Last week, the Coordinating Center distributed a refreshed version of MVC’s common conditions report. This report delivers a comprehensive analysis of care episodes for eight prevalent medical and surgical conditions frequently targeted for quality improvement initiatives within MVC hospitals. It assesses hospital performance and highlights potential areas for growth. The report’s current conditions include atrial fibrillation (A-Fib), chronic obstructive pulmonary disease (COPD), colectomy (non-cancer), congestive heart failure (CHF), coronary artery bypass graft (CABG), percutaneous coronary intervention (PCI), pneumonia, and sepsis. Notably, total knee and hip (joint) replacement, which was previously included, has been replaced by A-Fib in the latest report.
MVC generated reports for 96 eligible hospitals. General acute care hospital (GACH) and Critical Access Hospital (CAH) members received tailored versions of the report, which included benchmark data specific to their respective hospital categories and tailored comparison groups. A blinded version of the general acute care hospital report is available here.
Although the provided metrics and figures vary by condition and case count, report pages generally focus on 30-day total episode payments, post-acute care and post-discharge ED utilization, readmission rates, and common reasons for readmissions. The report has been updated to feature data covering the period of January 1, 2023, through December 31, 2024, for Blue Cross Blue Shield of Michigan (BCBSM)/Blue Care Network (BCN) Commercial, BCBSM/BCN Medicare Advantage (MA), and Michigan Medicaid; Medicare FFS data covers the period of January 1, 2023, through June 30, 2024.
Upon opening the latest report, MVC members will first find a summary of patient population demographic data for each condition/procedure category their hospital was eligible to receive, facilitating a comprehensive and effective comparison across service lines for a variety of non-medical drivers of health.
On subsequent condition or procedure pages, most hospitals will have a figure displaying the breakdown of 30-day risk-adjusted, price-standardized post-acute care payments by payer categories (see Figure 1). The categories available included BCBSM/BCN Commercial, BCBSM/BCN Medicare Advantage, Medicare Only, Medicaid Only, and Dual Eligible; hospitals received data points for those payer categories with at least 11 episodes during the reporting period. As a reminder, the “Dual-Eligible” category represents patients eligible for both Medicare and Medicaid coverage, and the separate Medicare and Medicaid categories do not include those patients when the separate Dual-Eligible category is included.
Figure 1.
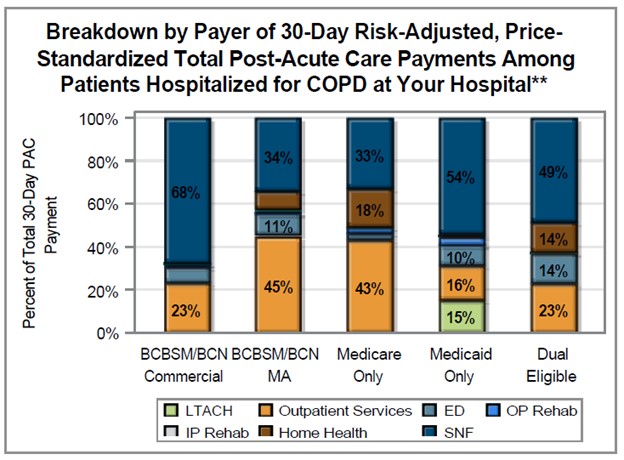
**Information is presented only for those payer categories that have at least 11 episodes during reporting period. Missing data labels represent less than 9% of the total.
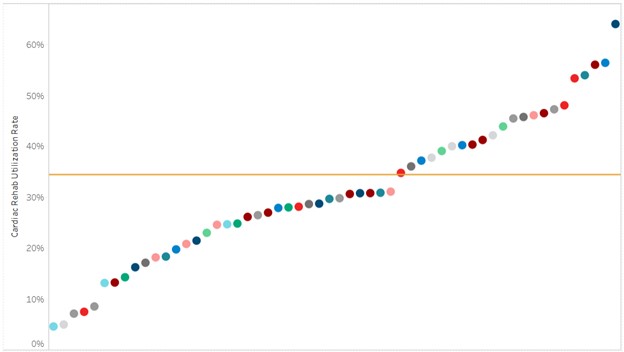
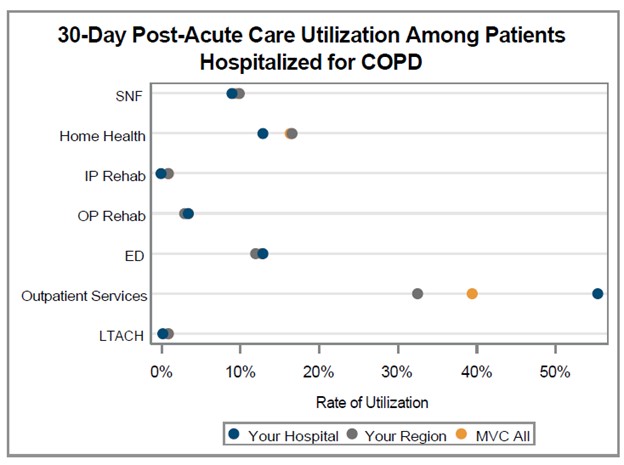
Beyond offering insights into payments by payer and post-acute care categories, this figure can offer additional insights and context compared to the report figure that follows it for post-acute care utilization rates (see Figure 2). The two figures together serve to provide a clearer understanding of the relationship between rates of utilization and percent of episode spending for each post-acute care category, illustrating whether spending aligns with utilization frequency. The post-acute care categories for both figures includes home health care, skilled nursing facility (SNF) care, inpatient rehab, outpatient rehab, emergency department care, long-term acute care hospitals (LTACH) and outpatient services.
Figure 2.
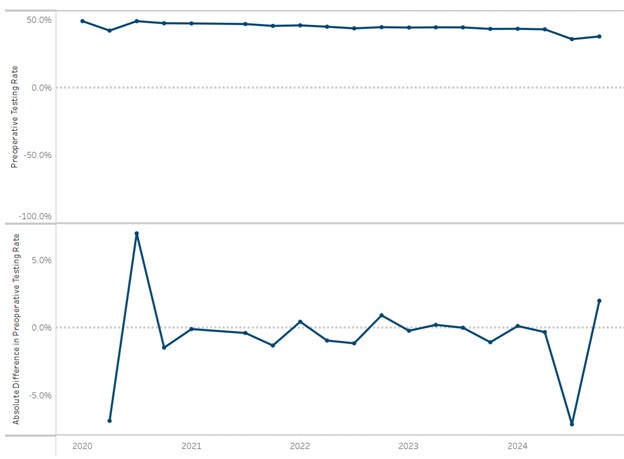
The remaining figures focus largely on ED utilization and readmissions, with some service line pages including figures for common reasons for readmission. Readmissions were generally observed to be highest across the collaborative at about 20% for patients hospitalized for CHF, followed by patients hospitalized for sepsis or COPD. Readmission rates were lowest across the collaborative at about 6% among patients who underwent a PCI procedure. There is also a visible decrease over time in 30-day readmission rates across the collaborative for all eight common conditions (see Figures 3 and 4); however, it is important to note that the 2024 Q3-Q4 data point does not include Medicare FFS patients, which is likely impacting the rate for that time interval.
Figure 3: 30-Day Readmission Rate Among Patients Hospitalized for Atrial Fibrillation, COPD, Colectomy, and CHF*
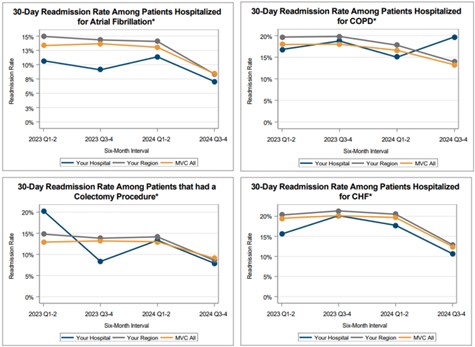
Figure 4: 30-Day Readmission Rate Among Patients Hospitalized for CABG, PCI, Pneumonia, and Sepsis*

*Data points are only shown for six-month intervals with 11 or more episodes. Data from 2024 Q3-Q4 excludes Medicare episodes.
MVC is dedicated to regularly updating its commons conditions report, aiming to equip collaborative partners with insightful data that can drive and reinforce meaningful advancements in healthcare quality. We hope these reports prove beneficial and welcome MVC members to contact MVC with any questions or analytic requests.