Prior to surgery, most Michigan patients will undergo a series of tests, such as blood draws, urinalysis, chest x-rays, or electrocardiograms (ECGs/EKGs). Many of these tests are unnecessary for healthy patients undergoing low-risk procedures such as groin hernia repair. Routine preoperative testing is widely considered a low-value service, and yet a majority of hospitals continue to order these tests. In an effort to drive improvement in this area, MVC hosted its second annual preoperative testing awareness campaign this week.
“For a patient, it is key they get the right amount of preoperative assessment,” said Dr. Michael Englesbe, professor of surgery at the University of Michigan, director of the Blue Cross Blue Shield of Michigan-funded Collaborative Quality Initiatives, director of the Michigan Surgical Quality Collaborative (MSQC), and co-director of the Michigan Opioid Prescribing and Engagement Network (Michigan OPEN). “Too little testing and important risks may be missed, too much and patients may be exposed to critical risks of unnecessary testing and delays in care.”
MVC’s Coordinating Center supports preoperative testing de-implementation in several ways. One is providing opportunities for MVC’s members to collaborate and learn from one another. This year MVC launched a workgroup series focused on preoperative testing, the first of which took place in March. As part of its campaign this week, MVC promoted the next session in this workgroup series, set to take place Tues., Aug. 1, from 1-2 p.m. featuring guest speaker Nick Berlin, MD, MPH, MS. Those interested in this topic should register to attend here.
Another key strategy MVC uses to support preoperative testing de-implementation is through data analysis and reporting. MVC analysts utilize administrative claims data to calculate testing rates in the preoperative period, and then share these results with members as reports or as unblinded data at collaborative-wide meetings. More recently, MVC partnered with MSQC to distribute these reports more widely to support cross-collaboration between clinical and quality personnel at a given site.
These reports are an invaluable resource in benchmarking the extent of the issue statewide, says Dr. Hari Nathan, MVC’s director and the chief of hepato-pancreato-biliary surgery at Michigan Medicine. “MVC data can be used by hospitals and providers to understand how their rates of preoperative testing compare to those of other hospitals in Michigan,” he said. “By focusing on a homogeneous cohort of healthy patients undergoing common, low-risk surgical procedures, MVC benchmarks can help all hospitals understand where they have an opportunity to improve, regardless of facility size, resources, or patient population.”
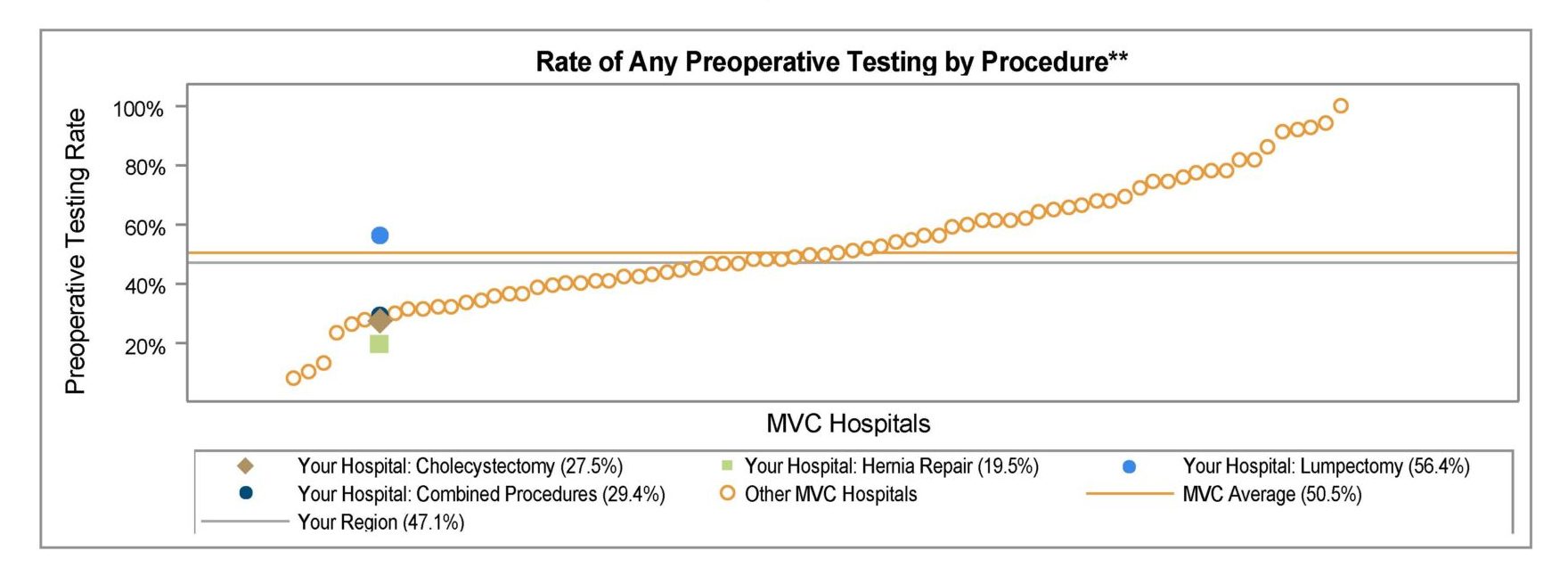
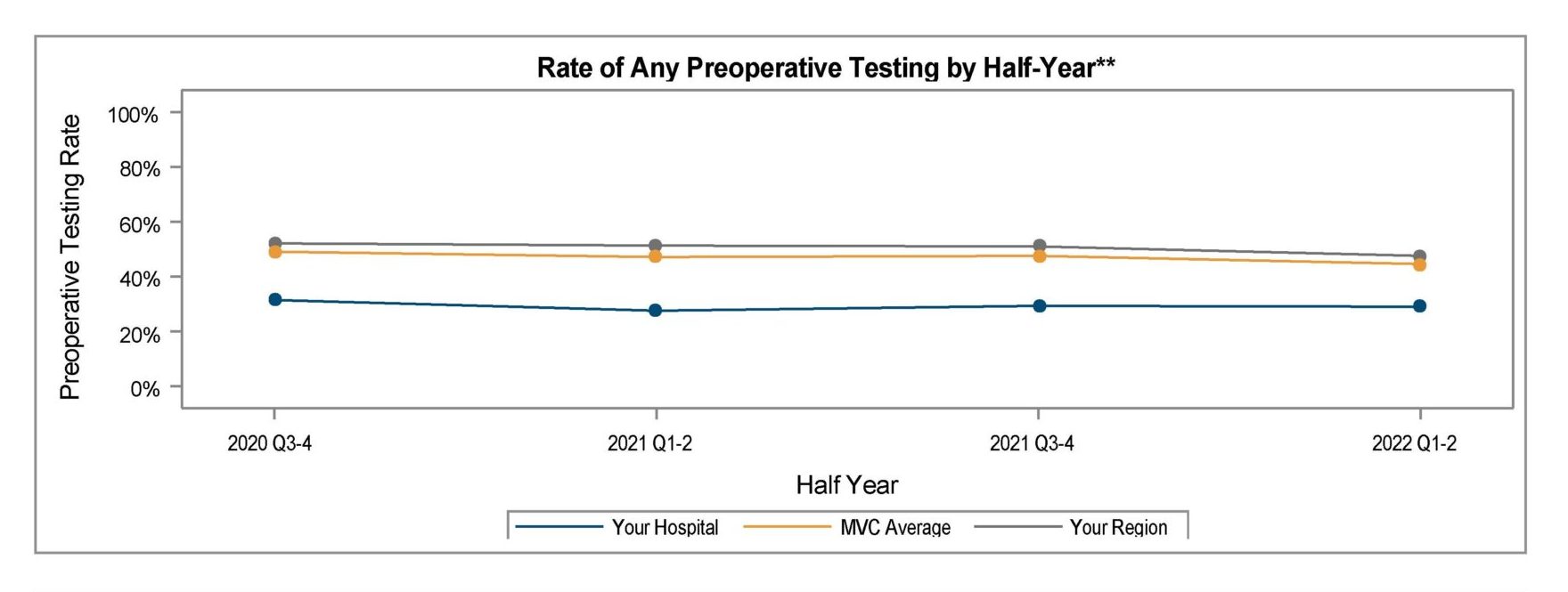
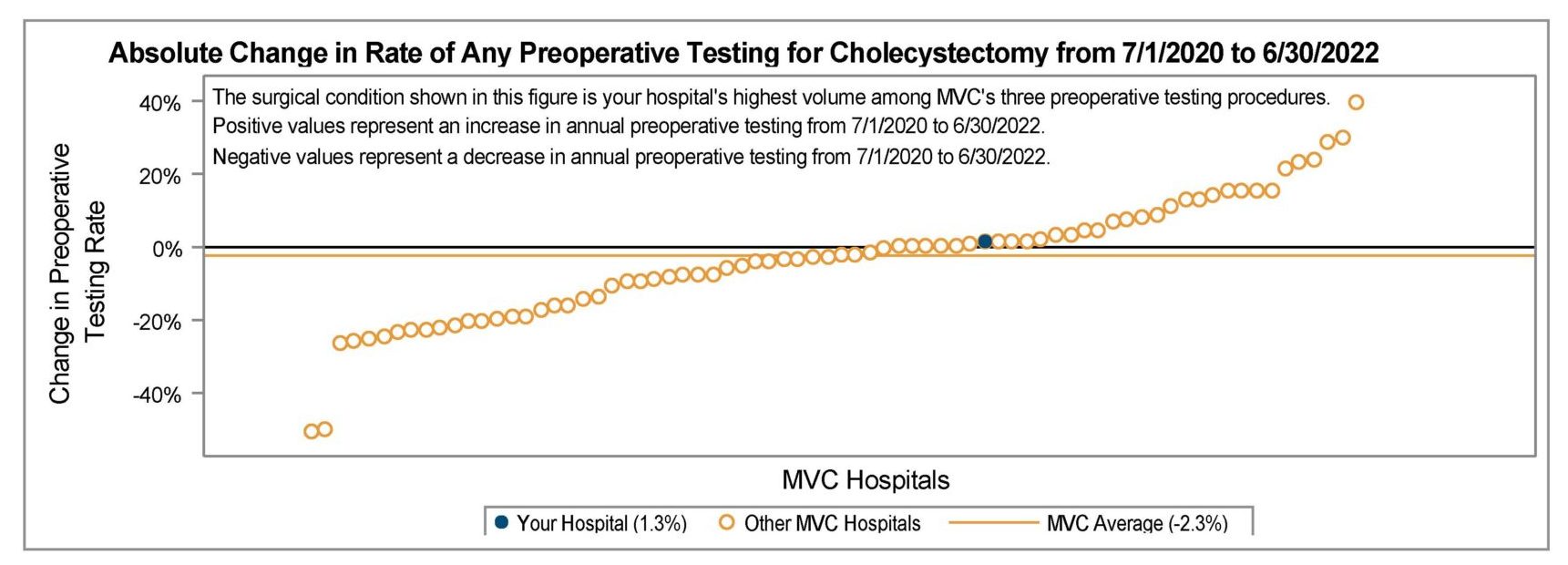
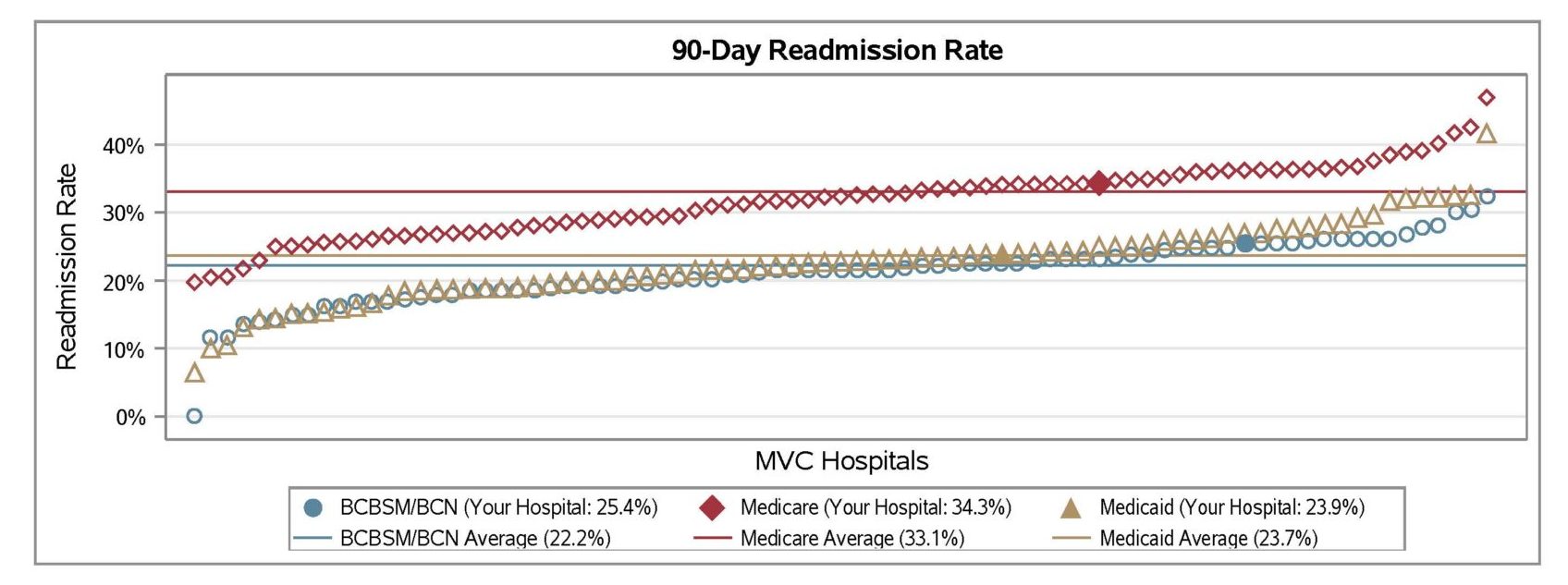
Across the collaborative, MVC sees wide variation in preoperative testing for low-risk elective surgeries like hernia repairs and lumpectomies, with testing rates among young, healthy patients ranging from 10% to 97% across MVC hospitals. This level of interhospital variation is evidence that many hospitals in Michigan are safely performing low-risk surgeries without widespread preoperative testing and that even those hospitals with average rates likely have room to safely reduce their testing further.
MVC also sees quite a bit of intrahospital variation, with certain surgeries driving the overall preoperative testing rate at a given site. Based on the findings of its latest report, one potential area of focus for sites may be reducing the rate of cardiac testing; the rate of ECGs is quite variable across the collaborative and could lead to a cascade of care.
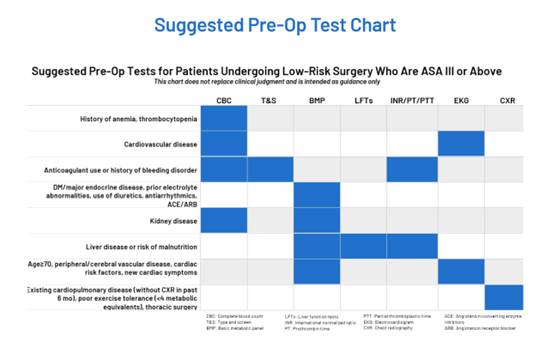
MVC shared its refreshed preoperative testing push report with members in April and also held a report review webinar in June to review the measures included. This webinar also included advice from Dr. Nathan about how to take action using this data. Dr. Nathan promoted several new resources developed in partnership by MSQC, the Michigan Program on Value Enhancement (MPrOVE), and MVC. These include a customizable decision aid (Figure 1), which sites can download to add their branding or modify. It is accompanied by a similarly customizable preoperative testing reference chart (Figure 2).
Figure 1.
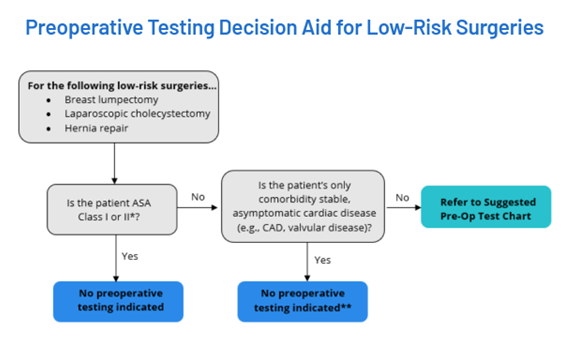
Figure 2.
Both of these resources are currently housed on a new Waive the Workup de-implementation resource website managed by MPrOVE, MSQC, and MVC. In addition to pages for the decision aid and chart, the site also offers talking points for debunking common myths about preoperative testing. For instance, one common counterargument to reducing preoperative testing prior to low-risk surgery is a perception that there’s no harm in ordering them, either because they are relatively inexpensive or because they are not invasive tests.
On the contrary, research has established substantial financial costs and risks to patient harm because of preoperative testing, which can and should be safely reduced. Mihir Surapaneni, BBA, a medical student at the University of Michigan Medical School, has been conducting research with MVC on preoperative testing and its impact. “One of the major theories for why there’s so much variability—and indeed just a high utilization rate—for preoperative testing is that there’s no perceived downside,” Surapaneni said. “Many of these tests are relatively cheap compared to the total cost of healthcare and indeed most of them cost no more to the patient than a stick of blood, but we really have to consider that there are costs. Preoperative testing costs billions of dollars in the United States healthcare system annually, and when you consider how strained the healthcare system is and how much of an onus there is on payers and the government to decrease costs, this really adds up. And secondly, we have to consider the possibility of testing cascades—which has been well-documented—in that a patient comes in having an abnormal lab value or test that actually had nothing to do with their intended surgery, and this leads to more and more tests which are expensive and potentially invasive. And finally, we have to consider that there’s established literature showing that even when an abnormality is found in a routine preoperative test, these abnormalities: 1) rarely impact the clinical course of the patient, and 2) rarely lead to actual substantive change in that patient’s care. And I think that we really have to consider these when we’re deciding whether or not we want to test our patients routinely.”
In addition to registering for the Aug. 1 workgroup, MVC has a third preoperative testing workgroup session scheduled for Oct. 26, 11 a.m. - 12 p.m. The Oct. session will be a forum for sharing current successes or initiatives underway across the collaborative. If your hospital has a current initiative underway on preoperative testing de-implementation or has a low average testing rate, MVC would love to learn from you. Please reach out to the MVC team if you’d be interested in sharing your site’s story on Oct. 26.