The MVC Coordinating Center will soon distribute refreshed hospital-level versions of its push report utilizing emergency department-based episodes (“ED-based episodes”). MVC generated separate versions for acute care hospitals and Critical Access Hospitals (CAHs) with tailored comparison groups. In addition to reflecting more recent data across all included payers, these refreshed hospital-level reports differ from prior versions due to the addition of three high-volume ED conditions and the incorporation of Michigan Medicaid claims.
Each page of the report is dedicated to a specific condition with the same metrics throughout, such as risk-adjusted, price-standardized 30-day total episode spending, inpatient admission rates, and rates of post-ED utilization. Reports feature each hospital’s own attributed ED-based episode data for eight high-volume ED conditions: abdominal pain, cellulitis, chest pain (nonspecific), congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD), diabetes with long-term complications (including renal, eye, neurological, or circulatory), diabetes with short-term complications (including ketoacidosis, hyperosmolarity, or coma), and urinary tract infection (UTI). The three new conditions included in this year’s refresh include diabetes with long-term complications, diabetes with short-term complications, and UTI.
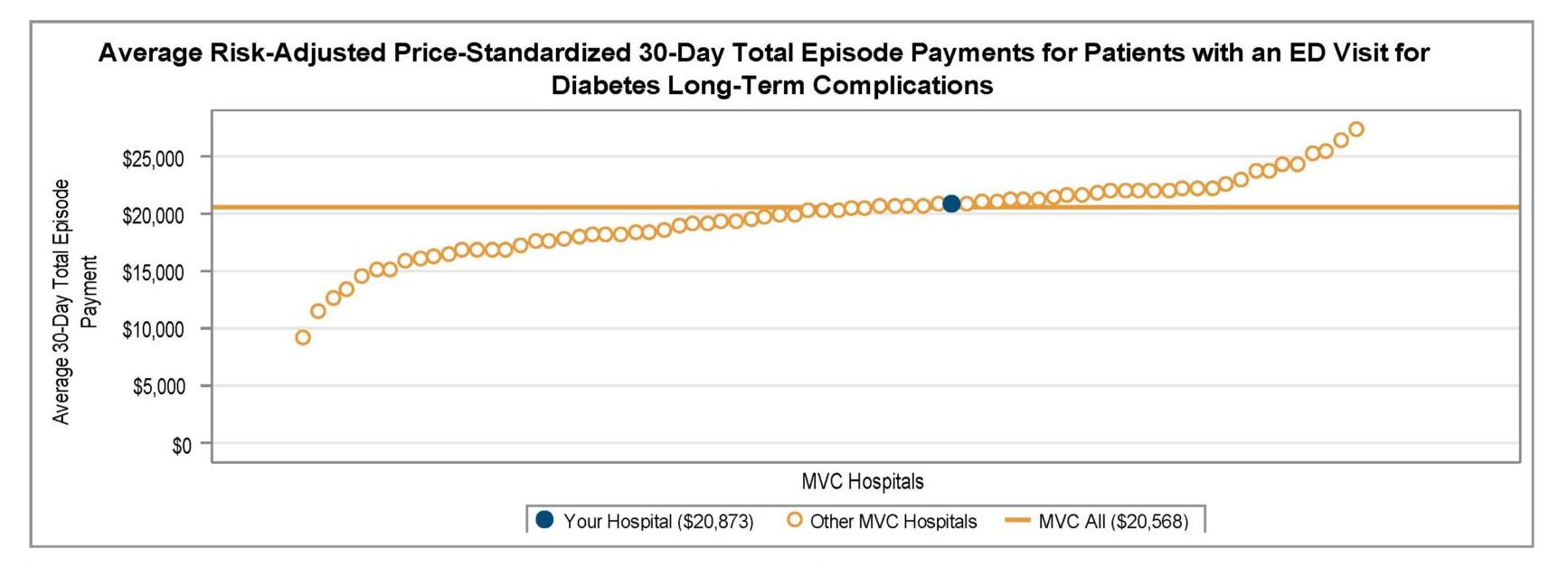
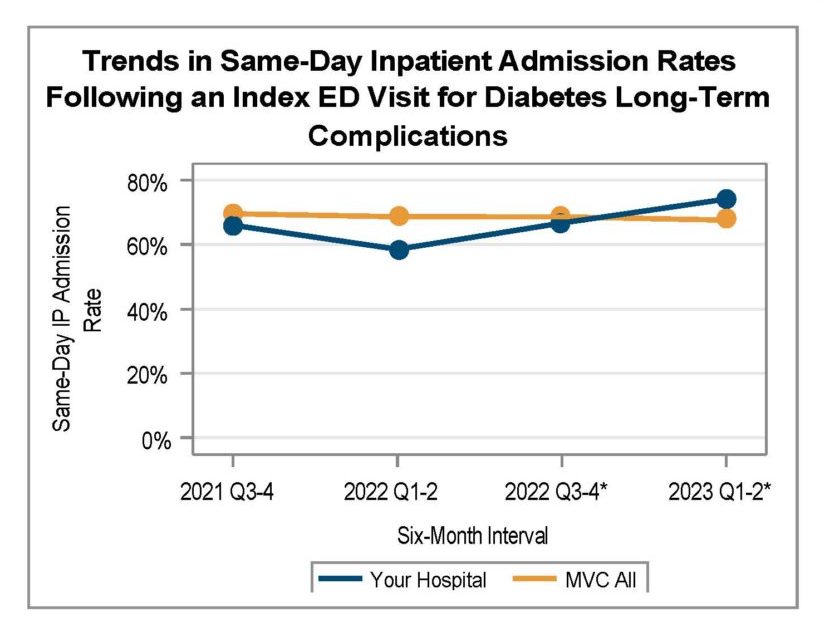
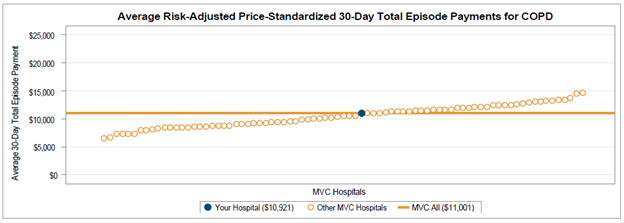
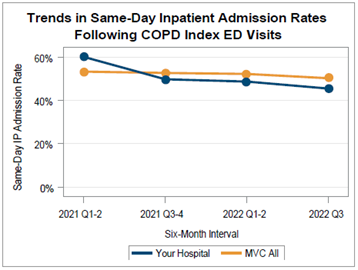
Among general acute care hospitals receiving a report, the average risk-adjusted, price-standardized 30-day total episode payment (Figure 1) for the reported conditions is highest for diabetes with long-term complications ($20,568), CHF ED-based episodes ($17,245), diabetes with short-term complications ($12,087), and COPD ED-based episodes ($10,289). The collaborative-wide average is lowest for chest pain ($3,111) and abdominal pain ($3,123) ED-based episodes. Within each condition, MVC 30-day total episode payments are consistently higher for episodes in which the patient had a same-day inpatient admission compared to episodes in which the patient did not have an inpatient stay beginning on the date of their ED visit. With that information in mind, hospital members can also use their individualized reports to track their same-day inpatient admission rate at six-month intervals using trend graphs for each included ED-based condition (Figure 2).
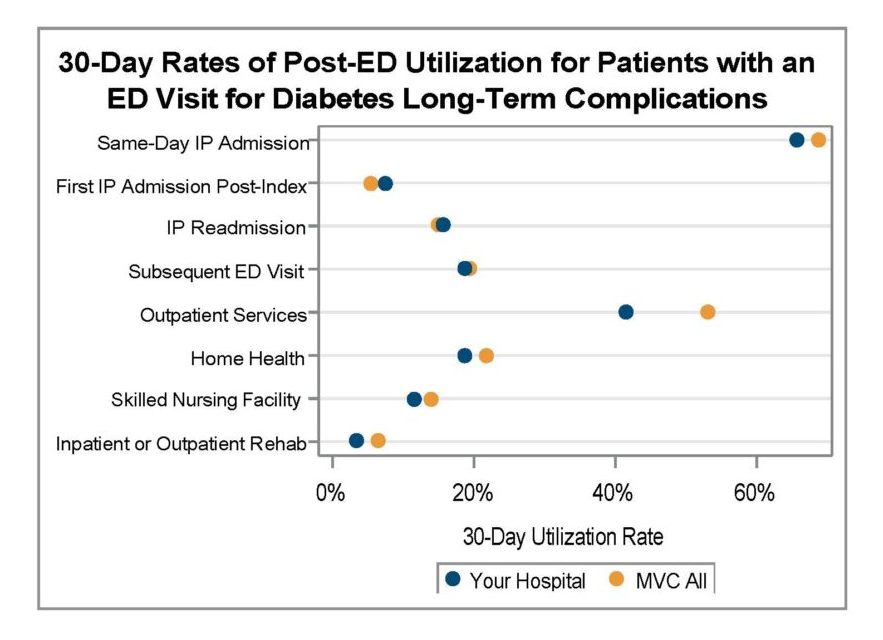
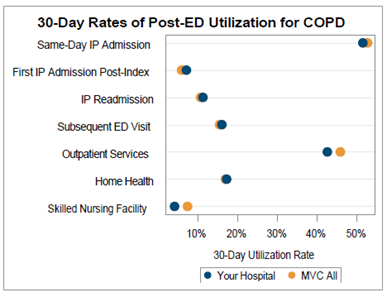
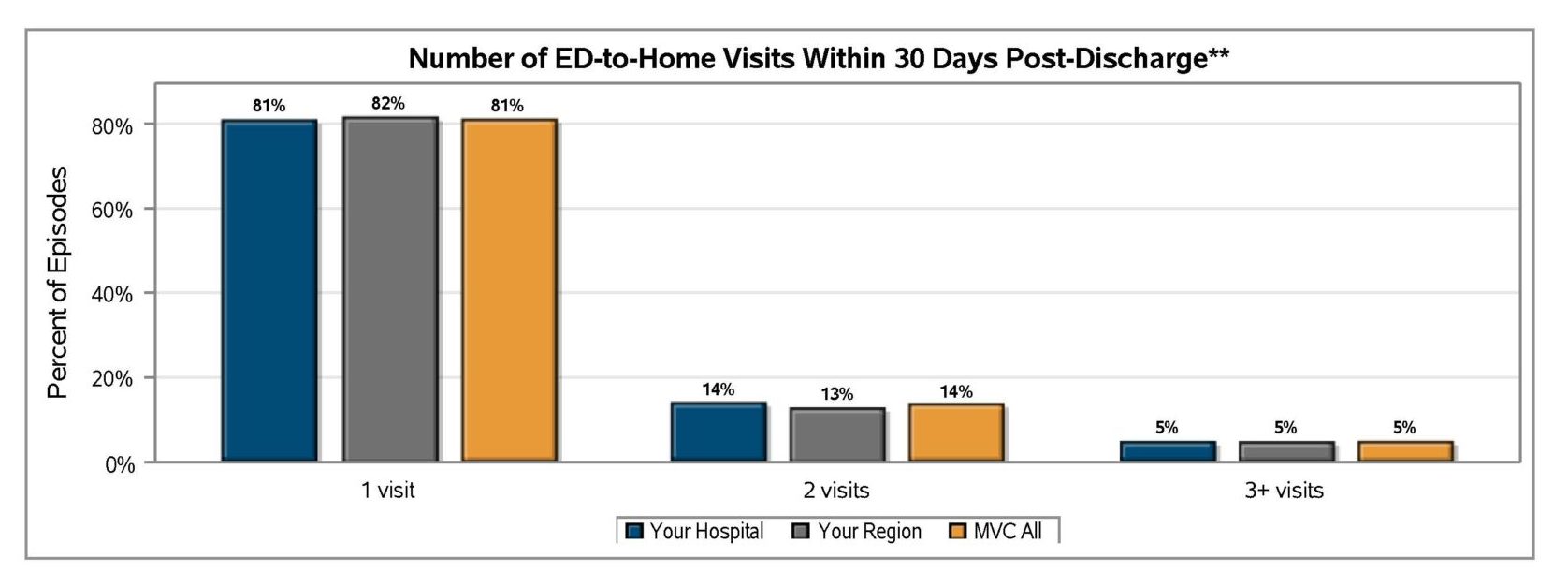
A key goal for these ED-based episode reports is to provide insight into healthcare utilization following index ED visits. Therefore, reports continue to include a dot plot (Figure 3) comparing patient post-ED utilization at a member hospital against their peer comparison group. Dot plots provide information on what percent of episodes had a same-day inpatient admission, what percent did not have a same-day inpatient admission but did see the patient admitted in the 1 to 30 days following the index ED visit, and the percent of patients who had two or more inpatient admissions (thus, at least one readmission) during the episode of care. Also provided are rates of subsequent ED visits, receipt of outpatient services, home health, skilled nursing facility care, and inpatient or outpatient rehab.
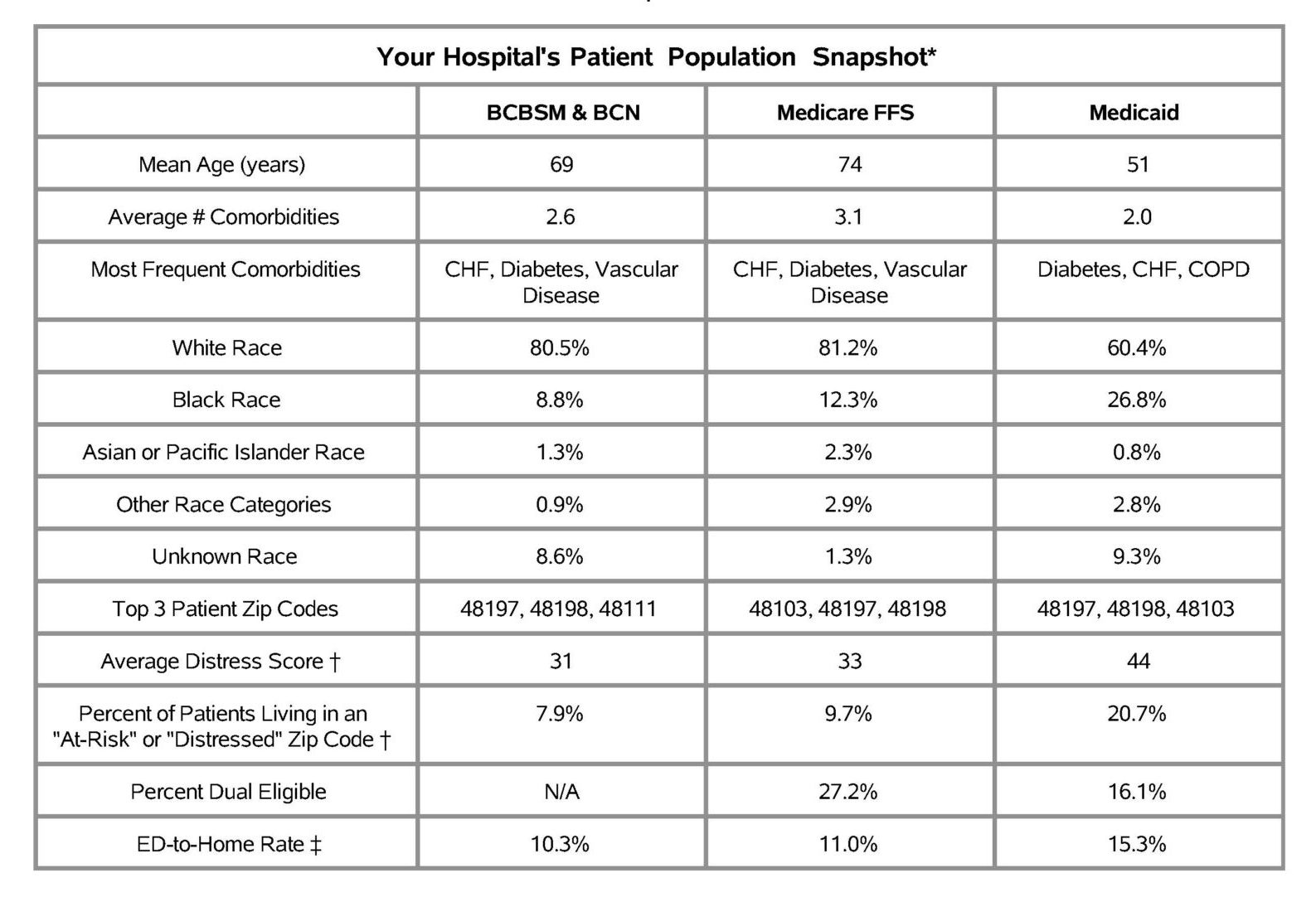
These ED-based episodes are built using MVC’s most recent medical claims data from Medicare FFS, Blue Cross Blue Shield of Michigan PPO Commercial and Medicare Advantage plans, Blue Care Network HMO Commercial and Medicare Advantage plans, and Michigan Medicaid.
ED-based episodes utilize MVC’s newest episode of care data structure, which was developed last year in collaboration with the Michigan Emergency Department Improvement Collaborative (MEDIC), a BCBSM-funded Collaborative Quality Initiative with the goal of improving care and patient outcomes in Michigan emergency departments. MVC and MEDIC team members worked closely to develop 30-day episodes of care initialized by a patient’s visit to the ED and including all claims-documented care received in the 30 days following a patient’s index ED visit.
Please share your feedback with the MVC team if certain report measures are helpful or if you wish to see additional ED-based episode reporting for certain conditions and metrics. MVC is now also accepting custom report requests using its new ED-based data. Contact MVC to learn more.