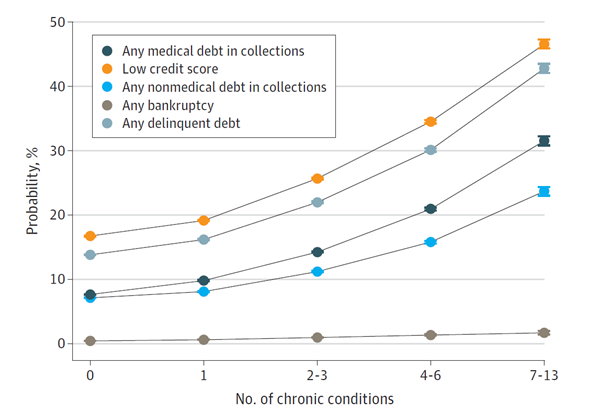
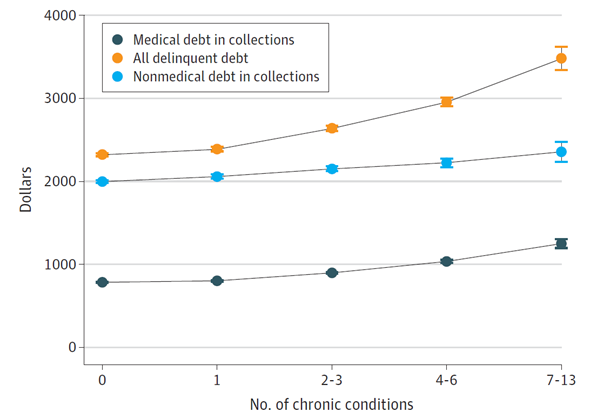
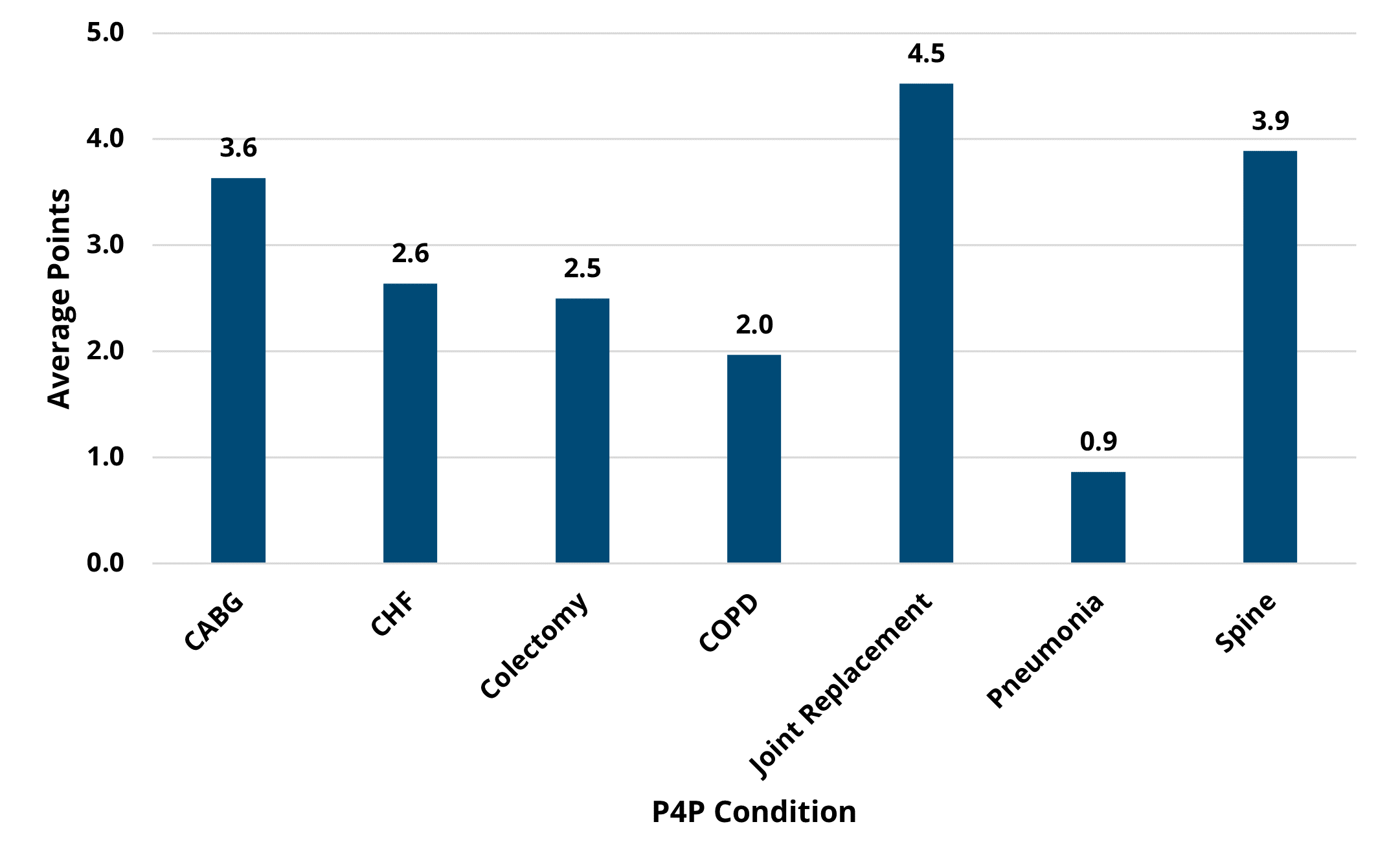
“We were expecting an association between adverse financial outcomes and chronic disease burden, but we were really struck by the magnitude and strength of the association that we found,” said Dr. Becker. “To see such a large increase in rates of adverse financial outcomes by chronic conditions really emphasizes that there is a crisis of financial instability among individuals with high chronic disease burden.”
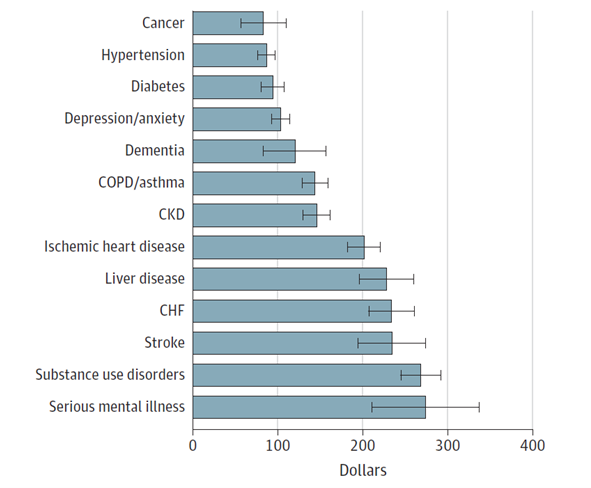
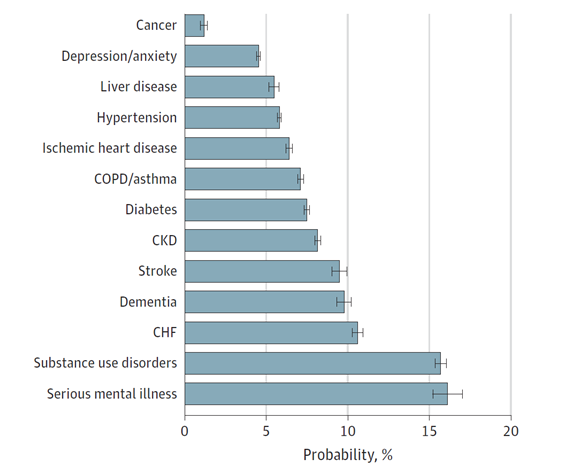
Such significant variation across chronic conditions could be the result of several factors, such as some conditions requiring more costly treatments and high out-of-pocket expenses, and others making it more likely that patients miss work or cannot stay employed. The implications of such findings are impressive given the already high rate of patients with multiple chronic conditions—4 in 10 adults in the U.S. have more than one chronic condition—and the fact that poorer financial health is linked to more forgone medical care, worse physical and mental health, and greater mortality. Chronic conditions are already the leading causes of death and disability as well as the leading drivers of America’s $4.1 trillion in annual healthcare costs.
Dr. Becker and her colleagues were clear that their analysis did not determine causality—it is still unknown whether poor financial health leads to the development of chronic conditions or vice versa. Therefore, they advocated for the value of further analyses to determine underlying causes, which would inform how to approach improvements. The authors offered that if poor financial health causes additional chronic disease, then new social safety-net policies intended to reduce poverty rates may be beneficial. If chronic diseases are leading to poorer financial outcomes, then changes to the design of commercial insurance benefits could provide additional protections from medical expenses for costly chronic conditions.
“Additional work to determine the causal mechanisms of this association is crucial,” said Dr. Becker. “If we don’t figure out why this association exists, and who is most vulnerable, we can’t hope to design social policies to help protect patients from adverse financial outcomes.”
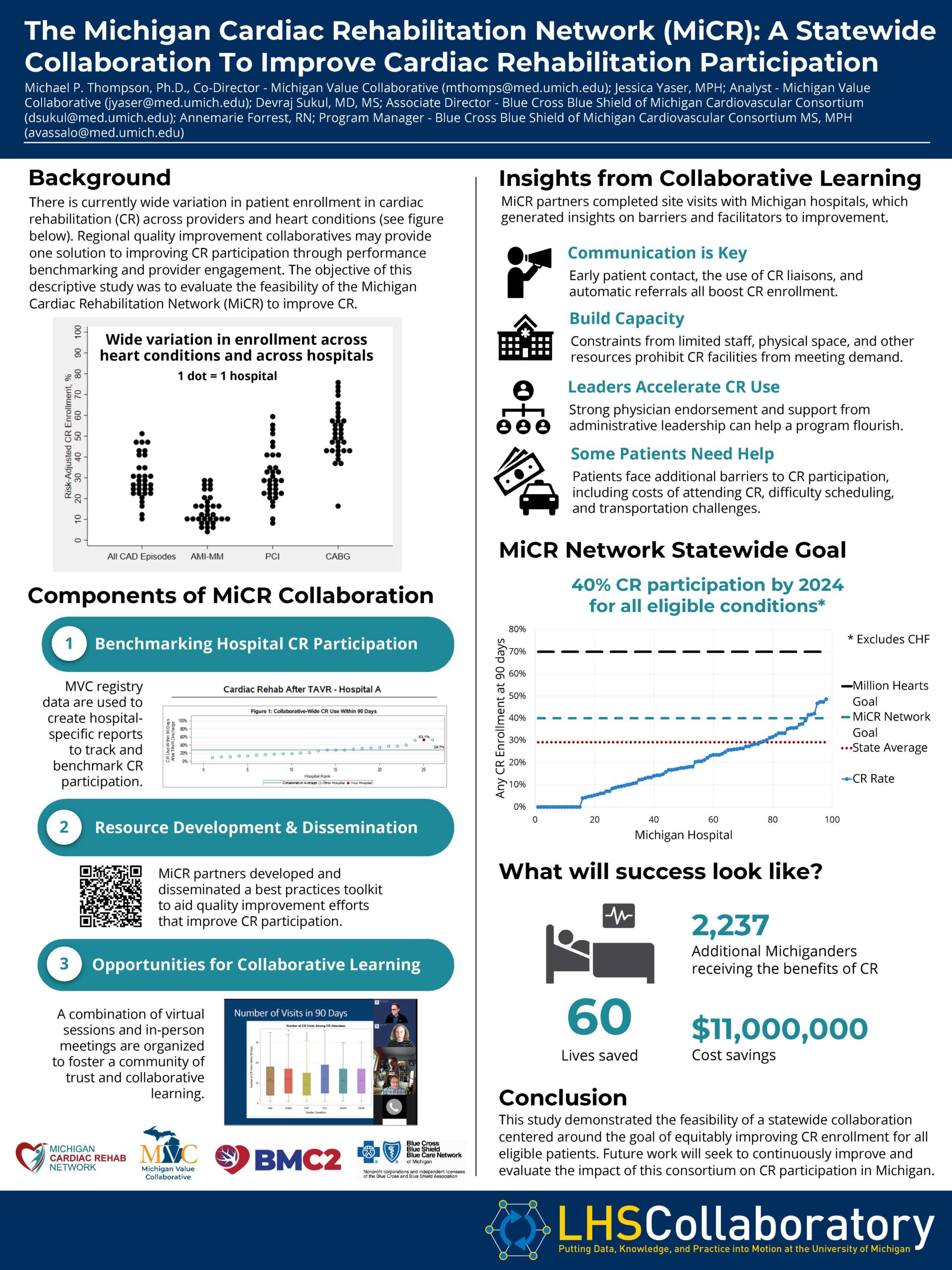
One of MVC’s core strategic priorities is intentional partnerships with fellow Collaborative Quality Initiatives (CQIs) and quality improvement collaborators. In the future, MVC hopes to do more with commercial credit report data given its unique uses and implications. It is the Coordinating Center’s hope that this work will help identify at-risk populations, understand how economic instability affects health outcomes, and generate insights that help working-age adults recover and return to work after major health events. The MVC team will continue exploring uses for this data in 2023 and engage its partner CQIs and collaborators to identify additional reporting opportunities for members.
As was recently highlighted in MVC’s 2022 Annual Report, MVC contributed to several other projects in the last 12 months similar to the analysis completed by Dr. Becker and her colleagues. MVC data and expertise also contributed to projects that resulted in new condition and report development, return on investment estimations for various healthcare initiatives, and additional insights on care delivery and patient outcomes. MVC will continue to identify partnerships and projects that leverage its rich data to achieve more sustainable, high-value healthcare in Michigan.
Publication Authors
Nora V. Becker, MD, PhD; John W. Scott, MD, MPH; Michelle H. Moniz, MD, MSc; Erin F. Carlton, MD, MSc; John Z. Ayanian, MD, MPP
Full Citation
Becker NV, Scott JW, Moniz MH, Carlton EF, Ayanian JZ. Association of Chronic Disease With Patient Financial Outcomes Among Commercially Insured Adults. JAMA Intern Med. 2022; 182(10): 1044–1051. doi:10.1001/jamainternmed.2022.3687.