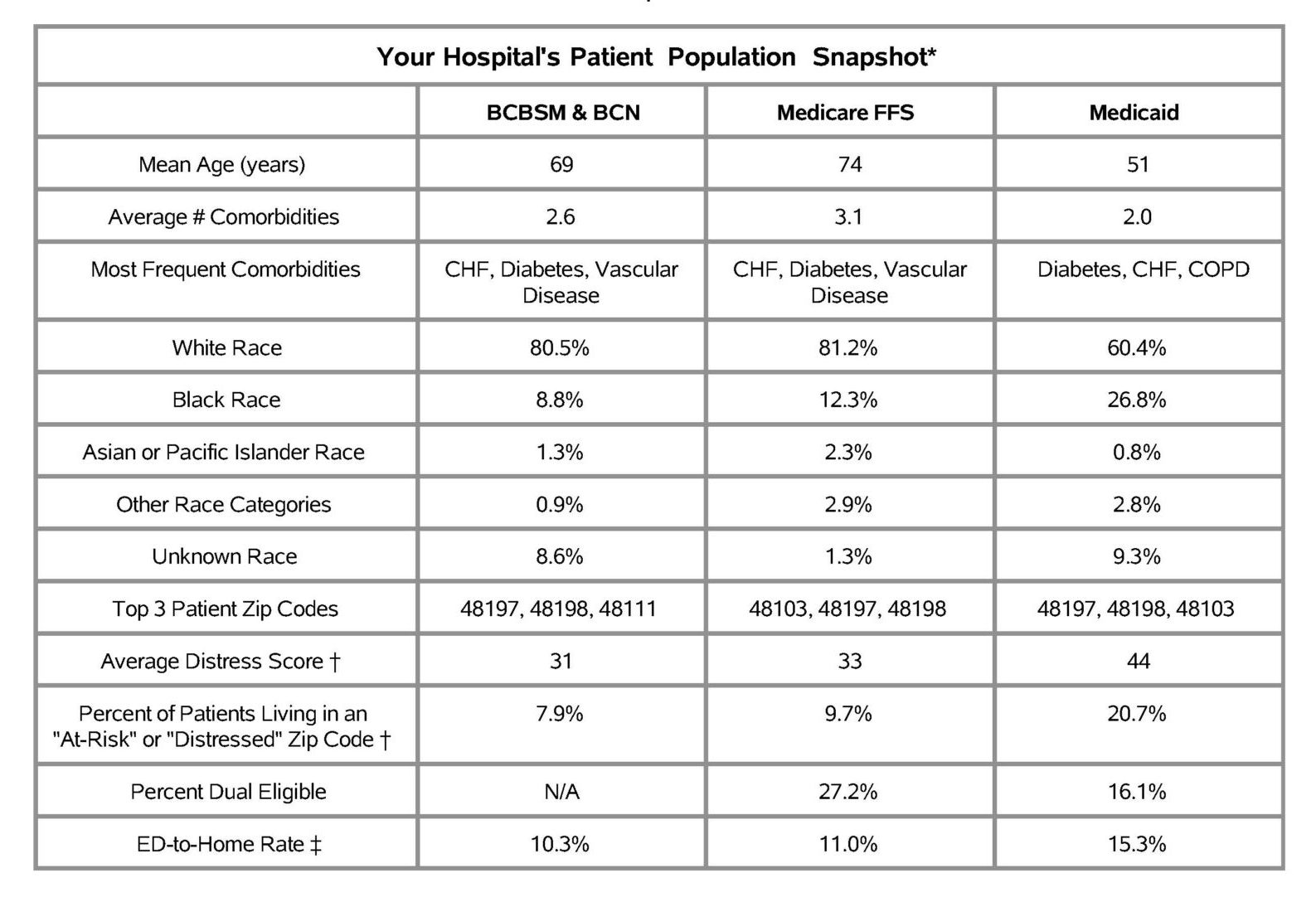
For Friday’s Obesity Summit, several MVC products were on display, including two recent analyses performed in partnership with MBSC. The two CQIs recently collaborated on a statewide improvement assessment about the impact of bariatric surgery on prescription fills for diabetes medications. Much of the evidence in the literature suggests that bariatric surgery may resolve or improve Type 2 diabetes symptoms in a large proportion of patients. MVC used its claims data to compare pre- and post-surgery receipt of diabetes medications, as well as the estimated cost savings to health insurance providers that could be attributed to a decrease in post-surgery diabetes medication prescription fills. There was a significant decrease in prescription fills for any diabetes medication (p<.001) from the 120 days pre-surgery to the 120 days post-surgery (see Figure 2).
Figure 2.
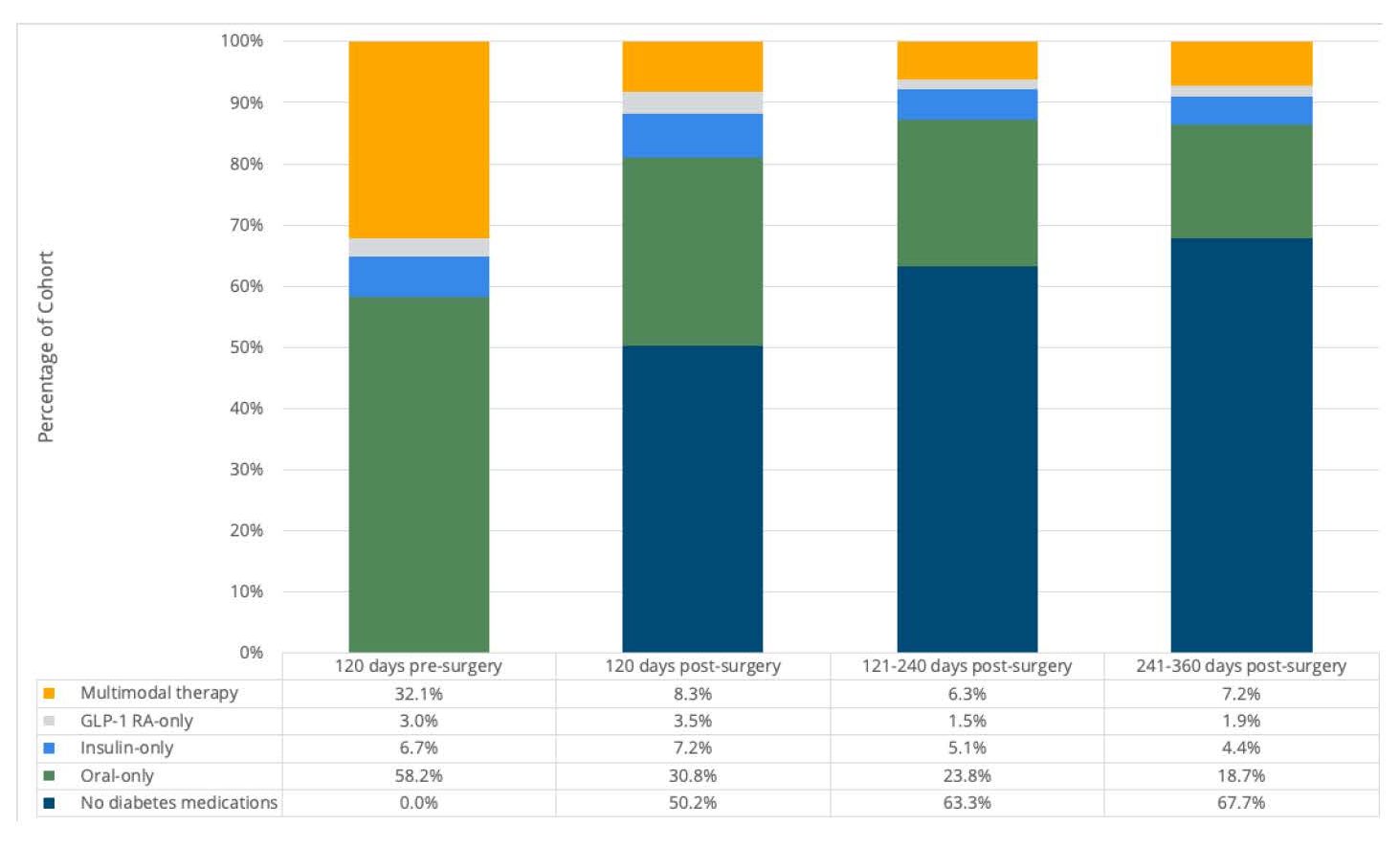
Furthermore, insurance providers in Michigan saved an estimated $76.5 million on diabetes medications in the 360 days following bariatric surgeries in 2015-2021, based on the average decrease in diabetes prescription payments per patient, the number of bariatric surgeries performed in that timeframe, and the proportion of bariatric surgery patients who have diabetes. These results provided evidence of statewide clinical outcome improvement and cost savings for Type 2 diabetes patients following bariatric surgery. The full summary of this analysis is available here.
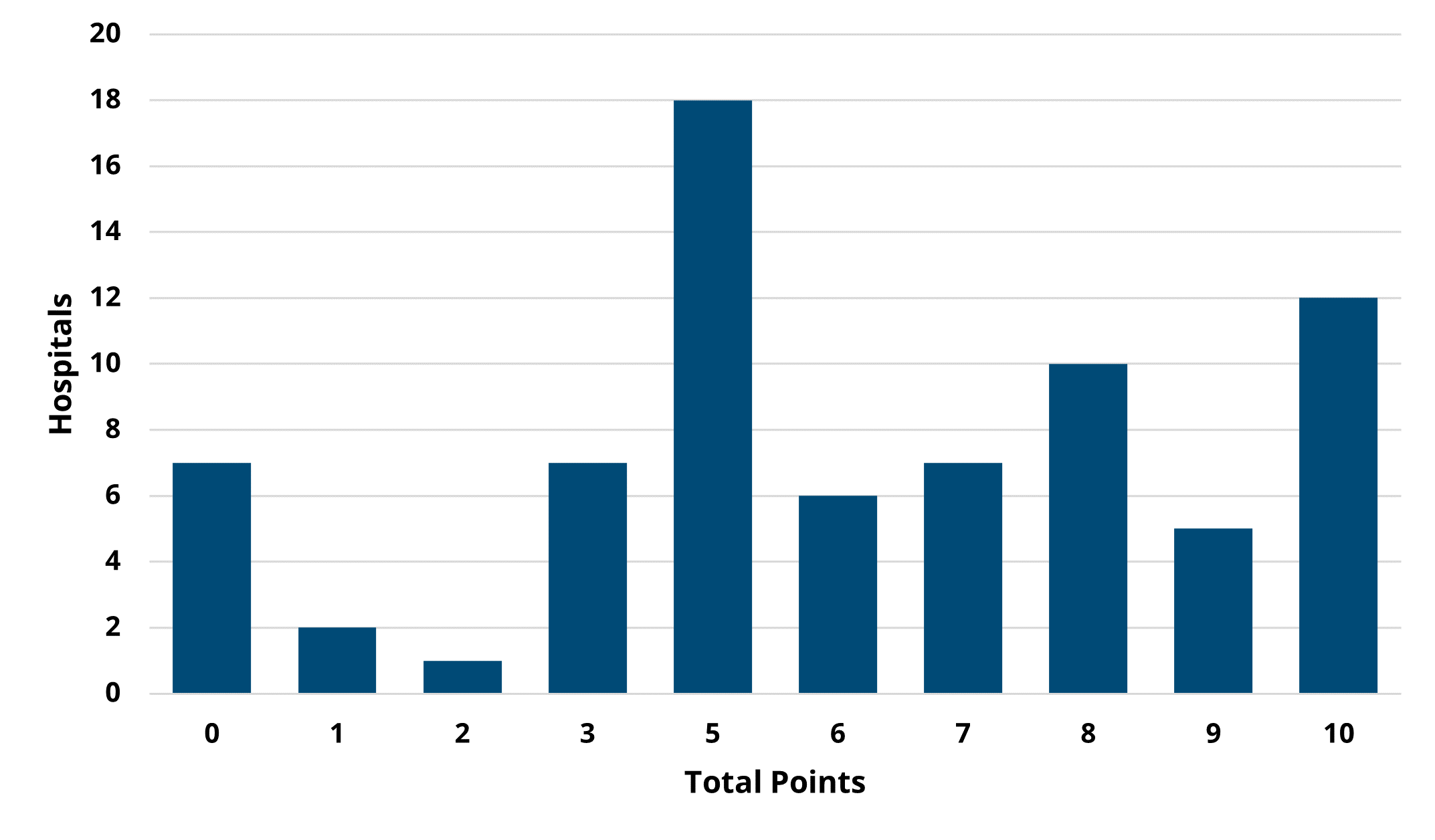
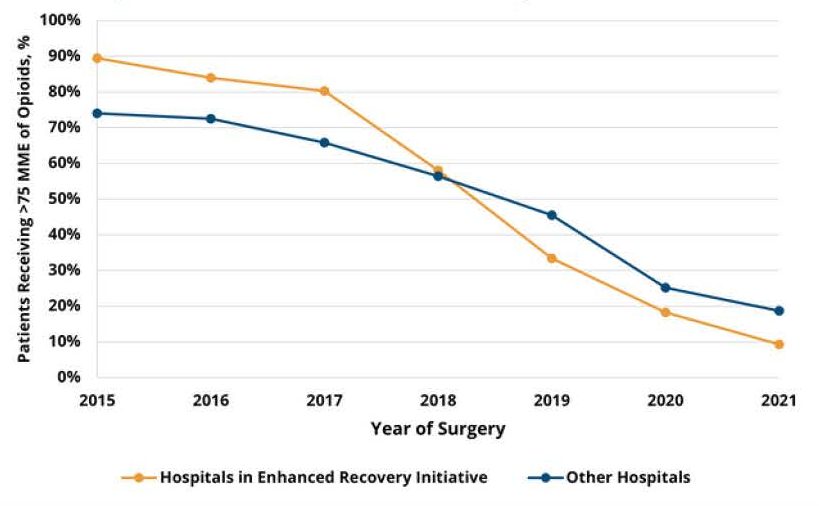
MVC partnered with MBSC on a similar analysis of opioid medication use that was also highlighted at the 2022 Obesity Summit. MBSC has been working to reduce opioid utilization and prescribing following bariatric surgeries across Michigan for the past five years. Some of their strategies include an opioid value-based metric and a voluntary enhanced recovery initiative that incorporates evidence-based guidelines for pre-, peri-, post-operative, and post-discharge care of bariatric surgery patients. This includes a recommendation of prescribing no more than 75 morphine milligram equivalents (MME) of oral opiate following surgery - a recommendation consistent with surgery-specific guidelines set by the Michigan Opioid Prescribing Engagement Network (OPEN).
In evaluating the impact of MBSC’s opioid reduction work, analysts identified that the average amount of opioids received in 30-day post-surgery outpatient prescriptions decreased from 297.0 MME in 2015 to 65.4 MME in 2021. The percentage of patients receiving more than the recommended threshold of 75 MME decreased from 75.8% to 17.9% of bariatric surgery patients. Furthermore, hospitals that participated in MBSC’s enhanced recovery initiative saw the rate of patients receiving opioid amounts above 75 MME decrease more sharply than the rate at other hospitals (p=0.02) (see Figure 3). Given these findings, MVC estimated that MBSC’s efforts resulted in $12.5 million in cost savings because of reduced opioid prescribing after bariatric surgery. The full summary of this analysis is available here.
Figure 3.
MVC will continue to leverage its robust claims data to further the goals of fellow Collaborative Quality Initiatives as well as MVC member hospitals and physician organizations. To stay informed about newly released analyses, resources, or projects, follow MVC Coordinating Center updates on Twitter or LinkedIn. To learn more about these projects or MVC’s reporting capabilities, contact the Coordinating Center at michiganvaluecollaborative@gmail.com.