Next week marks the kickoff of American Heart Month, commemorating the more than 600,000 Americans who die from heart disease each year and raising awareness about strategies that support heart health. Cardiac rehabilitation (CR) is one of those critical strategies, with the second full week of February each year dedicated to promoting its role in reducing the harmful effects of heart disease. In support of efforts to promote this life-saving program, MVC will host a CR-focused workgroup on Feb. 16, from 2-3 p.m., with MVC Co-Director Mike Thompson, Ph.D., assistant professor in the Department of Cardiac Surgery at Michigan Medicine, as its guest speaker. He will highlight some recent efforts to increase patient enrollment.
This is the third time MVC has hosted a workgroup dedicated to CR utilization; the first took place during last year’s CR week in February 2022 and featured guest presenters Steven Keteyian, Ph.D., Director of Preventive Cardiology at Henry Ford Medical Group, and Greg Merritt, Ph.D., patient advocate, in a discussion about strategies for increasing CR use. The second in November 2022 featured Diane Hamilton, BAA, CEP, of Corewell Health Trenton Hospital, who discussed addressing transportation barriers as an obstacle to CR attendance.
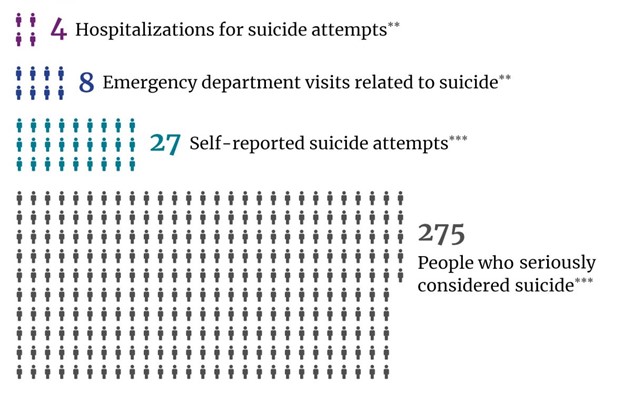
CR is a medically supervised program encompassing exercise, education, peer support, and counseling to help patients recovering from a cardiac event, disease, or procedure. There is high-quality evidence that it saves lives and money. A 2016 meta-analysis estimated that for every 37 coronary heart disease patients who attended CR, one of their lives was saved on average. Additionally, the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2) and the Michigan Value Collaborative (MVC) came together recently to measure the impact attributed to CR for percutaneous coronary intervention (PCI) patients treated between 2015 and 2019, and estimated 86 lives saved, 145 readmissions avoided, and approximately $1.8 million in savings.
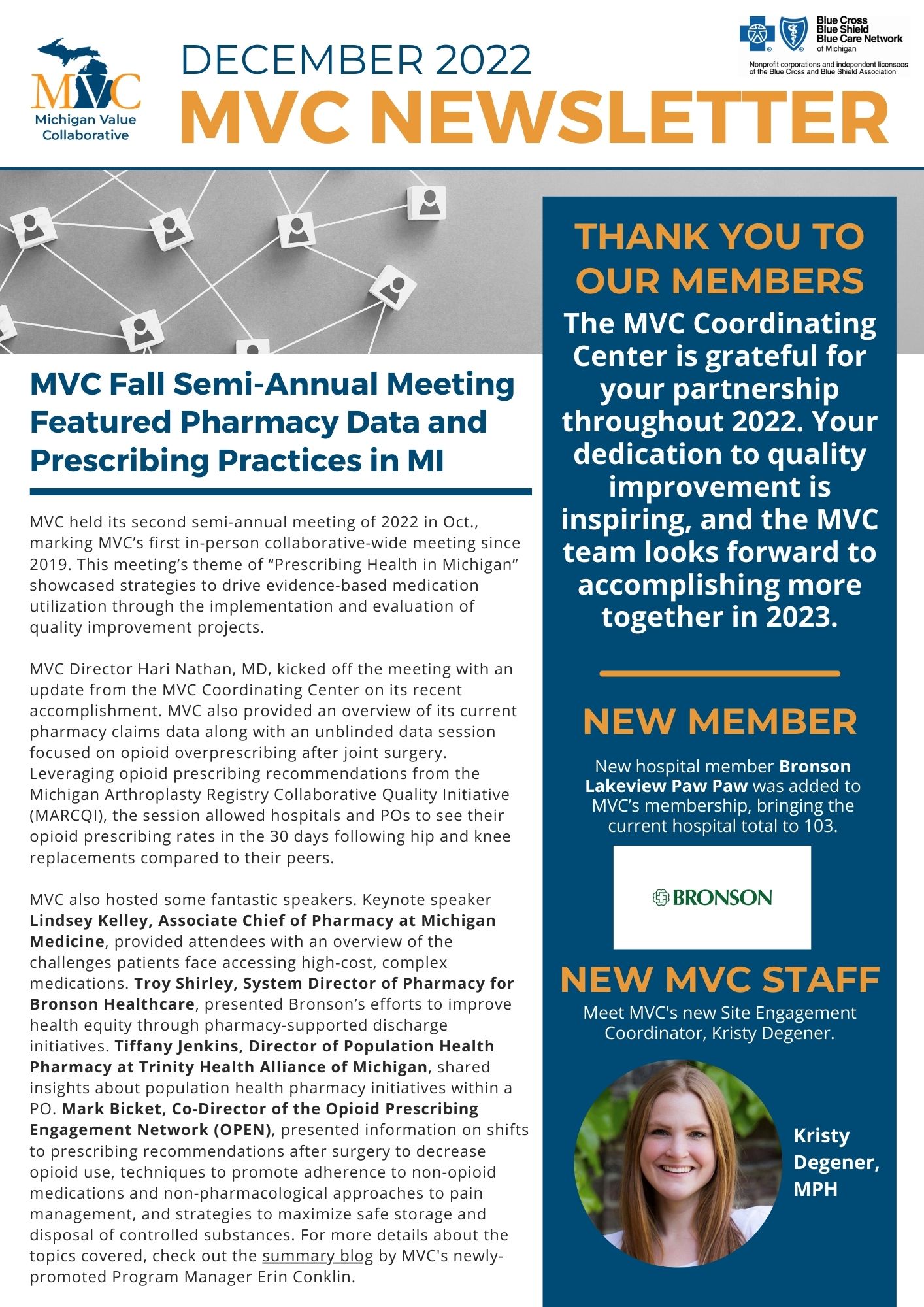
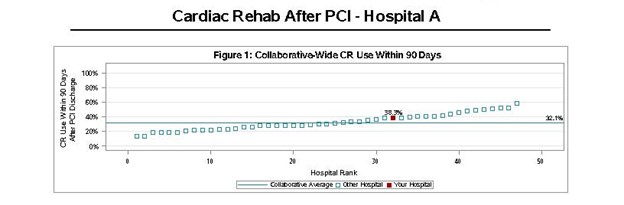
Despite the evidence in favor of its clinical impact and cost-effectiveness, CR remains heavily underutilized, with only one in three eligible Michiganders participating. MVC’s hospital-level cardiac rehab reports showcase similar findings (Figure 1). These reports were rebranded recently under the new Michigan Cardiac Rehabilitation Network (MiCR) umbrella in partnership with BMC2. They measure whether and when patients started CR at MVC hospitals and how long they kept going. The collaborative-wide average for PCI patients, for example, was 38.3%, with hospital rates ranging from approximately 10%-60%. Such a wide range in patient participation rates suggests MVC member hospitals would benefit from the insights of top-performing peers.
Figure 1.
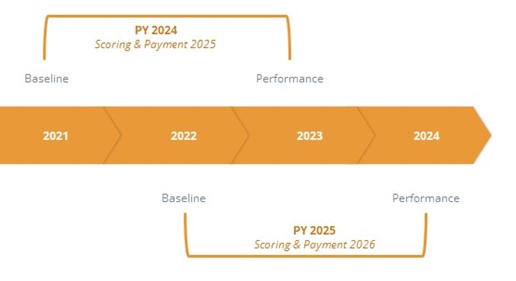
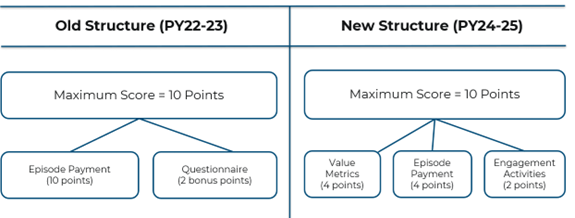
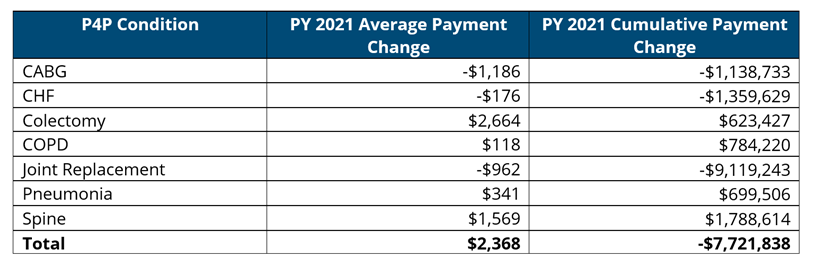
MVC is pursuing several strategies to address this critical gap in utilization. The upcoming Feb. 16 workgroup will be one of several CR-focused workgroups offered throughout 2023. The Coordinating Center decided to offer workgroups on this topic in part because of its recent incorporation of a CR measure into the MVC Component of the BCBSM Pay-for-Performance (P4P) Program. MVC member hospitals were recently asked to make metric selections for the upcoming Program Year 2024-2025 cycle, and as of February 2023 just over one quarter of hospitals elected to be scored on their CR rates for the new value metric component of the MVC measure. These hospitals will receive more P4P points if their CR utilization rate improves over time or is greater relative to their peers. These hospitals are currently treating the patients who will make up their performance year data for Program Year 2024 of the MVC measure. Therefore, MVC aims to offer tailored workgroups to support those sites being scored on CR utilization, most likely incorporating some unblinded data presentations and highlighting key resources and practices for quality improvement purposes.
The MVC team hopes these efforts to facilitate peer learning within the collaborative will help hospitals across the state improve CR participation. Doing so would save the lives of patients and improve the value of healthcare in Michigan. Sites that selected CR as their value metric component of the MVC P4P measure are encouraged to attend; however, anyone interested in this area of healthcare is welcome. Those interested in attending may register here. Please contact the MVC Coordinating Center with any questions at Michigan-Value-Collaborative@med.umich.edu.