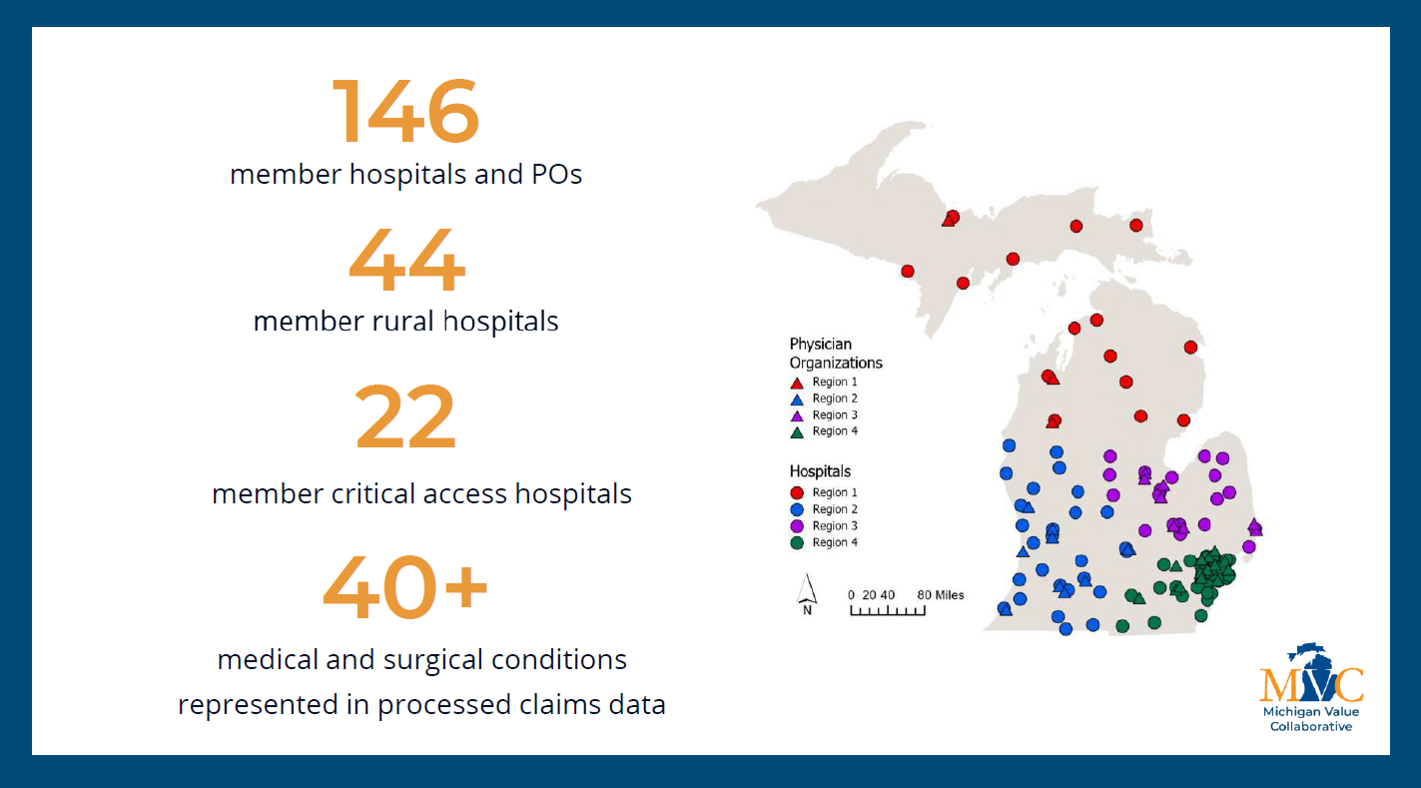
On August 21, 2025, MVC Coordinating Center hosted a virtual networking event providing members from rural, critical access, and acute care hospitals with an opportunity to make professional connections and discuss strategies for leveraging claims data. Twenty-three MVC members from twenty different hospitals and eight health systems participated in the ninety-minute event.
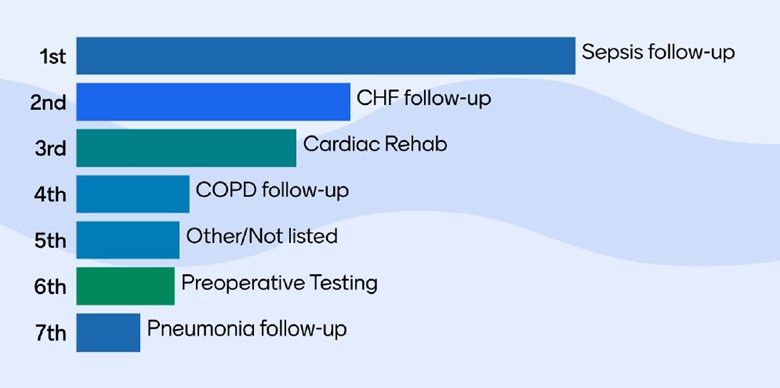
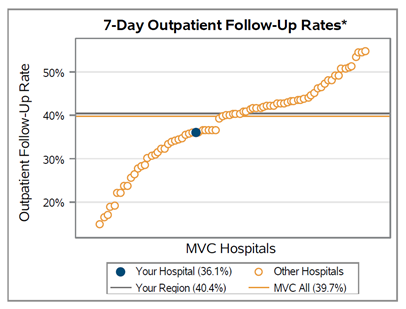
The event began with an ice breaker activity and a brief interactive quiz reviewing the number of and CMS requirements for rural and critical access hospitals (CAHs). This portion of the event concluded with a survey of MVC value metrics most relevant to quality improvement (QI) at rural and CAHs revealing most sites are focused on sepsis follow-up (Figure 1).
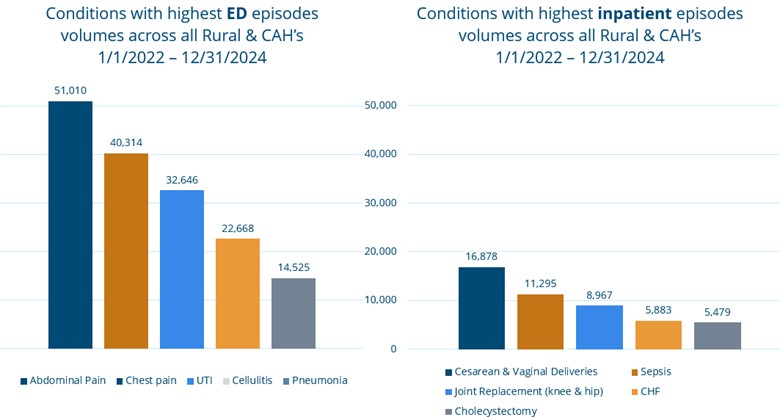
The networking event continued with a presentation by MVC’s Engagement Manager Jessica Souva, MSN, RN, C-ONQS highlighting MVC’s history with critical access and rural hospitals and the addition of ED-based episodes. Starting in 2016, CAHs began joining MVC membership and today twenty-four different CAH sites are active MVC members.
Souva emphasized the need to better serve this group by understanding their unique challenges. She then shared unblinded data on hospital-level index emergency department (ED) visits with behavioral health ICD-10 code rates for 30-day ED-based episodes from January 1, 2021 to November 30, 2024. Prior to sharing the data, members were asked where they thought their hospital’s rate would fall compared to the MVC All average, most felt their rates would be higher than the average. After sharing the data, most members found their rates to be lower than expected.
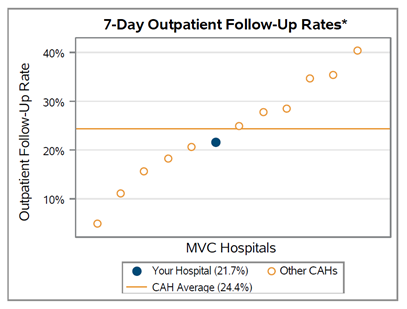
Aggregate data for conditions with the highest ED episode and inpatient episode volumes across all rural and CAHs from January 1, 2022 to December 31, 2024 were also shared (Figure 2). Souva encouraged members to discuss opportunities for benchmarking and custom analytics during the breakout session with this data in mind.
Figure 2. Conditions with the highest ED and inpatient episode volumes
The breakout discussions were structured to engage attendees in conversations about the challenges and strategies to address leveraging claims data for rural and CAHs. After breaking into two smaller groups, attendees were provided with three primary discussion prompts to reflect upon:
- Data Possibilities: What data sources and metrics are frequently utilized to determine outcomes and impact of process improvements in the inpatient or ED setting?
MVC members reported that various internal data platforms and benchmarking tools such as Vizient, Premiere, and Q-Centrix are used by critical access and rural health sites. They also noted frequently using metrics provided by various collaborative quality initiatives (CQIs) (e.g., HMS, MEDIC, etc.) and Medicare Beneficiary Quality Improvement Project (MBQIP) Core Measure sets to evaluate process improvements. When asked how MVC can optimize benchmarking for rural and CAHs, attendees explored options for comparing data with similar-sized sites and increased alignment between CQI pay-for-performance (P4P) metrics.
- Data Sharing: Which stakeholders are commonly engaged in determining strategies and indicators of successful QI initiative implementation?
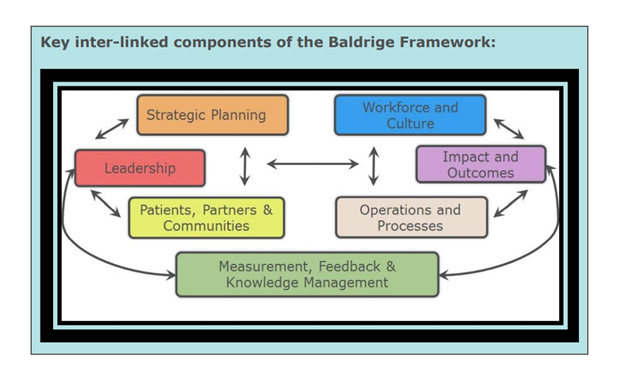
The discussions in both breakout rooms highlighted the importance of involving clinical leads, physician champions, and quality improvement oversight boards for the success of QIs. One hospital noted that they additionally include an executive sponsor for each QI which they find helps to drive QI forward. Others noted a shift in culture towards encouraging ownership of QI implementation to front line staff. They noted that with adjustments to quality departments’ scope and capacity, quality leadership can focus more on the “why” versus the “how” of QI.
- Conditions & Follow-Up Care: Are there specific conditions currently focused on reducing ED return visits and/or inpatient readmissions?
Key conditions of focus identified by MVC members include readmissions, chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), pneumonia, sepsis and diabetes. When asked if the data shared today inspired interest in new conditions or processes to investigate in the future, members noted interest in continuing to explore the utilization of behavioral health in ED-based episodes.
Feedback from members on MVC’s August Virtual Networking Event included:
- “I enjoyed participating and sharing during this event.”
- “This was very helpful. I would love more meetings like this specific to critical access hospitals and small rural hospitals.”
- “These networking events are always great and provide great insight into what is happening across the state. It allows us to share ideas but there is also a validation component that we are all experiencing a lot of the same challenges and barriers.”
- “This was a great networking event. As a member of an organization going through multiple ‘changes’, it was awesome to see how larger acute or rural hospitals tend to their QI projects.”
- “There was a lot of great dialogs about changing culture and how we approach quality improvement.”
MVC looks forward to hosting additional networking events in the future to increase collaboration and connection with MVC’s members. The next networking opportunity will be an in-person networking dinner on October 9, 2025, the evening before MVC’s Fall Collaborative-Wide meeting. If you are interested in attending, please register for this event here. Please note that space is limited.