MVC distributed a new push report on Aug. 28, highlighting the components and methods for MVC’s newest measure: health outcome variation for all-cause readmissions. The goals of the recently distributed push reports are to familiarize hospital members with the measure methodology as well as provide a first look at their hospital’s performance.
This measure was developed with the goal of addressing common challenges by MVC’s members in identifying and addressing gaps in health outcomes within their patient populations. A survey distributed to the MVC collaborative in 2024 identified barriers such as insufficient data and insufficient financial investments as key causes for lingering variation across their patient population. With the introduction of MVC’s health outcome variation measure, MVC seeks to quantify the magnitude of hospital-level variation in all-cause readmission rates between payer groups using an index of variation calculation. Readmission rates are risk adjusted for patient demographic and comorbidity data, as well as for non-medical drivers of health.
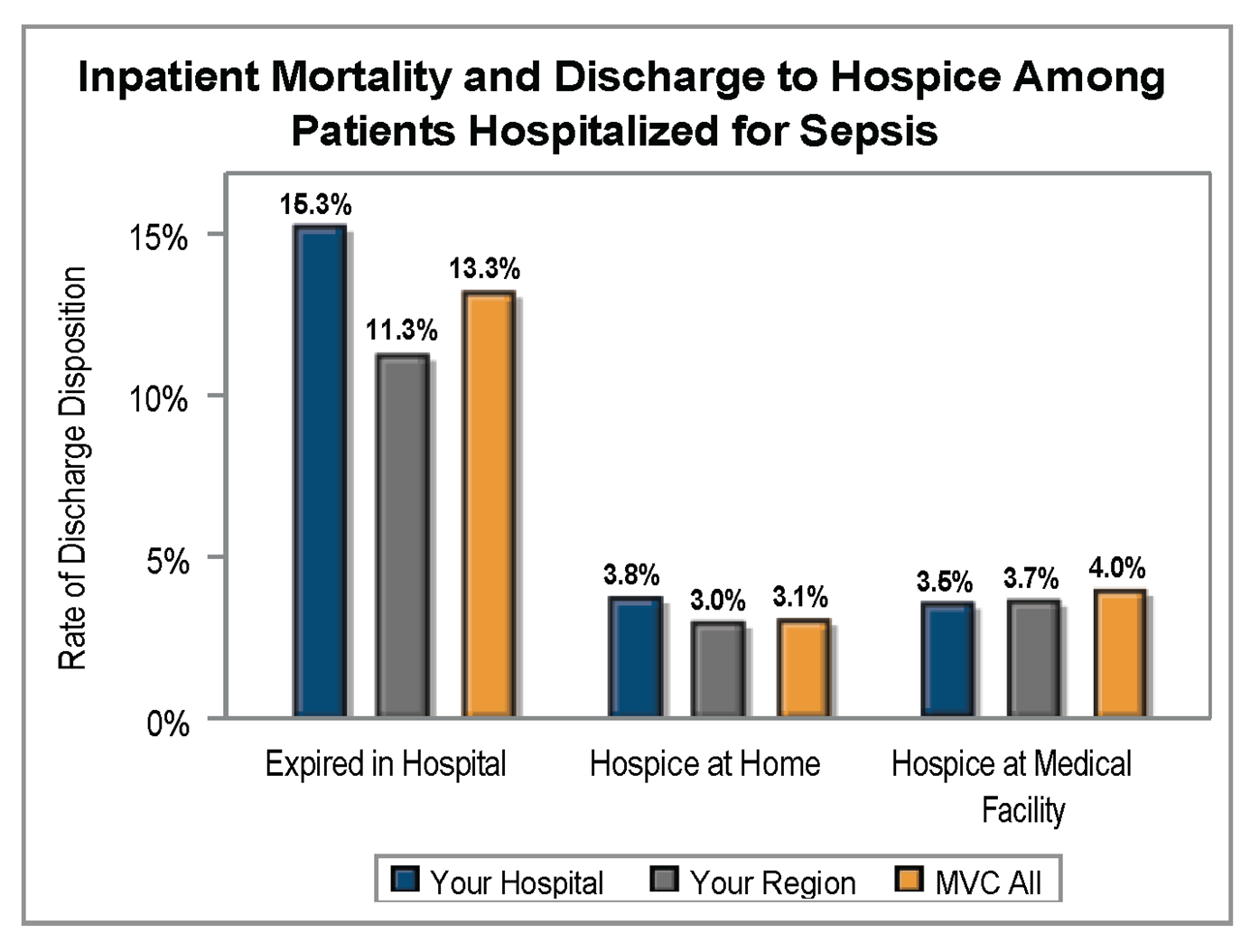
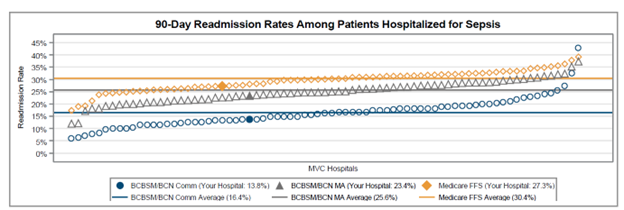
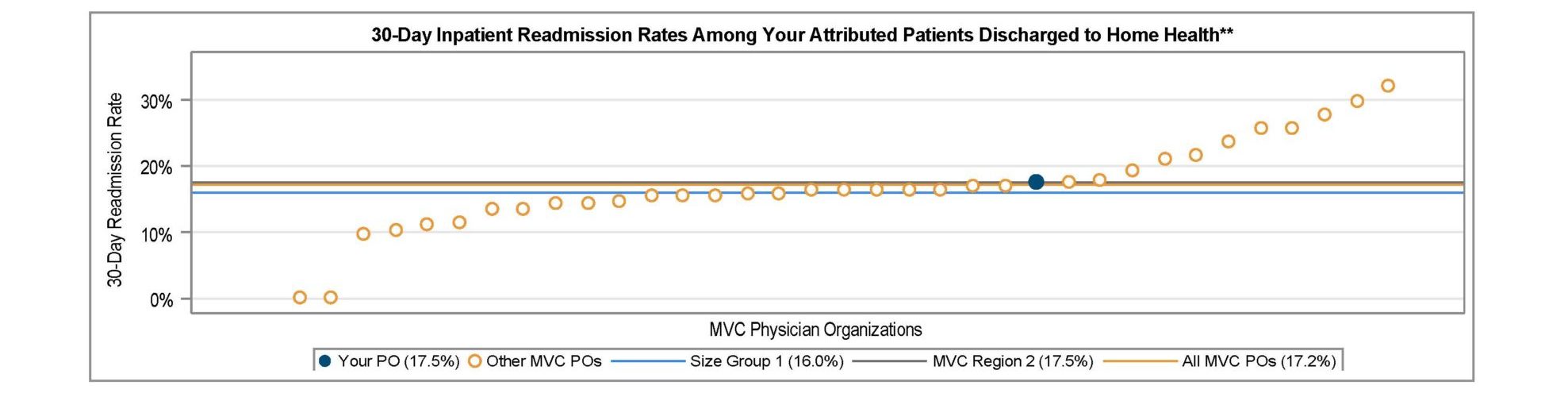
The first two pages of the push report provide a step-by-step walkthrough of the index calculation, beginning with the calculation of absolute differences in hospital-level readmission rates by payer group compared to the hospital-level average readmission rate. The five payer groups included in these calculations are BCBSM and BCN Commercial, BCBSM and BCN Medicare Advantage, Medicaid only, Medicare FFS only, and patients dual-eligible for Medicaid and Medicare; dual-eligible patients have been pulled out of the Medicaid only and Medicare only categories. This initial step helps to highlight which payer group(s) have a higher readmission rate than the hospital’s average rate (Figure 1).
Figure 1.
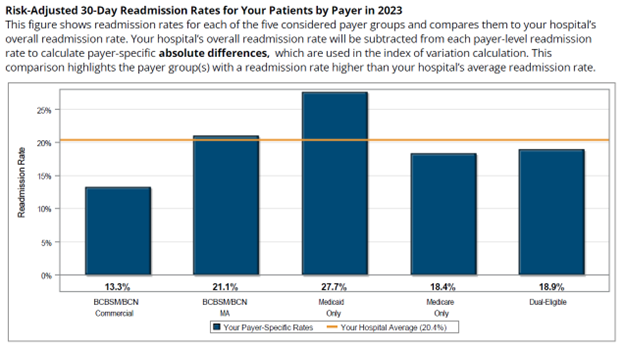
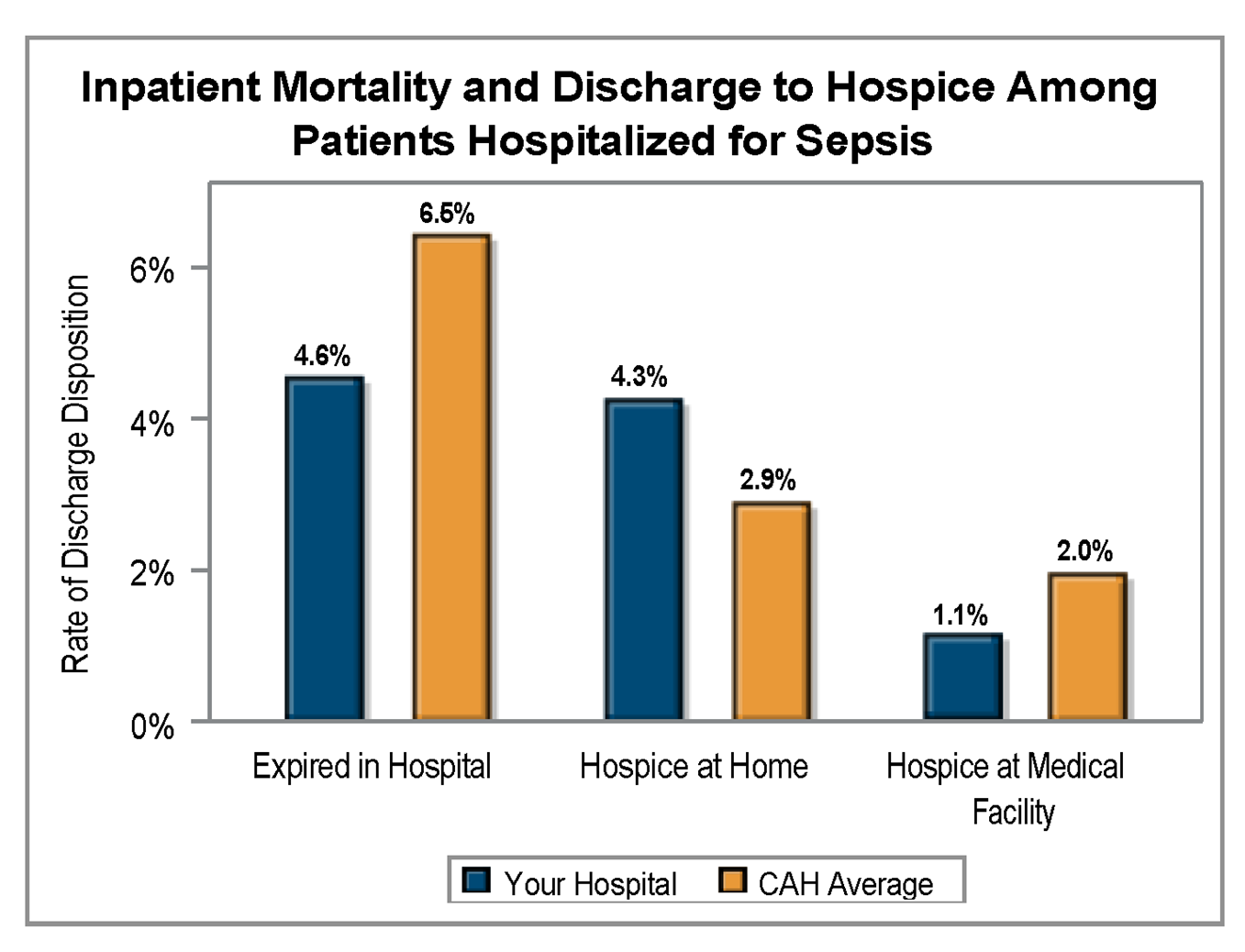
The next step in the methodology is to calculate a hospital’s index of variation using absolute differences in payer-specific risk-adjusted readmission rates compared to the hospital’s risk-adjusted average readmission rate. These payer-specific absolute differences are multiplied by the respective payer population proportion to yield weighted differences (Figure 2). The sum of those weighted differences across all five payer groups yields the hospital’s index of variation. This index calculation indicates the magnitude of payer-specific differences in risk-adjusted readmission rates within a hospital. A higher value indicates a larger spread in a hospital’s payer-specific risk-adjusted readmission rates as well as opportunities to develop strategies that reduce gaps in care across patient groups. A lower value is desired and indicates less variation in a hospital’s risk-adjusted readmission rates across payers.
Figure 2.
MVC first announced this measure at its fall 2024 collaborative-wide meeting, where Senior Advisor Jim Dupree, MD, MPH, announced its inclusion in the next cycle of the MVC Component of the BCBSM Pay-for-Performance (P4P) Program. Scoring on this measure will be offered in the Program Year (PY) 2025 scorecards with no points attached and thereafter will be worth one point in the PY 2026-2027 cycle.
Similar index or composite measures have been utilized by other health organizations, and MVC’s risk-adjusted measure can help identify hospital-level preventable differences in readmissions. Hospitals will earn the health outcome variation point by improving relative to their own baseline index or by performing well relative to their peers (i.e., having an index at or below the collaborative-wide median index).
As hospitals review their provided push report and become familiar with this new health outcome variation measure, they are encouraged to reach out to MVC with any questions.