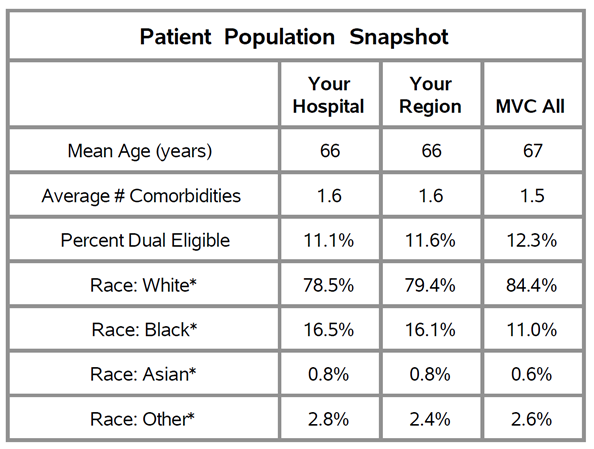
This year, the Michigan Value Collaborative (MVC) completed all scoring and evaluation for Program Year 2023 of the MVC Component of the Blue Cross Blue Shield of Michigan (BCBSM) Pay-for-Performance (P4P) Program. This concluded a two-year program cycle encompassing the program methodologies and conditions utilized in PYs 2022 and 2023. MVC is excited to share its member evaluation document for these two program years, which highlights hospital performance on average 30-day risk-adjusted, price-standardized total episode payments for the included conditions across both program years.
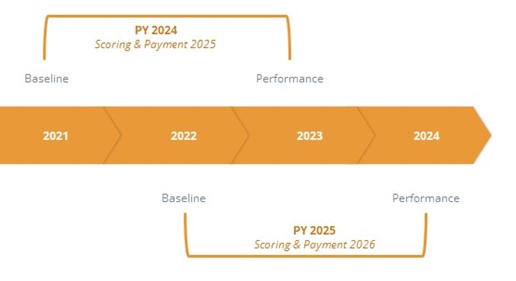
The PY 2022-2023 program cycle utilized episode claims from 2019 through 2022. PY 2022 scoring compared performance year data from 2021 against baseline year data from 2019. PY 2023 scoring compared performance year data from 2022 against baseline year data from 2020.
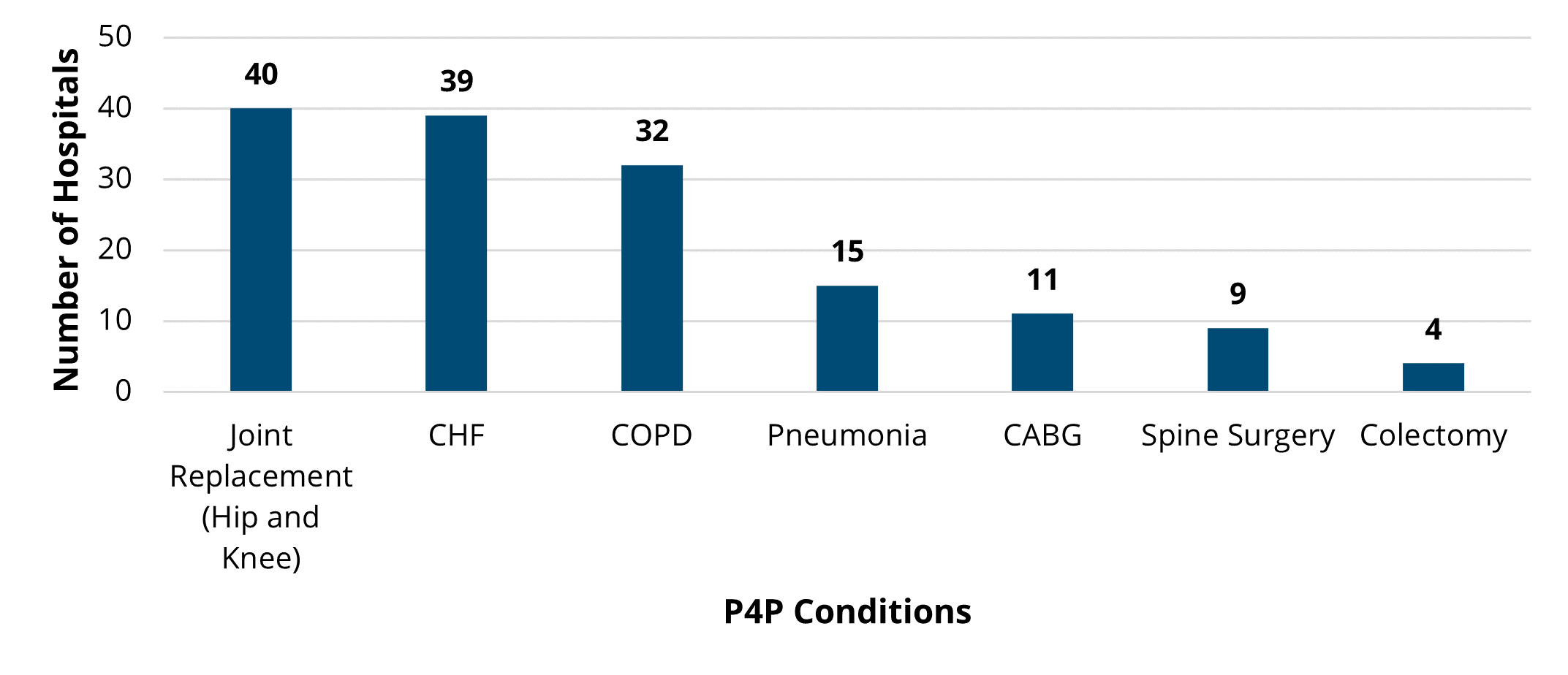
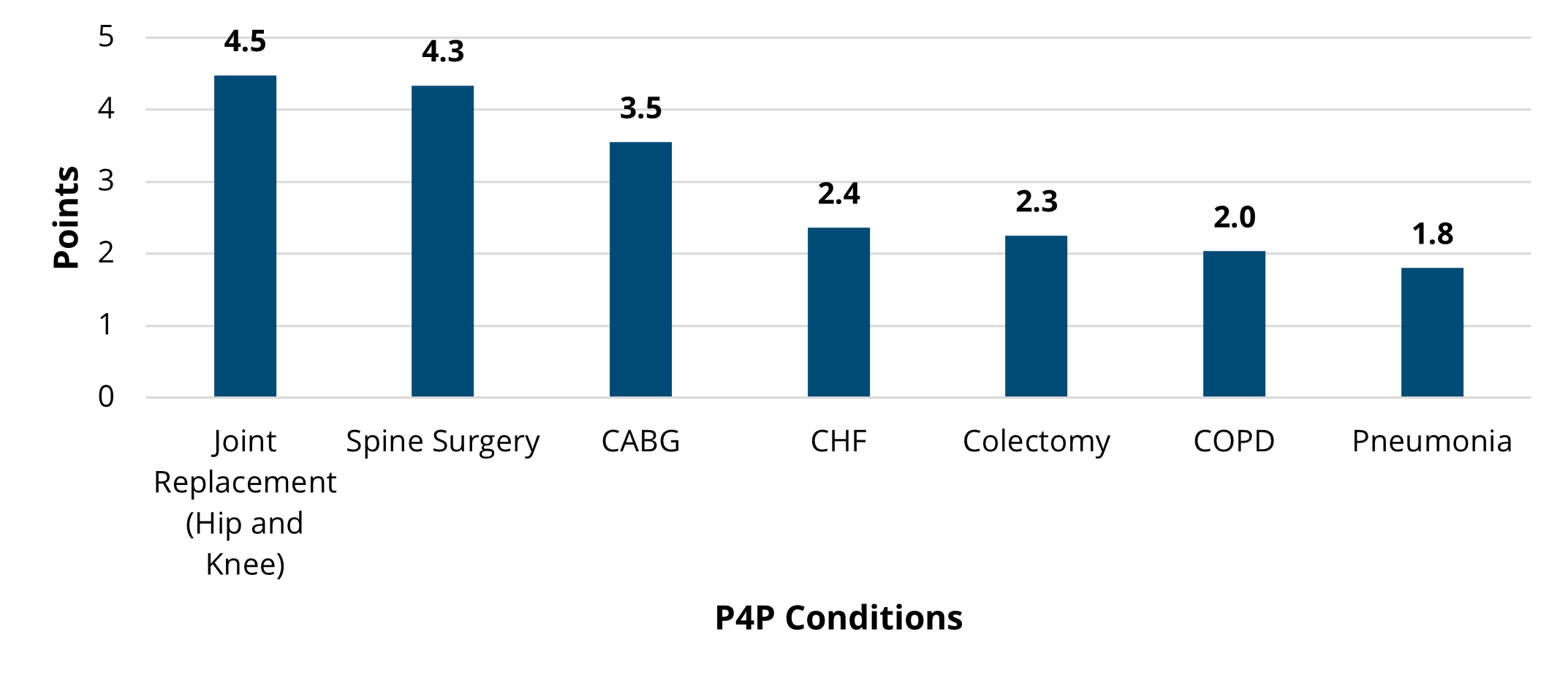
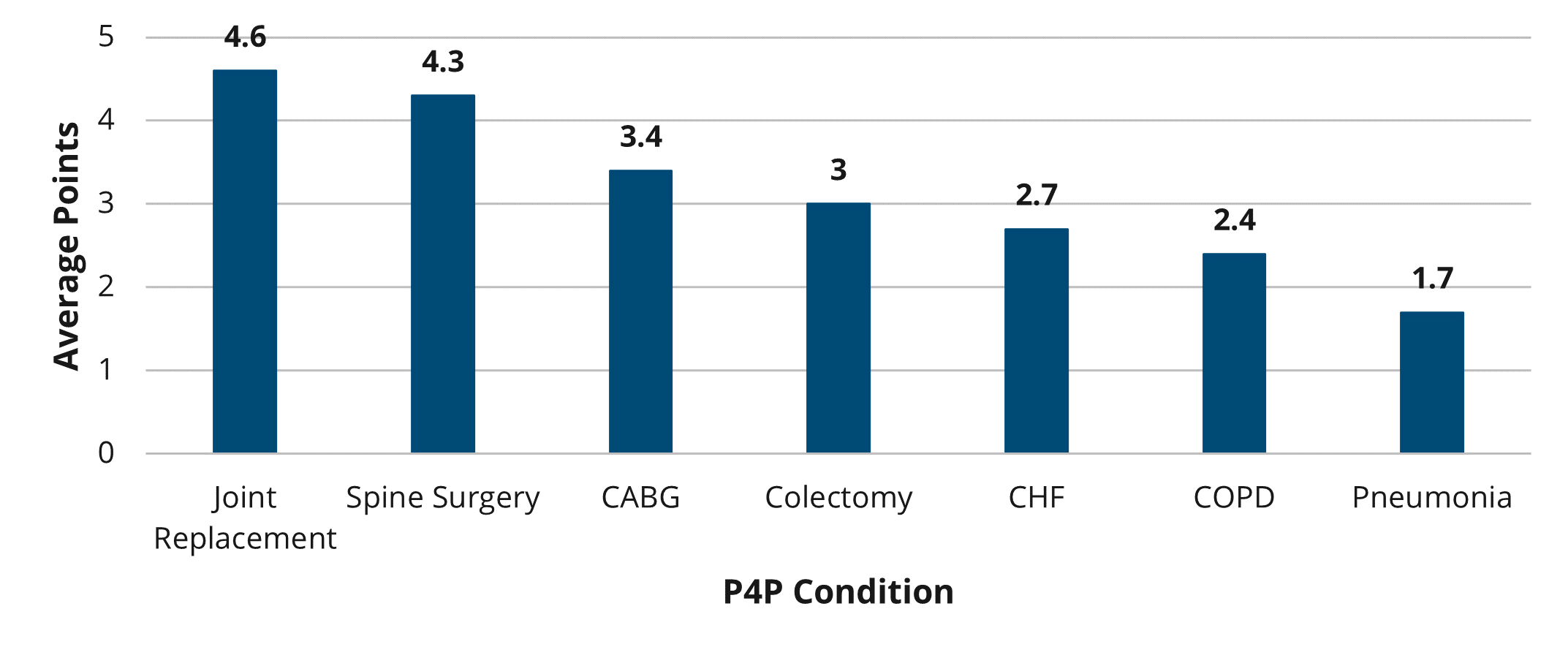
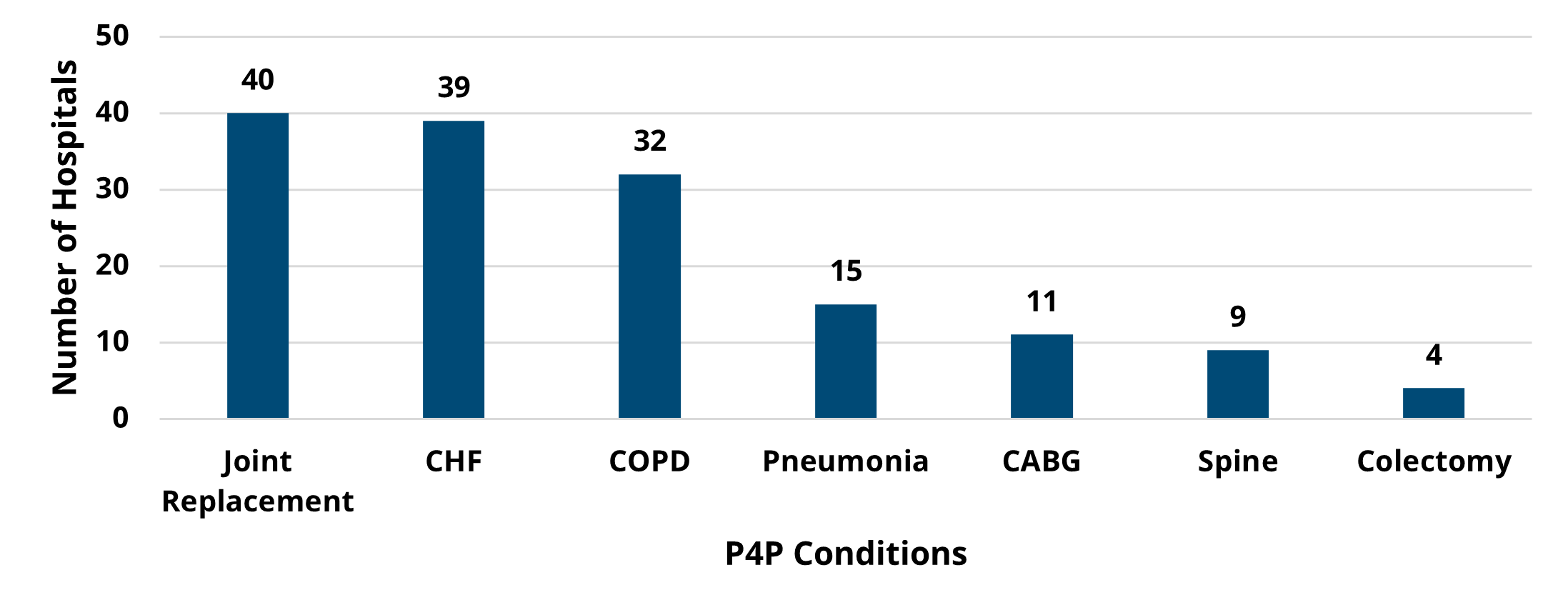
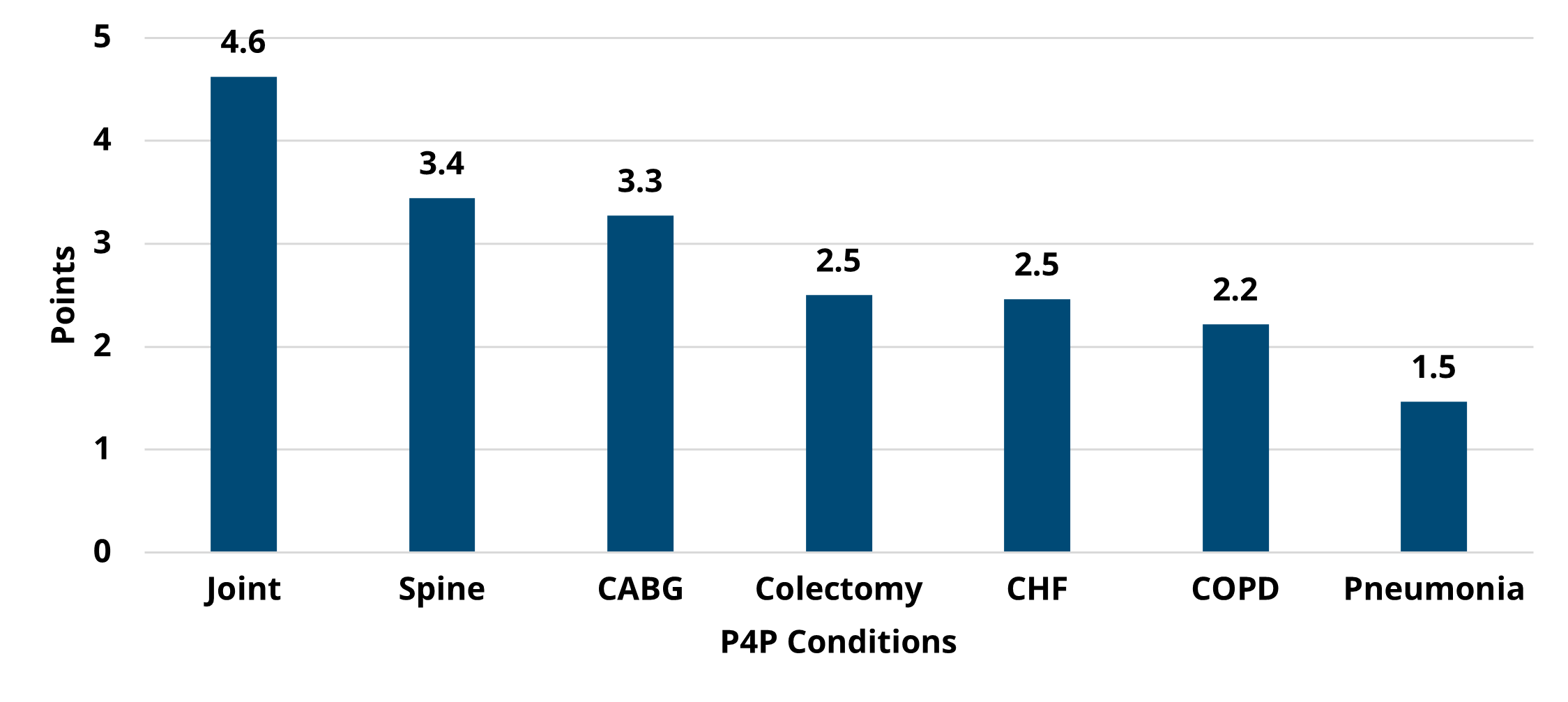
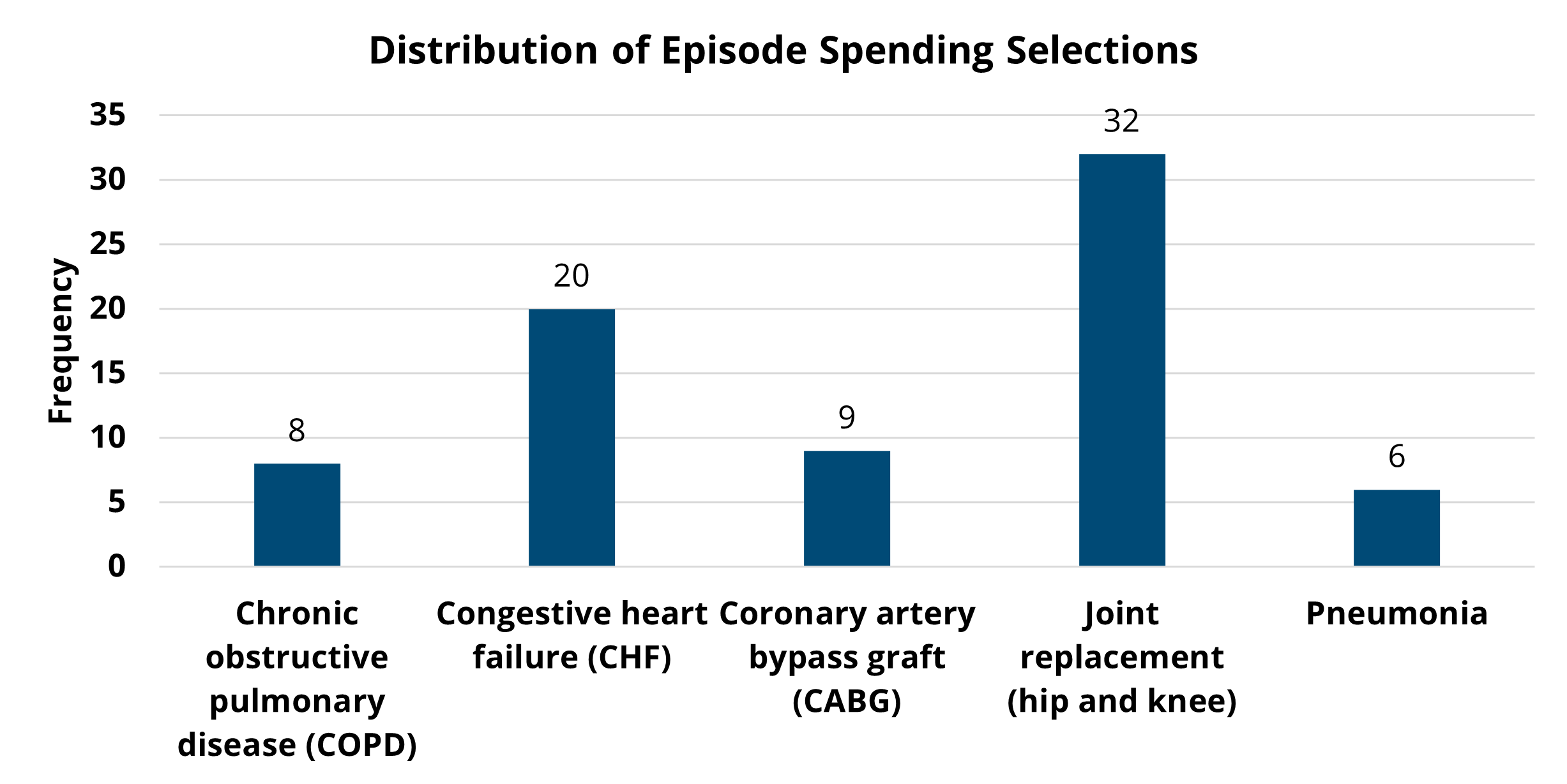
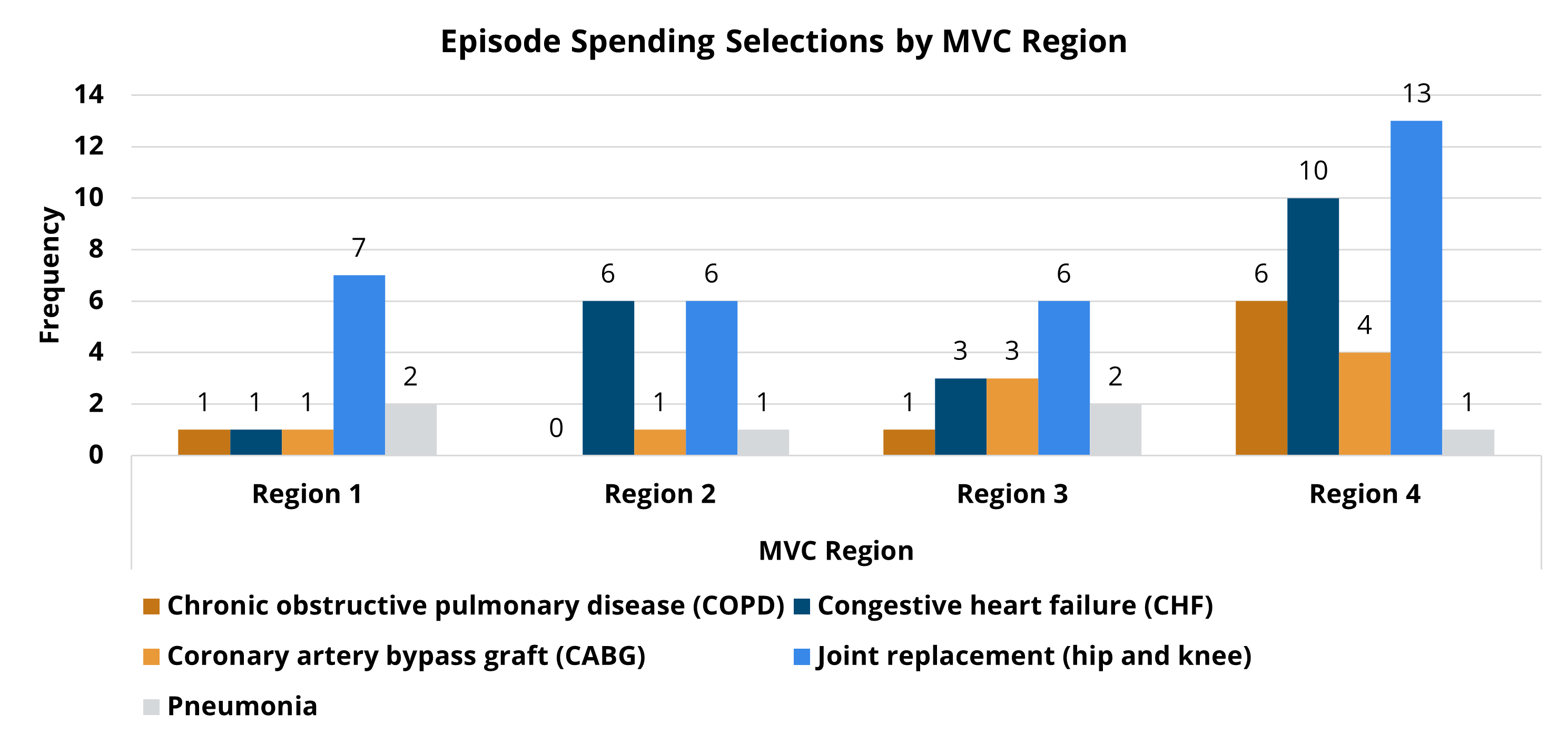
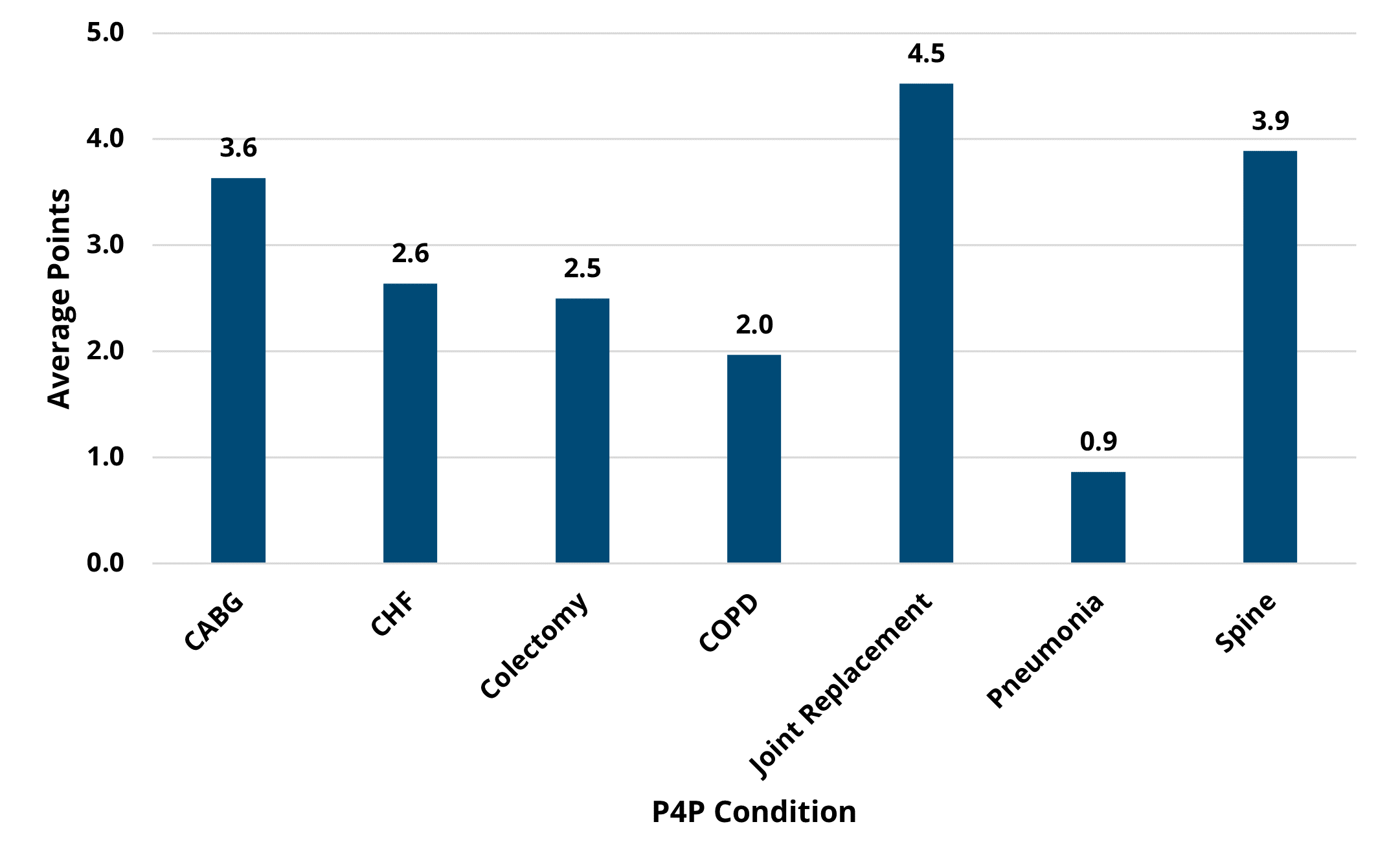
Hospitals chose two conditions from seven available options for the PY 2022-2023 program cycle, including chronic obstructive pulmonary disease (COPD), coronary artery bypass graft (CABG), congestive heart failure (CHF), colectomy (non-cancer), joint replacement (hip and knee), spine surgery, and pneumonia. Among these seven P4P conditions, joint replacement was the most selected condition (40), and colectomy was selected the least (4). Trends in average price-standardized episode payments showed a consistent decrease over the years for CABG and joint replacement, and a recent downward trend for pneumonia, spine, and colectomy payments as seen in Figure 1. MVC observed relatively consistent average payments over time for CHF and COPD episodes during PY 2022-2023.
The most striking observation in PYs 2022 and 2023 is the increasing shift to the outpatient setting for both spine and joint replacement surgeries. For joint replacement surgeries, 23.2% of episodes took place outpatient in 2019, 49.4% were outpatient in 2020, 71.6% were outpatient in 2021, and 85.4% were outpatient in 2022. Similar shifts were observed for spine surgeries during the PY 2022-2023 cycle, with the percent of outpatient spine surgery procedures increasing from 30.4% in 2019 to 51.4% in 2022 as seen in Figure 2.
This shift in outpatient utilization also impacted the decrease in average total episode payments since the associated costs for outpatient surgeries were significantly lower than inpatient surgeries. The decrease in total episode payments for spine and joint replacement surgeries was largely reflected in the index payments for PYs 2022 and 2023 respectively (Figures 3 and 4).
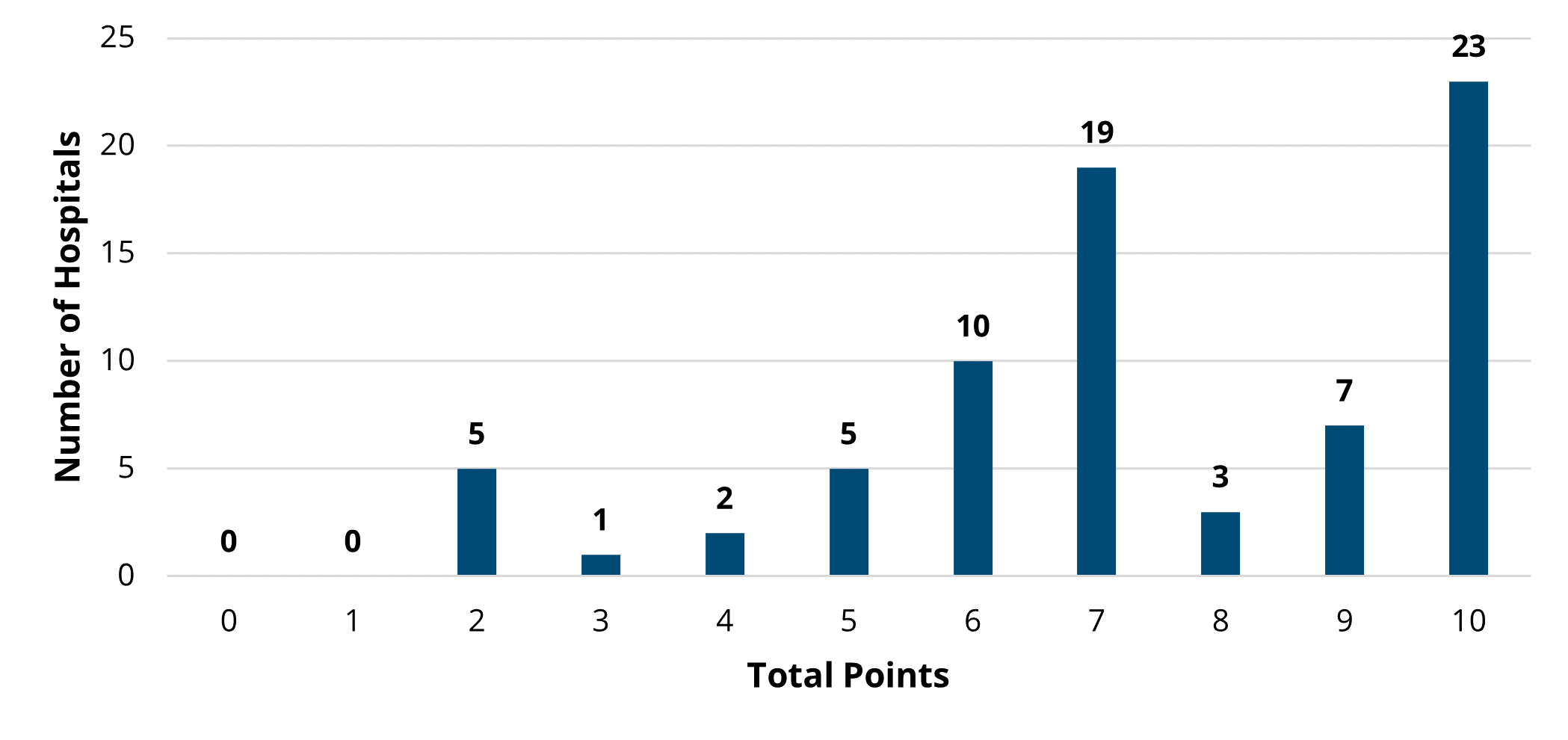
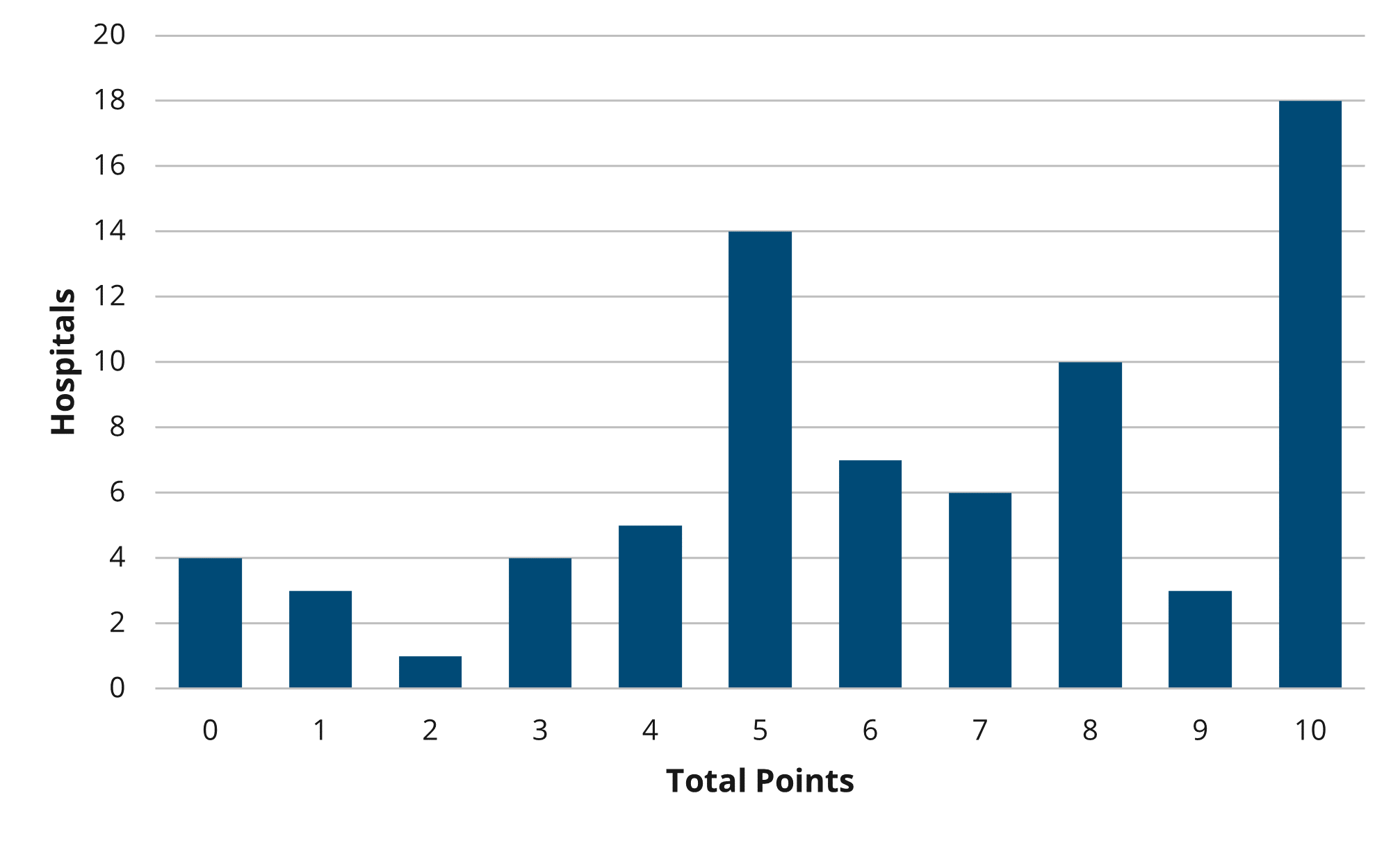
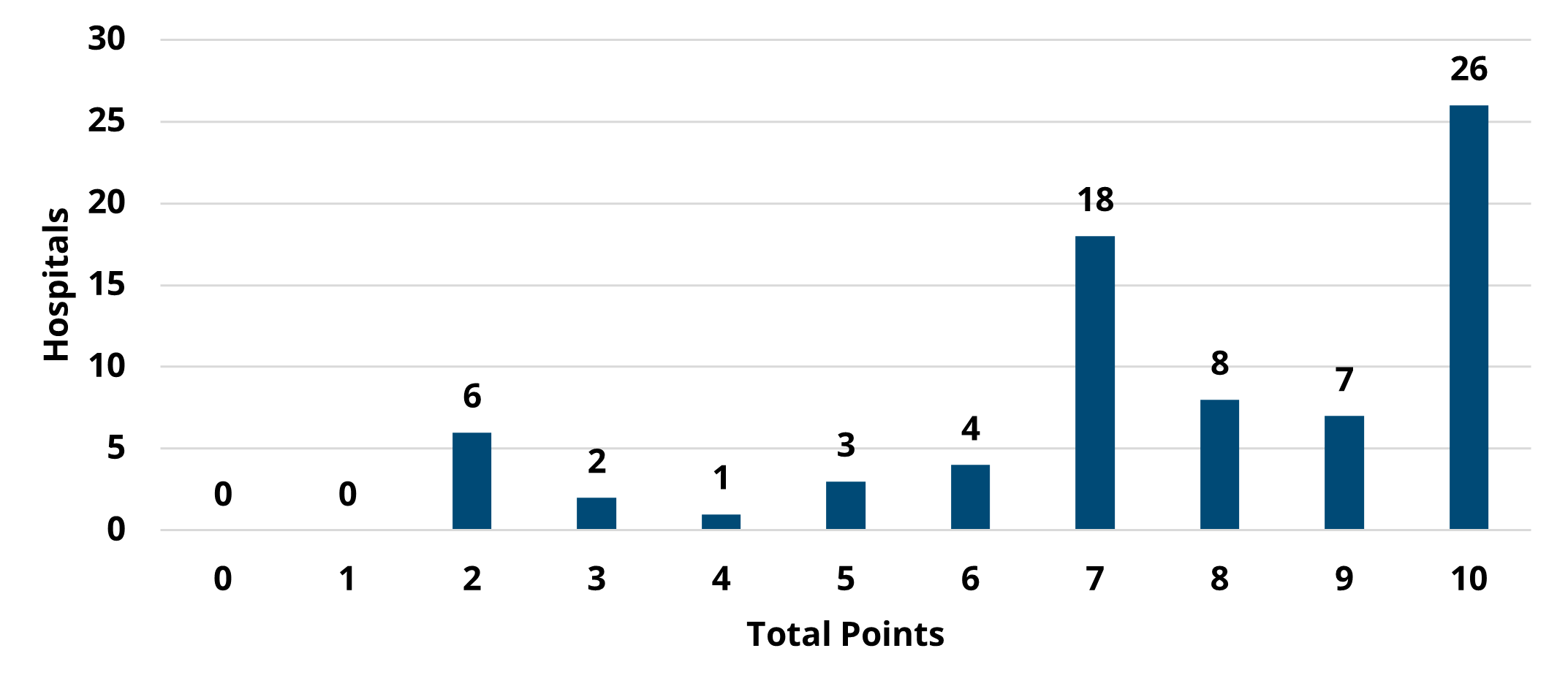
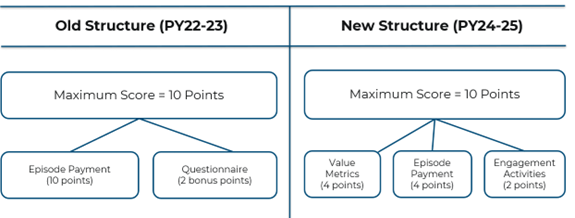
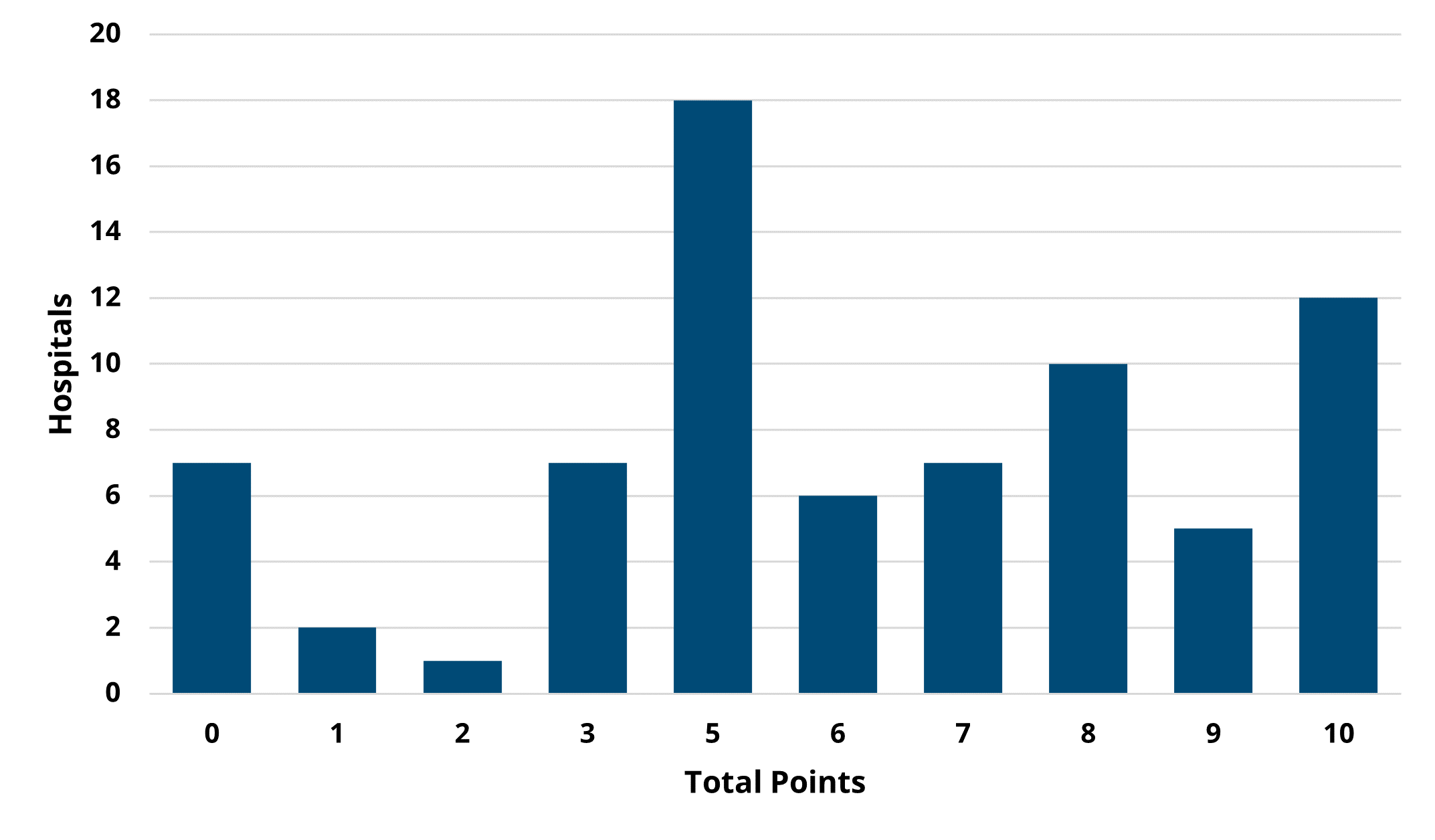
Overall, there was not much change between PY 2022 and PY 2023 in the overall points earned and average points based on hospital characteristics, though the scores on average were slightly higher in PY 2022 (Figures 5 and 6). For detailed, condition-specific analyses on scoring, please refer to the full member evaluation document.
If you have any questions regarding the MVC Component of the BCBSM P4P Program, please reference the P4P Technical Document for Program Years 2022 and 2023 and the MVC P4P FAQ PY 2022-2023. If you would like to set up a meeting to review your hospital’s performance, please contact the Coordinating Center at Michigan-Value-Collaborative@med.umich.edu.