Participation in cardiac rehabilitation (CR) programs is a crucial strategy for improving cardiac health outcomes. Participation reduces the risk of all-cause and cardiovascular-specific mortality, reduces readmissions, and enhances the patient’s quality of life. Despite the identifiable benefits, Michigan patients underutilize this high-value program, falling well below the 70% participation goal set by the Million Hearts Initiative. Therefore, the Michigan Value Collaborative (MVC) and several of its partners have identified CR as a high-value service for which they endeavor to drive improvement.
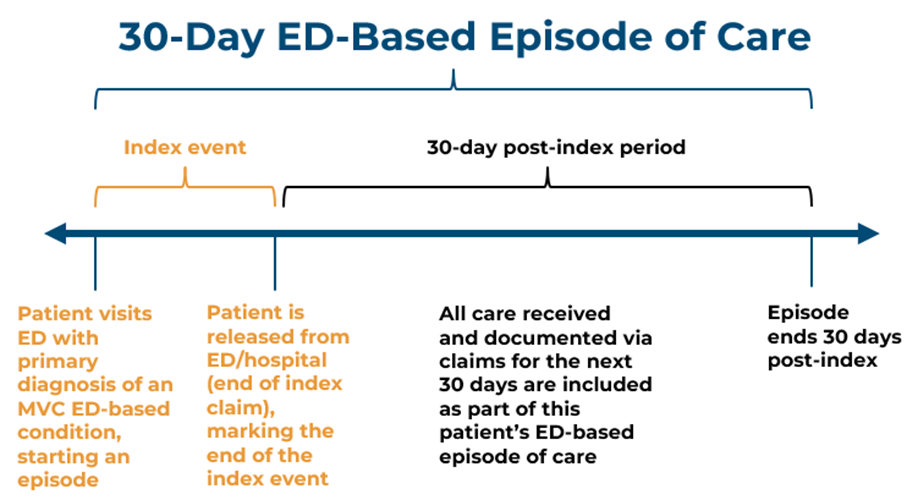
In support of this effort, MVC recently distributed the 2023 version of its CR reports to members with data on CR-eligible patients following discharge for heart attack (AMI), heart valve repair or replacement (TAVR or SAVR), coronary artery bypass procedure (CABG), percutaneous coronary intervention (PCI), and congestive heart failure (CHF). These reports were generated using MVC claims-based episodes of care with patient index admissions between 1/1/19-12/31/21 for multiple insurance plans, including Blue Care Network (BCN) HMO Commercial, BCN Medicare Advantage, Blue Cross Blue Shield of Michigan (BCBSM) PPO Commercial, BCBSM Medicare Advantage, and Medicare Fee-for-Service.
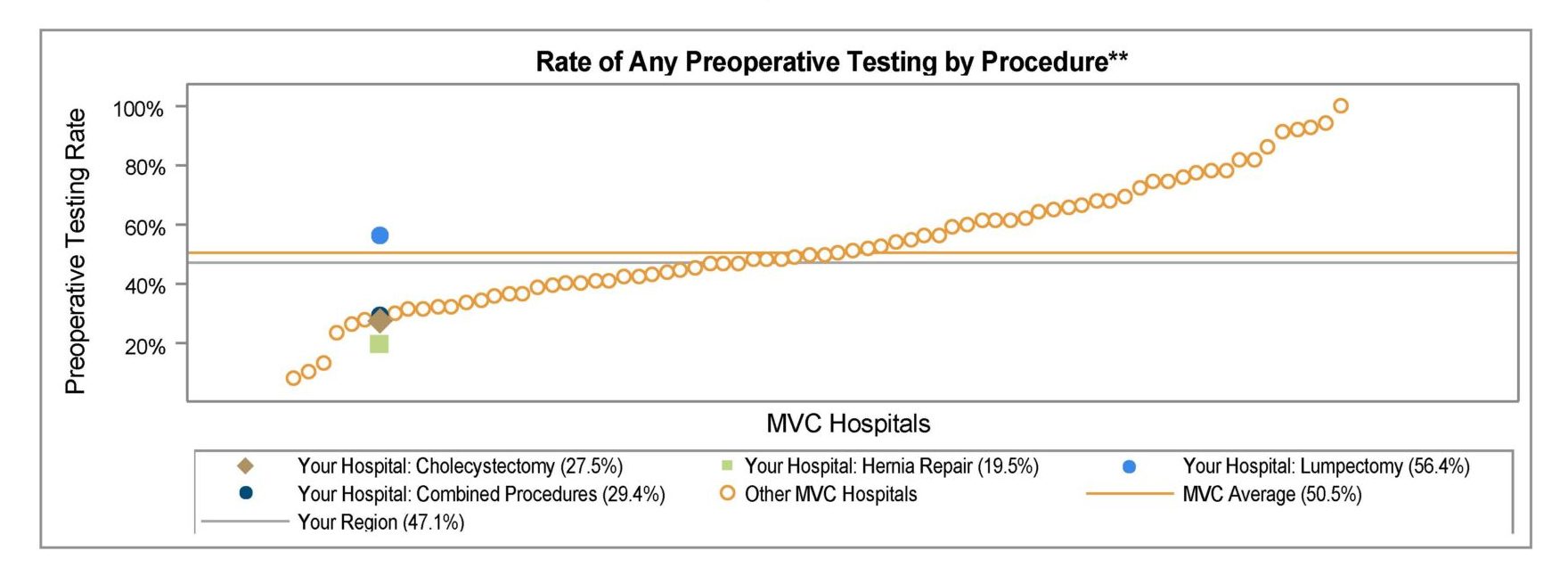
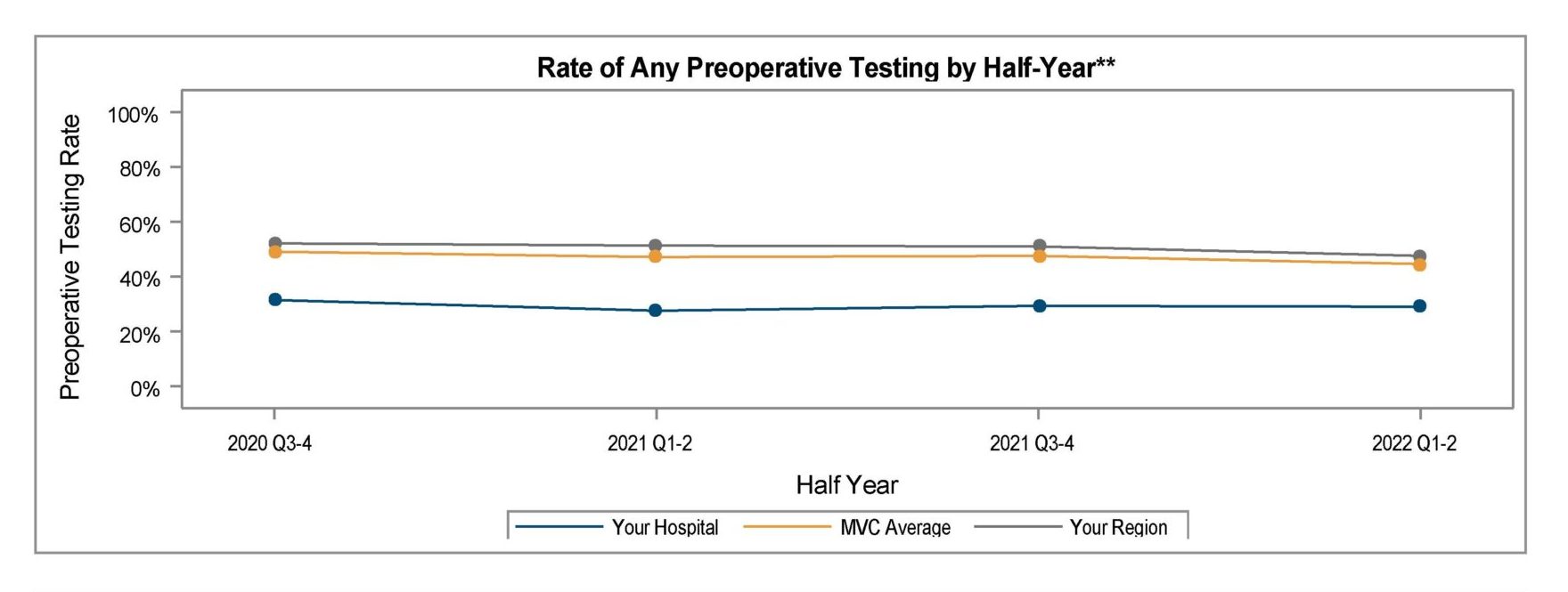
Hospitals received data on a specific procedure or condition if they had no fewer than 20 cases in the reporting period for that condition/procedure. The report pages include figures for a variety of CR metrics, including participation rates after discharge, quarterly trends in participation between 2019-2021, mean days to first CR visit among participating patients, and the mean number of visits completed among participating patients.
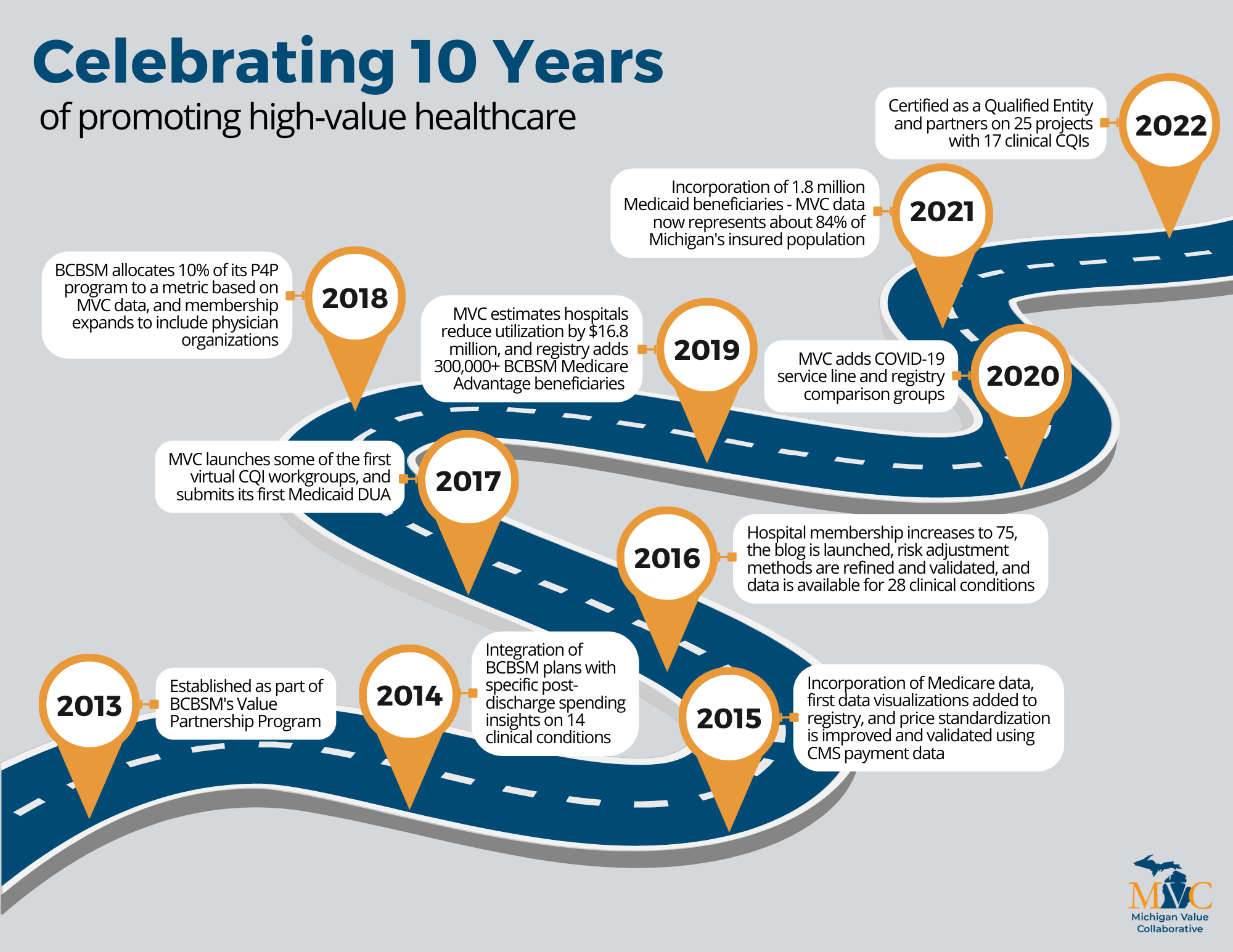
MVC generates these hospital-level reports as a product of the Michigan Cardiac Rehabilitation (MiCR) Network, a partnership between MVC, Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2), and the Michigan Society of Thoracic and Cardiovascular Surgeons Quality Collaborative (MSTCVS-QC). The MiCR Network strives to increase participation in CR for all eligible individuals in Michigan.
Given the current status of CR participation across the state, the MiCR Network is tracking progress toward two utilization goals: 1) for 40% of all eligible AMI, TAVR, SAVR, CABG, and PCI (referred to as the “Main 5”) patients to attend at least one CR session within 90 days of their hospital discharge, and 2) for 10% of all eligible CHF patients to attend a single CR session within one year of a CHF-related hospitalization.
In developing these reports, MVC found that the collaborative-wide average participation rate within 90 days of discharge for the "Main 5" procedures was approximately 36%, below the statewide goal of 40%. Similarly, MVC’s analysis found 3.2% of eligible CHF patients participated within 365 days of discharge, 6.8% below the statewide MiCR goal of 10%.
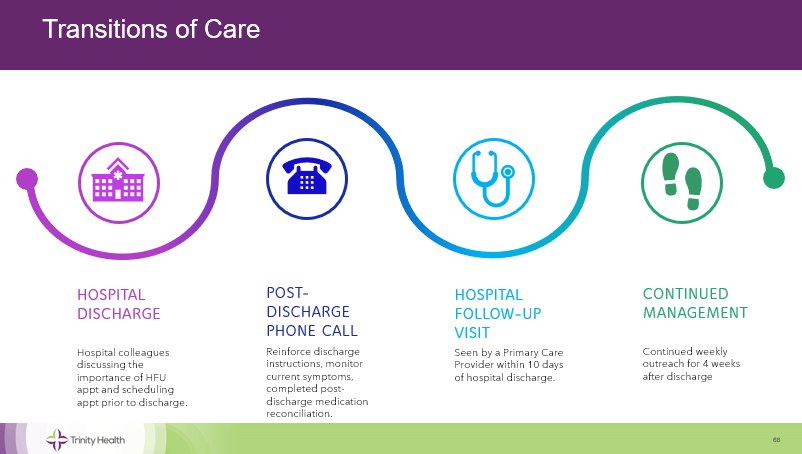
The report also offers patient population demographics intended to help hospitals identify disparities in participation. Research evidence suggests that white males are more likely to utilize CR than women or patients of color, likely due to several socioeconomic and cultural factors. Hospitals are encouraged to consider any gaps showcased in their demographic snapshot and consider the provision of additional, tailored strategies that increase referral and participation among those patients.
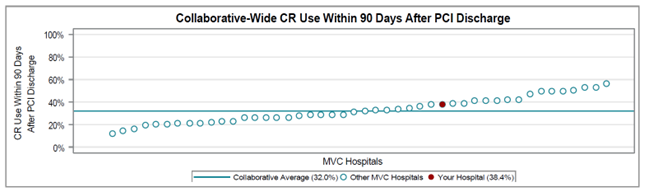
Other high-level findings from the report included varying averages in CR participation by the procedure type. CABG and SAVR, more clinically invasive procedures, had the highest utilization rates at 54.9% and 51.3% respectively, whereas patients being treated for the chronic condition of CHF were the least likely to attend (3.2%). There is also wide interhospital variation in utilization rates for each procedure. For example, the collaborative-wide CR utilization rate after PCI is 32%, but hospital rates range from just above 10% to nearly 60% (Figure 1).