In the United States, disproportionate rates of chronic disease and illness are commonly documented among communities of color. National Minority Health Month (NMHM) takes place throughout April as a way to raise awareness about health disparities among minority groups and how racism and barriers to healthcare access have historically marginalized such groups. According to the CDC, health equity is “the state in which every individual has a fair and just opportunity to attain their highest level of health.” To achieve such a state, extensive efforts are necessary to address systematic injustices and support equitable access to healthcare.
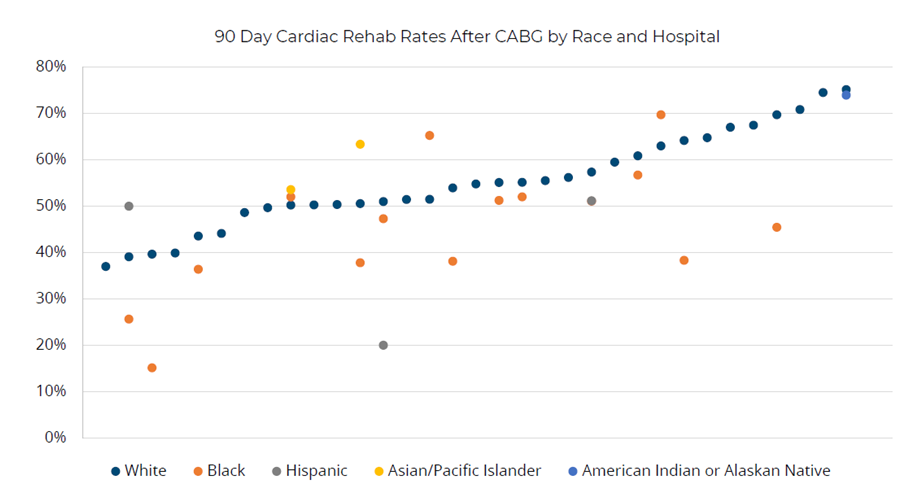
At MVC, emphasizing this vast issue and supporting change begins with one critical step: identifying and quantifying current disparities within patient communities in Michigan. MVC is utilizing claims-based data analytics to identify differences in care for specific patient demographic groups. For instance, in a recent analysis of MVC claims, MVC found differences by race in the rates of patients attending cardiac rehabilitation after a coronary artery bypass graft (CABG), with lower average utilization rates among some minority groups compared to patients who are white and higher average utilization rates among other minority groups (Figure 1). There are also significant disparities in cardiac rehabilitation utilization rates after CABG by gender and payer categories. Highlighting the landscape of current healthcare utilization may help quality improvement teams understand where disparities exist within their patient populations and prompt discussions about the social and environmental circumstances that may contribute to such findings.
MVC also recently collected surveys from its members on their health equity priorities, challenges, and initiatives to date. The survey results will be summarized at MVC’s upcoming spring collaborative-wide meeting, and some of the survey responses will be further expanded upon and shared with members as blogs and case studies to provide real-world examples of the work happening in hospitals across the state. Since health equity is a strategic priority for many healthcare teams, MVC’s recent survey was developed to help members understand what others are doing and facilitate shared learning on this topic.
However, there is also much to learn from national examples and strategies. In December 2022, for example, Blue Cross Blue Shield of Massachusetts announced the creation of payment contracts that provide financial rewards to practices addressing racial and ethnic inequities in healthcare delivery. Dr. Mark Friedberg, Senior Vice President, Performance Measurement and Improvement at Blue Cross explained, “This encourages health care systems to increase their investments in developing, expanding and sustaining programs that produce measurable improvements in equity.” This financial investment is a huge breakthrough for Blue Cross which will allow healthcare providers and organizations to learn what barriers to care exist and methods of resolution.
Financial incentives focused on equity are also a large component of State Medicaid strategies. In California, Medicaid plans could earn incentive funds by demonstrating improvement in the two race/ethnicity groups with the lowest baseline vaccination rates. In Michigan, there are financial incentives for using withheld funds for improvement on a subset of quality measures within the African American and Hispanic population groups. As more states and systems begin to invest in financial incentives with equity goals, MVC is working to re-evaluate the methodologies and metrics of the MVC Component of the BCBSM Pay-for-Performance (P4P) Program for opportunities to similarly incentivize and reward achievement and/or improvement in equitable care delivery.
As health equity activity continues to grow and evolve, MVC is committed to expanding its data sources and reporting to support members' understanding of the needs of their patients. Studies emphasize that disparate health outcomes are closely related to social determinants/influencers of health (SDOH/SIOH), with social factors often predicting the incidence of illness and disease. It is for this reason that MVC has continued to incorporate Distressed Communities Index (DCI) data into patient demographic tables in MVC push reports, in addition to stratifying select outcome measures by relevant demographic categories. MVC continues to explore opportunities to integrate additional supplemental SDOH data sets into its analyses – a recent example was shared at MVC’s October collaborative-wide meeting presentation (see slides), which focused on the relationship between county-level social need indicators and post-discharge care utilization.
Organizational strategies and investments are rapidly growing and evolving within healthcare, and will likely be necessary for years to achieve meaningful improvements. MVC is eager to support member activity in this space to achieve high-value care for all and will continue to highlight the excellent work and success stories happening across its membership. If you have a success story to share or would like to request a custom analysis focused on a specific patient population, please contact the MVC Coordinating Center.