Health equity is a top priority for providers across the country, who are keenly aware of the prevalence and exacerbation of existing health inequities. The state of Michigan in particular ranks poorly in measures of population health and social determinants of health (SDOH), which represent a huge opportunity to improve equity and health outcomes for patients. Health equity is currently a key strategic focus of the Michigan Value Collaborative (MVC) Coordinating Center in the years ahead, as well as for Blue Cross Blue Shield of Michigan (BCBSM). As work in this area grows, some suggest that better data collection is the next critical step to improving health equity.
Data collection is the focus of BCBSM’s latest initiative - the SDOH Standardized Data Collection and Aggregation Initiative - which offers incentives to physician organizations (POs) for collecting and submitting SDOH screening data. Its goal is to increase SDOH screening by primary care physicians during annual wellness visits as well as enhance SDOH data submitted to the Michigan Health Information Network (MiHIN), Michigan's nonprofit statewide health information network.
This data will be used in the short term to improve data conformance and SDOH definitions within the Michigan provider community. Ideally, this initiative will help BCBSM to improve care coordination between providers, identify gaps in resources and community-level social need trends, and provide analytics and reporting to the provider community. The long-term goal is to reduce disparities and improve health outcomes.
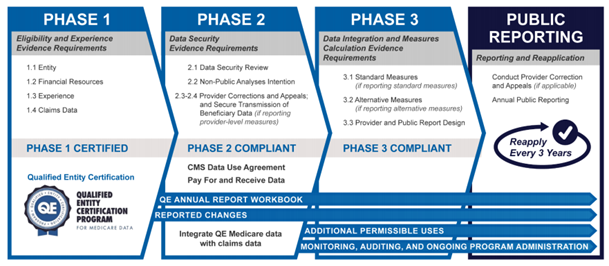
There are multiple pathways for POs to participate, primarily by either submitting screening data through MiHIN’s SDOH use case, or by developing infrastructure to enable participation in MiHIN’s SDOH use case. BCBSM sees this incentive program as an important step toward ensuring all patients receive the care they need.
“The SDOH initiative is valuable for both patients and providers because it encourages providers to screen for SDOH needs in patients and also encourages that the data from these screenings is exchanged in an interoperable way,” said Karolina Skrzypek, MD, Medical Director of Clinical Partnerships at BCBSM. “It is very important that providers across the state of Michigan have the ability to access SDOH screening data regardless of where the screening took place. Screening for SDOH needs by providers is the first step in helping to address these needs in our patients.”
These points were echoed by Martha M. Walsh, MD, MHSA, FACOG, Medical Director of Clinical Partnerships and Engagement at BCBSM, who said, “We know that when patients have SDOH needs, that it is more difficult for them to have their healthcare needs met and for patients to care for their chronic conditions. Our initial goal in having providers screen for SDOH needs is for patients to have their needs addressed at the point of care.”
Some POs are already actively submitting this data to MiHIN and can receive incentive payments for continuing to do so. The other pathways are focused on those who have capacity to store and extract SDOH data but are not submitting it to MiHIN, or those POs who don’t yet have the digital infrastructure in place. Helping all POs to achieve a similar capacity and submit their data to the same vendor will allow for a broader understanding of the gaps and communities in need of further funding.
“By aggregating this data, we hope to learn more about specific domains of need and geographic areas with the most needs so that we can start to address these more broadly,” said Dr. Walsh. “We hope that by screening for and addressing SDOH needs, we will start to be able to decrease disparities in care for our most vulnerable patients.”
Incentives for the MiHIN SDOH use case pathways are paid out of the BCBSM Physician Group Incentive Program (PGIP) reward pool. Therefore, any deadlines related to participation are based on PGIP payment cycles. Those POs wishing to participate in the October 2022 cycle should submit their opt-in form and any other required materials by the end of August.
A separate value-based reimbursement (VBR) reward was created specifically for patient-centered medical home (PCMH) designated primary care physicians for completing SDOH screenings using Z codes. This VBR payment was available when the SDOH initiative launched in January. Provider offices had six months to work towards meeting the criteria to receive VBR effective 9/1/2022. Criteria for the 2023 cycle was previously announced and updates to the criteria will be provided during the upcoming BCBSM September PGIP quarterly meeting.
Any POs or providers interested in learning more about this initiative and the pathways for participating can read the full brochure here and submit questions directly to BCBSM at POPrograms@bcbsm.com. In addition, if your PO or hospital has success stories or insights that have resulted from collecting SDOH screening data, please consider sharing your story and insights with the MVC Coordinating Center at michiganvaluecollaborative@gmail.com.
Support for MVC is provided by Blue Cross Blue Shield of Michigan as part of the BCBSM Value Partnerships program. Although BCBSM and MVC work collaboratively, the opinions, beliefs, and viewpoints expressed by the author do not necessarily reflect the opinions, beliefs, and viewpoints of BCBSM or any of its employees. To learn more about the Value Partnerships program, visit www.valuepartnerships.com.