This week the Michigan Value Collaborative (MVC) introduced a new push report for its physician organization (PO) members focused on chronic obstructive pulmonary disease (COPD), providing a tailored version for each of MVC’s 40 PO members. This new push report was created in response to member interest in improving the quality of care for chronic diseases. It utilized 30-day claims-based COPD episodes from Medicare Fee-For-Service, Blue Cross Blue Shield of Michigan (BCBSM) PPO Commercial, and BCBSM Medicare Advantage with index admissions from 1/1/19 to 6/30/21.
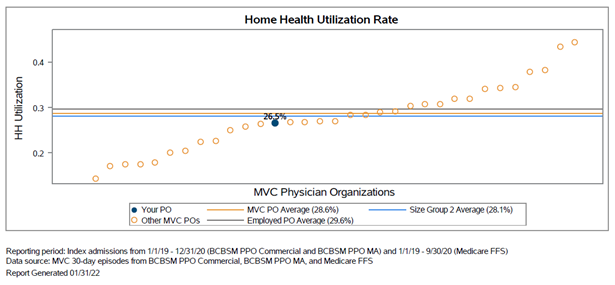
One feature the MVC Coordinating Center is excited to highlight is the inclusion of 30-day readmission rates by major comorbidity categories for COPD. Rates were assessed for a PO’s attributed COPD patients overall as well as for attributed patients with congestive heart failure, diabetes, and vascular disease (see Figure 1). These comorbidities are assessed using diagnosis codes on claims in the six months prior to the patient’s index hospitalization.
Figure 1.
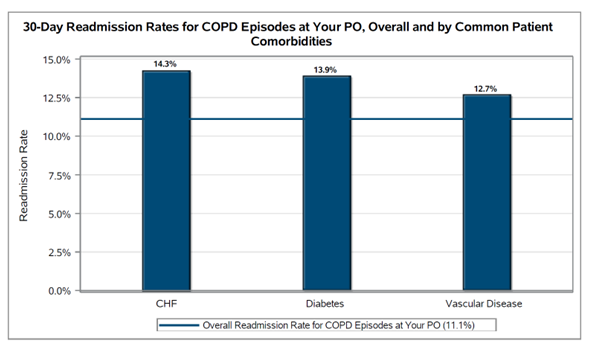
Also featured in this report were 90-day rates of pulmonary rehabilitation utilization following COPD index hospitalizations. This is the first time MVC has included a measure of pulmonary rehabilitation utilization in a collaborative-wide report, and the Coordinating Center hopes that this metric will encourage increased use of this important program across Michigan. Across all COPD episodes in the report, the collaborative-wide rate of pulmonary rehabilitation for PO-attributed patients was 2.7% (see Figure 2).
Figure 2.
Due to the low collaborative-wide rate, the Coordinating Center assessed 90-day utilization of pulmonary rehabilitation rather than 30-day utilization. However, the American Thoracic Society recommends the initialization of pulmonary rehabilitation within three weeks following hospitalization. Click here to learn more about American Thoracic Society recommendations for pulmonary rehabilitation and other care following COPD hospitalization.
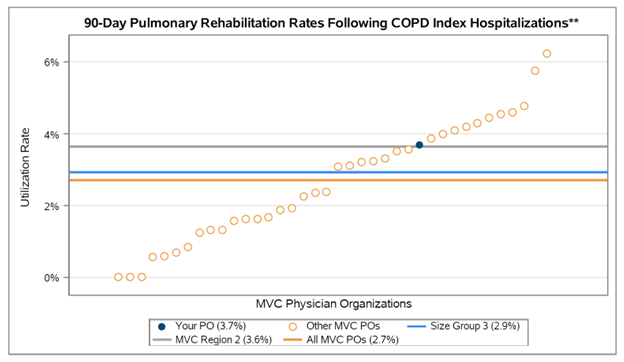
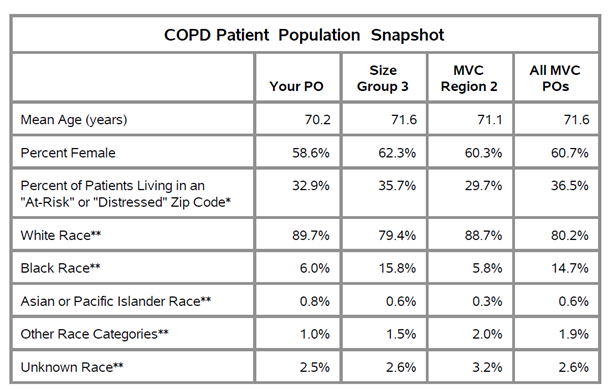
Each PO’s complete report also includes figures illustrating average price-standardized risk-adjusted 30-day total episode payments, average index hospitalization length of stay, trends in readmission rates, rates and payments of post-acute care utilization, rates of outpatient follow-up, and patient population demographics. A patient population snapshot table details several demographic variables, including a variable based on data from the Economic Innovation Group’s Distressed Communities Index (DCI). It identifies the proportion of patients living in an “at-risk” or “distressed” zip code across all payers (see Figure 3). The DCI is derived from the U.S. Census Bureau’s Business Patterns and American Community Survey.
Figure 3.
A second table provides information on index hospital locations of care for the PO’s attributed patients, comparing the percent of patients treated at each site as well as each index hospital’s average 30-day total episode payment.
The COPD PO report is also being shared with members of the newly established lung care Collaborative Quality Initiative, commonly referred to as INHALE (Inspiring Health Advances in Lung Care). INHALE focuses on patients with asthma and COPD. They disseminate strategies to improve outcomes in these patient populations and reduce the costs associated with asthma/COPD care.
MVC also partnered with a fellow Collaborative Quality Initiative to provide POs with a provider resource that may be relevant to their work with COPD patients. The Healthy Behavior Optimization for Michigan (HBOM) team provided its Quit Smoking Resource Guide to send alongside MVC’s report. HBOM aims to ensure that all smokers who are interested in quitting receive the support and resources they need to be successful. Read more about HBOM’s materials and efforts on the HBOM website or in MVC’s May spotlight blog.
If you have any suggestions on how these reports can be improved or the data made more actionable, the Coordinating Center would love to hear from you. MVC is also seeking feedback on how collaborative members are using this information in their quality improvement projects. Please reach out at Michigan-Value-Collaborative@med.umich.edu.