Mental illness and related conditions such as depression are increasingly prevalent and costly. More than 50% of patients will be diagnosed with mental illness or disorder at some point in their lifetime, according to a World Health Organization research survey, and one in four adolescents will experience depression by the age of 18, contributing to an estimated $406 billion in medical treatment costs in a single year in the U.S. To bring attention and awareness to this issue, the month of May is celebrated nationally as Mental Health Awareness Month. It represents an important opportunity for healthcare providers and hospitals to evaluate the ways in which they currently support patients experiencing mental health/substance use disorder (MH/SUD) conditions.
To help facilitate this conversation, the Michigan Value Collaborative hosted a workgroup yesterday focused on increasing access to high-quality mental health for patients and increasing support for providers. MVC’s guest speakers hail from the Michigan Collaborative Care Implementation Support Team (MCCIST), including Gregory Dalack, MD, MCCIST Co-Lead and Daniel E. Offutt III Professor and Chair of the Michigan Medicine Department of Psychiatry, and Karla Metzger, LMSW, MCCIST Program Manager.
The presenters highlighted the psychiatric Collaborative Care Model (CoCM), an evidence-based integrated behavioral health model that is primary care based and highly cost-effective. Research evidence suggests that up to $6 are saved in long-term healthcare costs for every dollar spent on collaborative care. The presentation included research evidence of the benefits of CoCM, an introduction to its components, tips for implementation and common challenges, and several success stories from both patients and providers.
The Collaborative Care Model
Those unable to attend Thursday's MVC workgroup can access the full recording on MVC’s YouTube channel. Additionally, the American Psychiatric Association (APA) and Academy of Psychosomatic Medicine (APM) jointly developed a report on the CoCM that reviews current evidence, essential elements of implementation, and recommendations for better meeting the health needs of people with mental health conditions, which is available here.
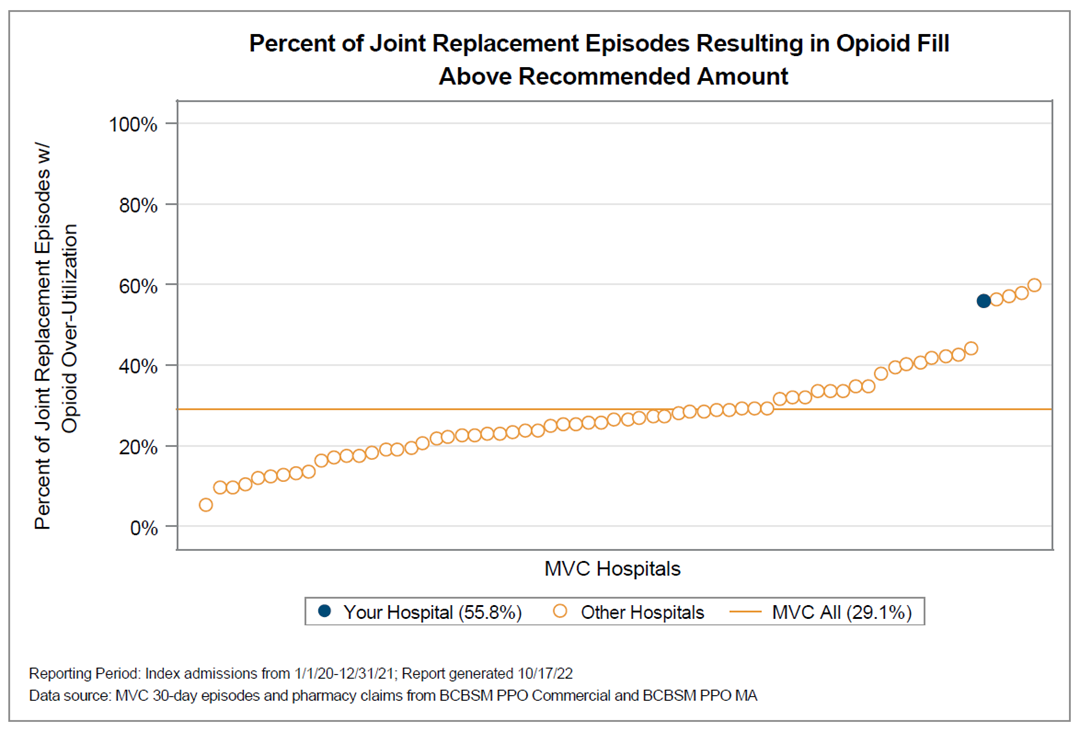
The American Hospital Association has also compiled a variety of resources on its Mental Health Awareness Month webpage related to mental health information, suicide prevention, opioid stewardship, downloadable posters to help employees adopt respectful language, case studies, and other tools and resources.
For those working in the behavioral and mental health space, there is also a recently formed Collaborative Quality Initiative (CQI) focused on mental health. Established in 2022, the Michigan Mental Innovation Network and Clinical Design (MI Mind) CQI is a statewide partnership with providers and provider organizations that works to prevent suicide and improve outcomes by reducing suicide attempts and deaths. MI Mind offers access to and engagement in evidence-based services for providers with a focus on suicide prevention, with plans to expand into other behavioral health domains, such as depression, anxiety, and substance use disorders. For a closer look at MI Mind, read MVC’s blog about their formation and check out the MI Mind website.