Healthcare Leaders Issue Support for Climate Change Mitigation
The past year forced healthcare to grapple with never-before-seen challenges. In response, facilities and clinicians found ways to think creatively, adapt, and find common ground with peers to best steward the health and safety of our communities. But the pandemic isn’t the only challenge requiring that kind of response. The healthcare industry is placing greater emphasis than ever before on the issue of climate change amidst the news and commitments coming out of the 2021 United Nations Climate Change Conference, also known as COP26.
The greater emphasis following this year’s conference is perhaps related to an increased overall focus on direct impacts to public health as well as the looming presence of a global pandemic that nearly all countries have struggled to manage. Countries like Britain are looking to reduce emissions by piloting a first-of-its-kind zero-emissions ambulance, citing that air pollution contributes to one out of every 20 deaths in the United Kingdom. The new vehicle was parked and promoted at the events in Glasgow. It is also notable that the healthcare industry has been increasingly concerned with variability in health outcomes due to social determinants of health; the impacts to human health by climate change and environmental pollution are also felt disproportionately by vulnerable communities.
The COP26 commitments included one from the U.S. Biden Administration to halve the United States’ greenhouse gas emissions by 2030. According to Health Care Without Harm (HCWH), an international nongovernmental organization concerned with mitigating healthcare’s impact on environmental health, “the U.S. health sector is responsible for 8.5% of U.S. greenhouse gas emissions and 27% of the global health care emissions… Addressing the climate crisis as a core driver of disease must be central to the health sectors’ mission today and in the future. As a fundamental sector in our society, and the only sector with healing as its mission, it makes sense for health care to lead the way to kick our addiction to fossil fuels, improve public health, and save billions of dollars in health costs in the process.”
They posited that healthcare has a unique relationship with climate change because of healthcare's role in bearing the financial costs and human health burden (see Figure 1 from the Centers for Disease Control and Prevention) from “increased disease spread and more frequent extreme weather events.”
This belief is shared by at least 45 million healthcare workers (which represents 75% of the health professionals in the world) associated with letters urging immediate action on climate change. There are already leaders in these efforts throughout the U.S. The Healthcare Climate Council created a playbook (see Figure 2) for operationalizing climate solutions in areas such as energy, food, leadership, operating rooms, purchasing, infrastructure, transportation, and waste.
The playbook contains success stories of facilities that have made meaningful changes, such as one about the Cleveland Clinic saving more than $4 million in 2019 by reducing air changes per hour during non-surgical periods as part of their Operating Room Setback Plan. They save 25 million kWh/year in energy use and $2.5 million annually. Similarly, Ascension deployed a data dashboard to report facility operations (energy, water, temperature, humidity, and air changes) on a real-time basis, and they implemented a pulse oximeter collection project that resulted in 664,000 medical devices collected and 66.4 tons of landfill waste avoided. They reported that this effort required collaboration between green teams, the purchasing department, environmental services, clinicians, facility managers, and the medical device reprocessing vendor.
Quality improvement efforts in healthcare have always been multifaceted, seeking to systematically reduce variation and improve outcomes by standardizing processes and structures. Quality professionals look at technology, personnel, culture, physical capital, leadership, training, operations, and procedures, among other areas. This means that healthcare’s quality improvement teams are uniquely positioned to support their leadership in identifying and implementing climate solutions. These changes that help mitigate climate impacts also often lead to more efficient, sustainable care delivery.
There are a number of professional organizations ready to assist and offer guidelines for practice improvement, including Health Care Without Harm, its sister organization Practice Greenhealth, the Alliance of Nurses for Healthy Environments, the American Society of Anesthesiologists, the Association of American PeriOperative Registered Nurses, and the American Academy of Family Physicians, among others.
Much like with the COVID-19 pandemic, the actions and decisions of one facility, community, or country ultimately have an impact on everyone else, which means a culture of collaboration is a prerequisite for the successful integration of climate change mitigation in healthcare. If your hospital or physician organization has achieved value or outcome improvements that relate to environmental health or sustainability, the MVC Coordinating Center can help share your story. Please contact the MVC team at michiganvaluecollaborative@gmail.com.
Staffing Shortage Challenges Hospitals Across Michigan
The past 18 months of the pandemic forced healthcare to be creative and responsive to the needs of the moment, and in that time the MVC Coordinating Center heard from members about how they are working to maintain a high quality of care. The challenges and pivots shared by members vary significantly because facilities were impacted at different points in time and with varying levels of severity. However, one challenge echoes loudly and consistently for hospitals big, small, urban, or rural: the staffing shortage. This problem isn’t specific to Michigan. Across the United States, hospitals don’t have enough staff to keep up with their normal standards of care, with many having to turn away patients and ration care.
Health professionals are the lifeblood of healthcare delivery, so attaining or maintaining a high quality of care is only achievable with appropriate staffing levels. The Institute of Medicine framework defines quality care with six aims: that it be safe, effective, patient-centered, timely, efficient, and equitable. Some of those aims have been directly exacerbated by the pandemic—such as health equity or safety—while many have been at least indirectly impeded by the strains on frontline workers.
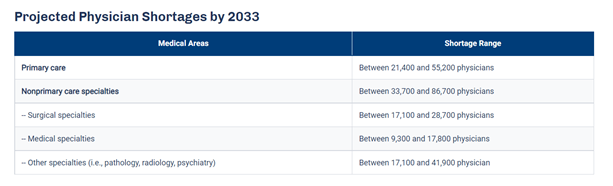
An article published by the Detroit Free Press this month titled, “Michigan hospital staffing shortage nears crisis point as COVID-19 patients rise,” paints the current situation as dire. The article quotes Brian Peters, the CEO of the Michigan Health & Hospital Association, as saying, “I have never heard a consistent theme from across our entire membership like I have on this staffing issue." He adds that the shortage affects multiple sectors of the workforce, such as nurses, physicians, housekeeping, technicians, and food service personnel. These new staffing issues occur within an industry that was already concerned about an expected shortage of primary care physicians (PCPs). The Association of American Medical Colleges (AAMC) published data that predicts an estimated shortage of between 21,400 and 55,200 PCPs by 2033 (see Figure 1), in part due to a population that continues to grow and age.
Figure 1.
Some hospitals suggest burnout as the main culprit for the current staffing shortages. A literature review on the effect of burnout on quality of care defines burnout as a state of fatigue and frustration manifested as physical and emotional exhaustion characterized by dissatisfaction and stress, with symptoms such as, “physical fatigue, cognitive weariness, and emotional exhaustion.” Anyone in that condition cannot perform at their best. So as quality teams try to find treatment efficiencies for conditions such as chronic obstructive pulmonary disease (COPD) or congestive heart failure (CHF), the elephant in the room is that they may not be able to provide treatment if nurses, technicians, and physicians aren’t adequately staffed.
The industry is expecting the shortages to increase slightly in the coming weeks as vaccination mandate deadlines approach. Currently, those health systems requiring COVID-19 vaccination include Henry Ford, Michigan Medicine, Beaumont Health, Trinity Health, Spectrum Health, OSF HealthCare, Ascension Health, and Bronson Healthcare, along with Veterans Health Administration facilities.
A variety of strategies are being proposed to lessen the burden felt by the shortage. Since it takes time to recruit new people into medical fields, these approaches generally fall into one of two categories: 1) retain current staff, and 2) deploy current staff as efficiently as possible.
The approaches that hospitals have mentioned for retaining staff are short-term in nature, ranging from approval of overtime and bonuses to instituting new staff well-being programs and sharing mental health resources. Efficient staffing is a more complex approach, but long-term with the potential to reduce the expected burden from future PCP shortages. The Harvard Business Review published an article that outlines strategies for efficient staffing in response to the PCP shortage, which could be repurposed and applied to other healthcare workforces. Among their suggestions, they highlight Advisory Board research that proposes the threefold answer is, “better use of PCPs targeted at specific populations, greater use of non-physician labor where appropriate, and much broader deployment of technology to increase access to primary care.” These suggestions align with several other priorities often voiced to the MVC Coordinating Center by members, including equitable access to care, expanded telehealth offerings, and improved care coordination utilizing nurse practitioners and physician assistants.
The work ahead will be challenging, as it often is in healthcare. Hospitals will continue to shoulder a shared burden in the months ahead. MVC encourages all members and partners to share resources that may help a peer institution improve the quality of care for Michigan residents. Please continue to bring these ideas to future workgroups and networking events, and contact the MVC Coordinating Center at michiganvaluecollaborative@gmail.com.
Growth On the Horizon for Robotic Process Automation in Healthcare
Hospital quality improvement teams have an increasingly difficult task ahead. Their efforts to improve quality of care across a wide range of medical services must be balanced with the need to expand their facility’s capacity, ensure proper handling of sensitive data, adhere to strict procedures, cut costs, and adapt to the limitations of a pandemic. This work poses challenges both organizational and operational. Even though patient care is the primary focus for hospital staff, they must maintain a constant stream of paperwork and other administrative tasks such as data entry, scheduling appointments, billing, and managing claims paperwork. Robotic process automation (RPA) presents an opportunity to decrease these administrative costs and streamline some operations.
RPA is defined as software that can automate repeatable, rule-based processes. RPA interacts with the assigned applications in the same way that a human does, logging into a given system and following a defined set of keystrokes and rules. It is not the same as artificial intelligence (AI)—there is no decision-making capacity. RPA can only offload manual, high-volume computer processes. The primary benefit of RPA, therefore, is its ability to free up time for humans to complete more complex tasks, such as interfacing with patients or interpreting data.
RPA is a burgeoning field recommended by consulting groups such as Deloitte, McKinsey, and Bain & Company. Although RPA hasn’t had sufficient time to make its way into academic literature, it is spreading quickly in all types of industries. For example, according to Deloitte’s Global RPA Survey, more than half of their 400 respondents from multiple industries were already pursuing automation with as many as 72% looking to add RPA in the next two years.
“RPA exceeds adopters’ expectations not only when it comes to the rapid rate of ROI increase, but also when it comes to facilitating compliance (92%), improved quality and accuracy (90%), or improved productivity (86%),” the report read. The report also suggests that the benefits of utilizing RPA may include cost reductions, boosts to productivity, more stable workflows, and fewer human errors, among others (see Figure 1).
Source: Summit Healthcare
Healthcare as an industry has the potential to significantly benefit from offloading administrative tasks to bots. According to McKinsey, the healthcare sector has the potential to automate around 36% of tasks. They suggest that the greatest potential for healthcare payers is in areas such as claims processing, customer service, and billing activities (see Figure 2).
Hospitals and health systems have pursued RPA in these areas as well and found success. One example written about in Forbes recently described the efforts of Baylor Scott & White Health (BSWHealth), an academic medical system with 52 different hospitals and the largest not-for-profit provider in Texas. BSWHealth uses RPA to automate “claim statusing” in its insurance collections department. The bot helps to check the status of outstanding insurance claims that, previously, a human employee would have to do by logging into multiple payer websites or placing phone calls. The RPA bot uses screen-scraping technology that mimics keystrokes the employee would enter to obtain claim statuses from payers. As a result, an abundance of claims—those that are accepted and scheduled to be paid—never clutter the employee’s desk. Instead, the employee only sees those that are denied and require human attention, resulting in outstanding claims being addressed faster. BSWHealth is pursuing a variety of RPA projects like this one across all of its revenue cycle departments. They reduced their total FTEs by over 20% while simultaneously reducing payer denials by 20%.
Success stories like this one are particularly exciting for hospitals struggling to manage their case load amidst the pandemic. Daily operations and procedures have been severely impacted financially and operationally by coronavirus. A recent survey conducted by the World Health Organization identified that almost half of the countries surveyed (49%) reported strains on their ability to treat diabetes, with 42% reporting the same for cancer and 31% struggling to properly manage cardiovascular emergencies. As a result, companies are pursuing automation opportunities more than ever before (see Figure 3), with Bain & Company reporting as many as 81% of hospitals pursuing RPA initiatives.
Still, according to a 2019 white paper by The Economist, “extensive” use of automation is only used by half of healthcare organizations, and healthcare in general is among the most resistant to adopting it. Some healthcare organizations remain cautious for a variety of reasons, including concerns about initial investments, maintenance costs, and the possibility of failure. The same white paper also proposes that data privacy and security concerns might be a significant hinderance to RPA efforts, as well as a deficit in the skill sets needed to develop the bots.
Plus, any discussion of RPA sometimes begets fears about job replacement. In some scenarios, health systems have seen an overall decrease in FTEs after putting RPA initiatives in place. However, the overall goal is usually to reallocate effort toward more high-level, cognitive projects in a way that increases productivity without replacing people. If an administrative task requires no higher-level thinking, then giving it to an RPA bot will free up time for clinical staff to attend to patient care rather than paperwork. In fact, according to Harvard Business Review, most new adopters of RPA have promised their employees that it won’t result in layoffs.
Despite hesitations, health systems are likely to test out RPA projects in the coming years in response to the current state of affairs. Hospitals have been forced over the past year to find efficiencies where they can. RPA bots appear to have the potential for a variety of benefits, not the least of which is flexibility to redeploy personnel to areas in need of increased staffing. As RPA begins to make its way into the literature, it will be important to consider research findings about best practices going forward.
It will also be helpful going forward to share lessons learned with peer institutions. One of the goals of the MVC Coordinating Center is to support collaboration and idea sharing across its membership. If any member is implementing RPA projects and would be interested in sharing their experience with others, please contact the MVC Coordinating Center team at michiganvaluecollaborative@gmail.com.
Identifying and Solving Potentially Preventable Hospitalizations
As hospitals continue to work on reducing readmissions, another area of focus to reduce costs is through preventing potentially preventable hospitalizations, especially in chronic conditions. Potentially preventable hospitalizations, known as PPHs, are unplanned hospitalizations that have the potential to be avoided if timely and appropriate outpatient care had been received. However, in order to reduce these admissions, there has to be a means of identification. A number of methods have been reviewed to try and develop a way to identify those patients at risk of having a PPH.
In Australia, a Preventability Assessment Tool (PAT) was developed to attempt to identify patients at high risk of PPH The use of the tool compared to a similar assessment performed by an expert panel was assessed to learn if the tool identified appropriate patients. The findings were recently published in a journal article. The expert panel consisted of a hospital physician, a primary care physician (or general practitioner (GP)), and a community nurse with expertise in the chronic conditions. The publication identified that the carefully constructed and developed PAT, when compared to the assessment of the expert panel, did not effectively identify those at risk of a PPH.
Another method to potentially identify these types of admissions is a hospital outreach program, also implemented in Australia. In the program, the patient record is flagged for areas of concern such as general health, medication, and wellness. Red flags are specific to disease or symptoms that have the potential for hospitalization. Trained telehealth guides reach out on a frequent basis (greater than weekly), while patients and caregivers can call in to the program at any time. Analysis of the flags being triggered through these phone calls may alert personnel to a deterioration in patient health, concerns about medications or a lack of support, and allow for outpatient care to be provided in a timely manner to avoid a hospitalization.
A study within the United States compared deep learning against a logistical regression model to identify prediction models for preventable hospitalizations, emergency department visits, and costs in heart failure patients. The study found that deep learning approaches identified these preventable areas more accurately than the traditional methods, indicating that outcomes are contributed to by clinical, demographic, and socioeconomic factors. The study found the main predictors for preventable hospitalizations in heart failure patients were diuretic usage, orthopedic surgery, and age (see Figure 1).
Research suggests that although hospitals can work to identify who is at risk for a preventable hospitalization or preventable emergency department visit, a more preferable method of reducing these is improving not only quality of care but also access to care within the primary sector of the community. By reducing barriers to healthcare and improving local community services, population health outcomes can potentially be enhanced which, in turn, may lead to a reduction in potentially preventable hospitalizations.
The Michigan Value Collaborative is interested in hearing how your facility is working towards identifying potentially preventable hospitalizations and ED utilization. Please contact us at michiganvaluecollaboarative@gmail.com.
Supporting the Mental Health of Healthcare Workers During COVID-19
Over the last year, the way in which care is delivered has changed and in turn, healthcare workers are faced with potentially high levels of anxiety and depression. These front-line workers, already at risk for high-levels of stress and burnout, are now experiencing even higher levels of stress. Mental Health America recently shared an article that discussed a survey distributed to healthcare workers from June-September of 2020. This survey was designed to gain an understanding of the experiences of healthcare workers working during the COVID-19 pandemic and to create better resources moving forward.
Around 93% of the 1,119 healthcare workers surveyed reported feeling stress, with approximately 86% of respondents noting experience of anxiety. The majority of respondents (76%) were worried about exposing loved ones such as children, spouses or even an older family member. Additionally, emotional and physical exhaustion were common changes reported over the previous three months, with healthcare workers often faced with a lack of emotional support. Despite these results, over half of survey respondents felt they were receiving emotional support from their family and over a third felt supported by their work colleagues.
While emotional and physical exhaustion is taking its toll, anxiety and depression in healthcare workers has also been caused by the uncertainty of how the pandemic will play out. There is a lot of unpredictability regarding the virus as new strains occur, surges continue, and people hesitate or decline vaccination. To help support healthcare workers, the National Academies of Sciences, Engineering and Medicine are responding by putting together a coronavirus resources section that has resources to support healthcare workers. These resources include information and webinars geared towards clinician well-being such as “Supporting Clinician Well-being During COVID-19” and “Taking Action Against Clinician Burnout”.
The Michigan Value Collaborative is committed to supporting collaborative members during the COVID-19 pandemic, and we know hospitals and physician organizations are working diligently to help support their individual staff during this time. To share the ways you are supporting your healthcare workers at your organization, please email us at michiganvaluecollaborative@gmail.com.
Monitoring Chronic Disease Utilizing Social Media and Sensors
According to the Centers for Disease Control and Prevention, “treating individuals with chronic diseases accounts for 86% of health care costs.” While the number of those living with chronic conditions and the associated costs may be increasing, the Michigan Value Collaborative (MVC) is committed to providing you with current data around providing the right care, at the right time, at the right cost. Technological advances in healthcare are changing how and where chronic disease care is being delivered, how these patients interact with providers, and how organizations exchange information.
Both diabetes and abnormal blood pressure (BP) are extremely common in chronic disease patients and cause various complications, including an increased risk of cardiovascular events. When thinking about the way in which these chronic diseases should be managed moving forward after the COVID-19 pandemic, technological advances offer promising solutions. Most devices in the healthcare industry have been digitalized. This advancement allows for routine monitoring using various devices that some patients may already own, such as a smart phone or a smart watch. These devices contain sensors that can be used to obtain information that can then be transmitted straight into the electronic health record (EHR). Other devices that can be used to collect patient information include a glucometer sensor, pulse oximeters, temperature sensors, scales, and many more. However, this method is not without its limitations.
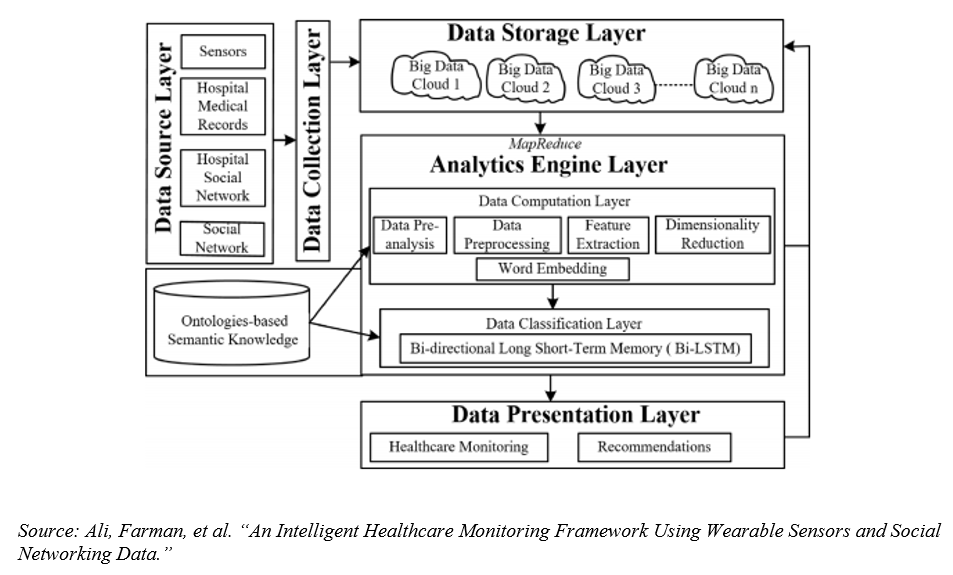
The amount of data that is generated from these devices is vast and not all systems are capable of storing and processing it efficiently for precise and real time monitoring. In order to negate this issue, a framework was recently published that can be seen in Figure 1 below. This framework utilizes the cloud environment along with a large analytics engine layer to help store and process the data. The recently published study identifies the importance of utilizing wearable sensors and social networking platforms in collecting patient data, but identifies the challenges that come with this such as issues with data storage and running correct analyses.
Chronic disease management patients may use social media platforms in order to seek support or learn new ways in which they may be able to reverse certain symptoms. Other ways in which monitoring is done through social networks include patient and provider conversations through application programming interfaces (APIs). Through these APIs, providers can pick up on tone or social connection status. Through this proposed framework of social media and sensor monitoring, providers can closely monitor chronic disease management patients.
MVC hosts chronic disease management workgroups where collaborative members discuss their current initiatives and connect on ways in which they can work together to better the health of Michigan. If you have any questions about upcoming chronic disease management workgroups, please feel free to contact the coordinating center at michiganvaluecollaborative@gmail.com
Long COVID-19, Just One Aftereffect of COVID-19
With continued COVID-19 surges occurring worldwide despite the availability of a number of variations of vaccines, some patients continue to experience what is now being dubbed as “Long COVID-19” or “Post COVID-19 Syndrome”. Symptoms that are commonly experienced include a persistent cough, dyspnea, chest and/or joint pain, neuralgia, and headaches. These symptoms can last up to 12 weeks and in some cases, even longer. The more people that develop long COVID-19, the greater the strain on the healthcare system and need for appropriate diagnosis and treatment options.
A recent paper by A.V. Raveendran from January 2021 proposed diagnostic criteria to help confirm a diagnosis of long COVID-19. Depending on clinical symptomology, duration criteria and the presence or absence of a positive swab or antibodies, a long COVID-19 diagnosis can be categorized as confirmed, probable, possible or doubtful. Having an appropriate diagnosis will allow the practitioner to prescribe the relevant treatment plan.
In the United Kingdom, where the number of people exhibiting long COVID-19 continues to increase, a guideline has been developed by the National Institute for Health and Care Excellence to provide recommendations to help identify, assess, and manage the effects. As more evidence is collected, the plan is to update the document on a continuous basis to maintain its validity. The guideline takes into consideration clinical symptomology, duration criteria, and the presence or absence of a positive SARS-Cov-2 test. It also provides guidelines for suggested referrals, and a plan of care with follow-up and monitoring.
While the guideline manual has many useful suggestions, there are a number of gaps where further detailed information will be needed. As new information is discovered, the goal is to include comprehensive reviews of symptomology, and pathology of the disease process and a better understanding of the variation in impact. Simultaneously, there needs to be an increase in rehabilitation and community resources to allow for individualized evidenced based care for those suffering from the debilitating effects of long COVID-19.
The Michigan Value Collaborative continues to assess data related to COVID-19 and will be sharing a dedicated COVID-19 push report with members in the coming months. If you would like access to the MVC registry, please request it here or via email michiganvaluecollaborative@gmail.com
Telehealth Use: Maintaining Access to Surgical Care During the COVID-19 Pandemic.
The COVID-19 pandemic created a unique situation which led to the high use of telehealth in caring for the medical patient population. However, it was unknown whether these same patterns would transfer to surgical care. The Michigan Value Collaborative (MVC) registry allows health systems to leverage administrative claims data from a variety of sources and better understand trends in telehealth use. Using MVC BCBSM data, the Telehealth Research Incubator at Michigan Medicine found in their study that telehealth was a viable way for patients to access surgical care.
Historically, surgery is the medical field least likely to use telehealth. However, with in-person care constraints resulting from the pandemic and updated policies making it feasible for telehealth visits to be eligible for reimbursement, a large uptake in telehealth among surgeons was witnessed.
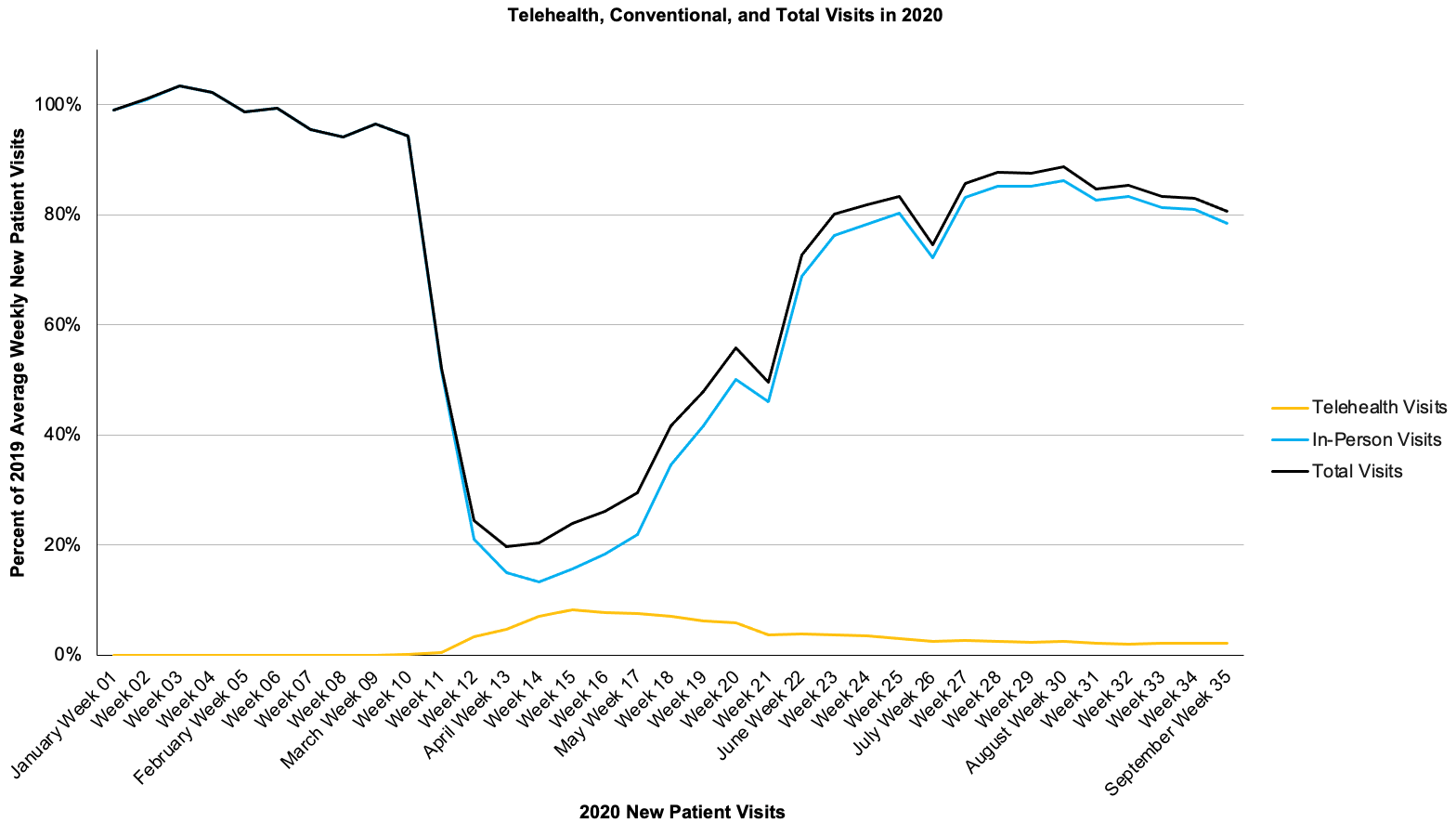
Approximately 60% of active surgeons used telehealth in some capacity during the pandemic. Specifically, our study examined telehealth use for new patient visits. We were curious if surgeons were able to use telehealth to evaluate new patients, and the results proved that this was a viable and beneficial option to provide care. Significantly, 27% of all active surgeons used telehealth for new patient visits.
As shown in Figure 1, at peak use, we found over a third of visits for new patients were performed using telehealth. This is in contrast to the fewer than 10 telehealth new patient visits in 2019.
Figure 1
In addition, the study indicated that telehealth was successfully used for many surgical visits across multiple different surgical specialties, with urology and neurosurgery being the highest utilizers. This is shown in Figure 2.
Figure 2
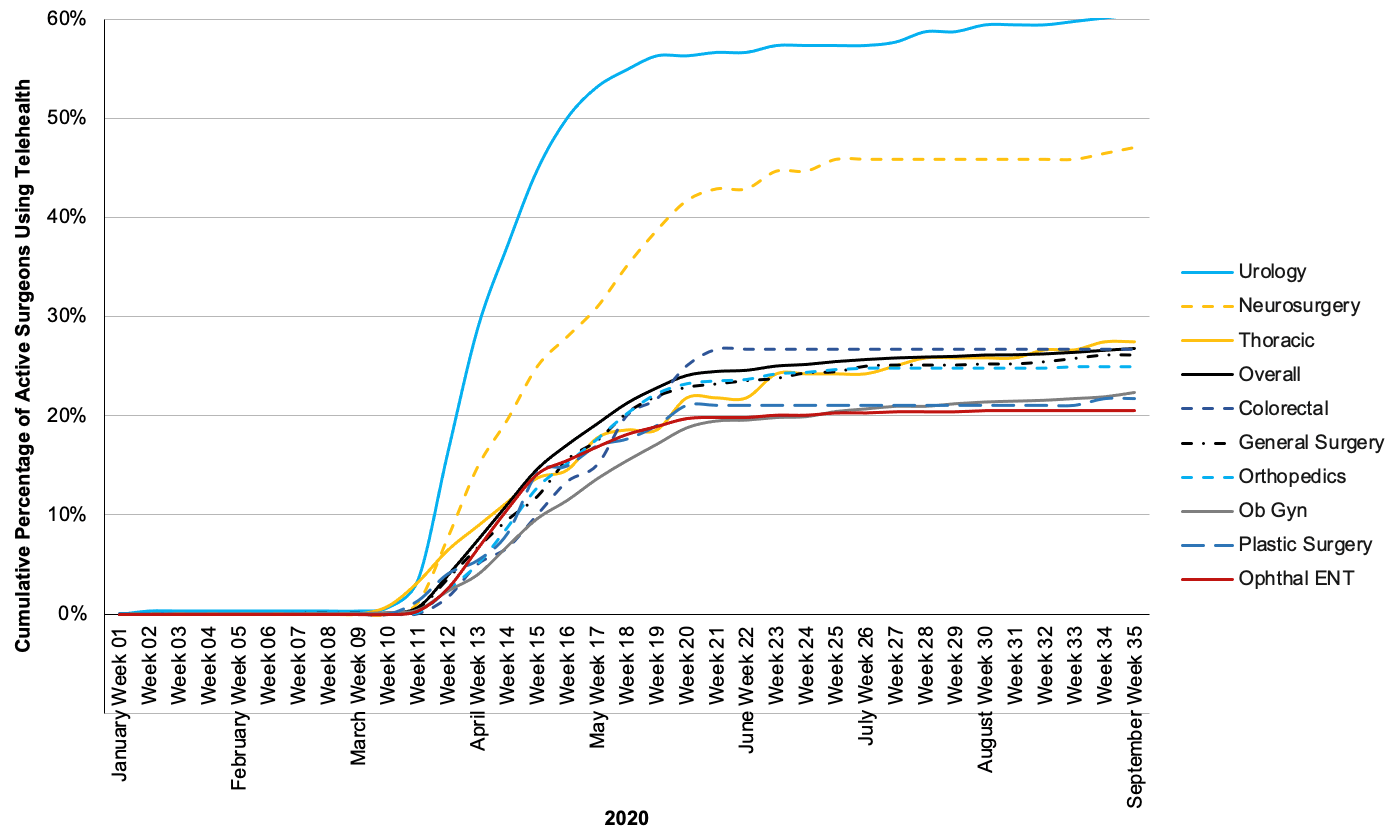
There were two distinct periods of telehealth use: an early pandemic (fast uptake) and late pandemic period (slow decline). The slow decline that occurred during the late pandemic period indicated the reopening of clinics in June, and an increase in more in-person visits being used again. These are shown as Period 2 and Period 3 in the preceding figures.
Of note, our study looks at new patient visits because of the way that claims data is collected. Anecdotal evidence suggests that surgeons used telehealth even more for their established patients and for follow-up visits post-surgery. Although telehealth might save patients time and money in traveling to clinic, needing child care, and missing work, this type of consultation would be most appropriate for patients without post-operative complications.
It was noticed that telehealth provided access to surgical care for a significant proportion of patients during the COVID-19 pandemic. Any sustained use of telehealth will require ongoing updated policies and infrastructure to ensure patients have continued access to this option for their care.
Please reach out to the Michigan Value Collaborative at michiganvaluecollaborative@gmail.com for further information.
Learning Health Systems and Quality Improvement
The mission of the Michigan Value Collaborative (MVC) is to improve the health of Michigan through sustainable, high-value healthcare with a vision to help provide the right care, at the right time, at the right cost. As part of this, MVC helps its members better understand their performance using robust multi-payer data, customized analytics, and at-the-elbow support. In addition, MVC fosters a collaborative learning environment to enable providers to learn from one another and share best practice. All of this is designed to help members respond to change, drive quality improvement, and improve performance.
Improving performance is often easier said than done – a phenomenon often referred to as the “60.30.10 Challenge”. Following the review of health learning systems in Australia, this phenomenon was identified as a key challenge that the healthcare system has faced for three decades. Despite change and areas for improvement being identified throughout healthcare, only 60% of evidenced based care is provided to patients, 30% of care is identified as waste or duplication, and at least 10% of patients experience adverse events or medical harm. With this in mind, can the current healthcare system embrace the many new technologies and advancements in medicine on the horizon?
While these new advances in technology have the ability to improve care and prolong life, there is conversely an addition of complexity and increased risk with utilizing them. It is important to understand that healthcare systems are complex and typically do not respond in a linear way to change. A collaboration of healthcare providers set up in Australia realized some key activities for improvement initiatives within health care systems . These activities were included in the setting up of the collaborative known as the Translational Cancer Research Network and involved incentives, resources, administrative support to provide encouragement, collaboration and reduced constraints, data support, and expertise in implementation science. A number of new projects such as increased consumer engagement and improvement in diagnosis for various cancers came out of involvement in this network.
While root-cause analysis has long been used to identify medical failures, this may not be the best method to effectively establish safety protocols to prevent further harm due to the complex pathways within healthcare that are infrequently repeated. Instead, healthcare needs to take a different approach by introducing models of care that promote collaboration, exceed independent specialties, and advocate for combining hospital, primary care, community agencies, and elder care to navigate well-informed patients through evidenced based healthcare pathways along the continuum of care. There is a need to shift the paradigm and learn from what is going well and those that are successful. By spreading good practices across all healthcare systems, allowing healthcare teams to effectively improve processes in real time, and teaching clinicians to manage data and understand continuous improvement methods, a learning system can be developed.
By creating a learning system, efforts to improve care can be better aligned. Drivers of the system include a commitment to improvement, being ready and prepared for change, being aware of the capacity of and barriers to progress, knowledge of implementation strategies, and lastly providing leverage and resources to learning. In addition, data can be utilized by these fluid learning systems to aid patient and clinician decision-making. It is hoped that a flexible system with relevant information and data to make the right decision, and the ability to adjust processes will help to reenergize clinicians, enabling them to provide increasingly appropriate, safer, and higher quality care with less waste.
The Michigan Value Collaborative (MVC) can help you by providing claims data across 40 different medical and surgical conditions. Additionally, we have regular workgroups that meet to share best practices. If you are interested in custom analytics for your institution, joining a workgroup or want to learn more about what MVC has to offer, please contact the Coordinating Center at michiganvaluecollaborative@gmail.com.