This January, healthcare organizations and advocacy groups across the country are promoting Healthy Weight Awareness Month, as well as innovations in weight loss procedures. In alignment with this national conversation, MVC recently hosted its first workgroup of 2023 with a guest presentation by Oliver Varban, MD, FACS, FASMBS, Associate Director at the Michigan Bariatric Surgery Collaborative (MBSC), about obesity in Michigan, the main challenges of treatment, and how MBSC uses data to improve surgical management outcomes. The aim of such workgroups is to impart relevant data, best practices, and success stories for the benefit of MVC members and partners working in that clinical area.
According to data from CDC, the prevalence of obesity increased from 30% to 42% over the past 20 years, with 41% of Americans currently considered clinically obese. Excess body weight is associated with many different conditions and comorbidities (e.g., certain types of cancer, heart disease, diabetes, and stroke) and is a risk factor for increased severity and fatality of various conditions, such as those who experienced more severe illness from COVID-19 infection. Clinical management interventions range from screening and lifestyle changes to medication and surgery.
Identification and treatment of obesity often begins by measuring a patient’s body mass index (BMI), an estimate of body fat based on height and weight. The CDC uses BMI to measure obesity, but this measure falls short in several ways. For one, the accuracy of the measurement is lower among men, the elderly, and those in the intermediate BMI ranges. In addition, racial groups experience differing levels of disease for a given BMI. On its own BMI is not an accurate predictor of health. There are also a number of complex connections to social determinants of health since patients residing in environments with more limited access to healthy food and physical activity often have higher BMIs.
MBSC has been working to support quality improvement in healthy weight management since 2005 and aims to innovate the science and practice of metabolic and bariatric surgery through comprehensive, lifelong, patient-centered obesity care. MBSC utilizes its extensive clinical registry data to generate tools that support clinicians and patients in decision-making, including several patient- and provider-facing tools that outline a patient’s likely risks, benefits, and costs for various treatment pathways.
Given obesity’s prevalence and association with other chronic conditions, improved outcomes for patients managing obesity have far-reaching implications. Therefore, MVC and MBSC partnered last year to measure the value of bariatric surgery in treating diabetes, one of the most common and costly chronic conditions. According to the American Diabetes Association, $1 in $7 healthcare dollars are spent treating diabetes and its complications, and patients diagnosed with diabetes face 2.3 times the average person's healthcare costs. The analysis performed by MVC and MBSC was largely driven by existing evidence in the literature that bariatric surgery resolved or improved Type 2 diabetes symptoms in a large proportion of patients (Varban et al., 2022). Using its rich administrative claims data sources, MVC helped analyze pre-surgery and post-surgery receipt of diabetes medications, which was used to estimate the overall impact across Michigan and its estimated cost savings due to a decrease in post-surgery diabetes medication prescription fills.
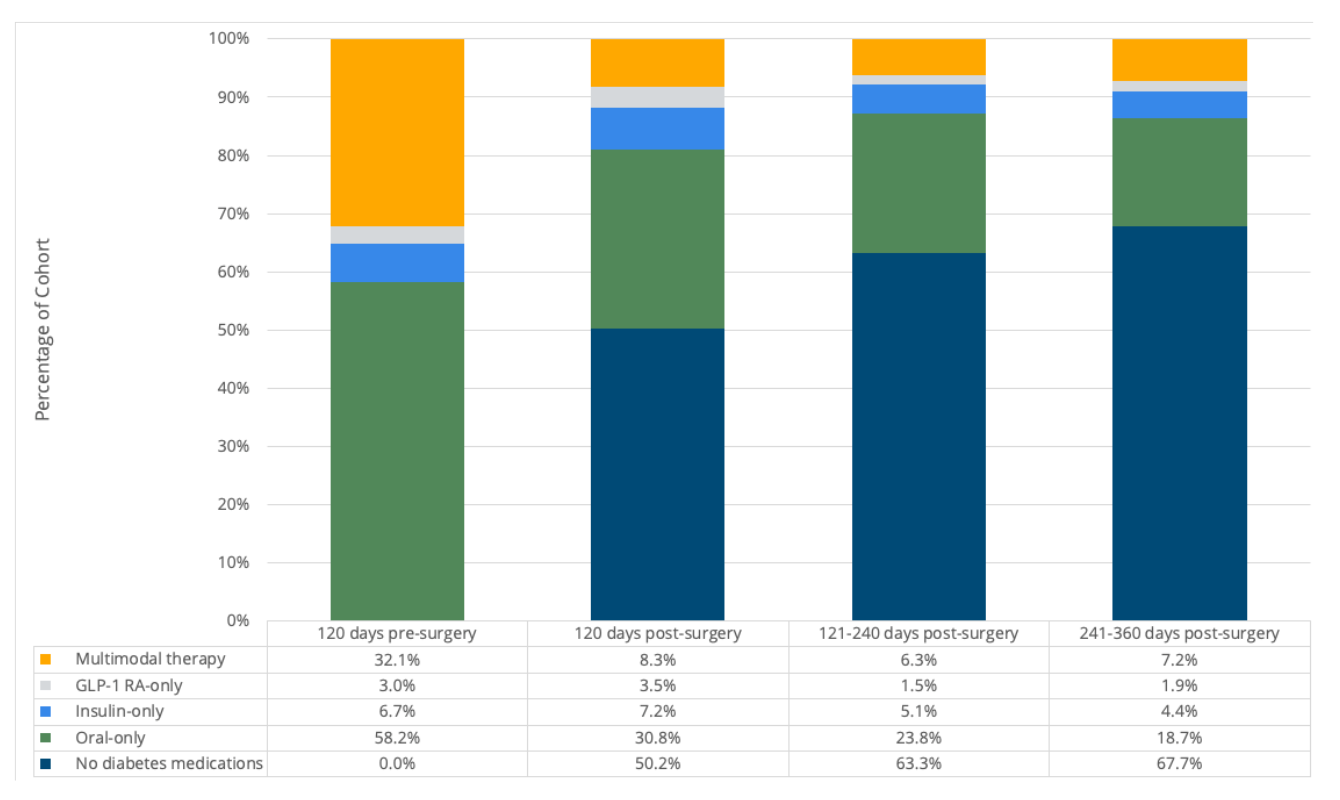
The most impressive finding of the analysis was a significant decrease in the percentage of bariatric surgery patients who filled any diabetes prescription post-surgery (Figure 1), with over 50% of patients who previously used diabetes prescriptions taking no medications within 120 days post-surgery. This amounted to an annual cost savings of about $4,133 per patient. Five years post-surgery, the continued estimated cost savings from reduced reliance on prescriptions ($20,665) surpassed the average price-standardized total episode cost of bariatric surgery ($14,832). These results provide evidence of statewide clinical outcome improvement and cost savings for Type 2 diabetes following bariatric surgery. A summary of this return-on-investment analysis was developed and publicized by MBSC and MVC in August 2022.
Figure 1.
This analysis was also evidence of the opportunities for cross-collaboration and information sharing in obesity care—between primary care providers, chronic disease management care teams, and bariatric surgeons; between collaborative quality initiatives with varying clinical, value-based, and socioeconomic focuses; and between providers, their patient, and their patient’s families. Obesity is a clinical diagnosis with extensive social complexities and implications for one’s physical and mental health. Improving support and care for those in seek of treatment requires intentional, innovative collaboration.
The complete recording of Dr. Varban’s recent MVC Health in Action workgroup presentation and the discussion that followed are available on MVC’s YouTube channel. Those with questions about any of the above-mentioned materials or analyses are welcome to contact the MVC Coordinating Center at Michigan-Value-Collaborative@med.umich.edu. MVC’s next workgroup takes place on Tues., Jan. 24, from 11 a.m. - 12 p.m., featuring a guest presentation by Karla Stoermer Grossman, MSA, BSN, RN, AE-C, Clinical Site Coordinator at the Inspiring Health Advances in Lung Care (INHALE) Collaborative Quality Initiative. Register to join us and hear about INHALE’s approach to improving outcomes for patients with asthma and chronic obstructive pulmonary disease.
