Diabetes is commonly cited as the most expensive chronic disease in the U.S., accounting for over $37 billion in 2017. As many as 1 in 10 Americans have been diagnosed, 90-95% of whom have Type 2 diabetes. Management of Type 2 diabetes involves healthy eating, physical activity, and often taking medication prescribed by a doctor, such as insulin, other injectable medications, or oral diabetes medicines to help manage blood sugar. It is both clinically and economically significant, then, that the Michigan Value Collaborative (MVC) was recently part of an analysis that estimated over $76.5 million in insurance savings on prescription diabetes medications after patients underwent metabolic surgery.
MVC identified these savings in partnership with the Michigan Bariatric Surgery Collaborative (MBSC) last year and published their findings in a co-authored research letter in JAMA Surgery. This work was featured recently by the medical news site Medpage Today.
The partner project was initiated by MBSC in 2022 to help assess the impact of bariatric surgery on prescription fills for diabetes medications across the state of Michigan, driven largely by existing evidence in the literature that bariatric surgery resolved or improved Type 2 diabetes symptoms in a large proportion of patients (Varban et al., 2022). MBSC is a regional group of hospitals and surgeons that aim to innovate the science and practice of metabolic and bariatric surgery through comprehensive, lifelong, patient-centered obesity care.
Using its rich administrative claims data sources, the MVC team first analyzed pre-surgery and post-surgery receipt of diabetes medications, which was then used to estimate a high-level snapshot of the overall impact across Michigan. MVC's analysis included estimated cost savings to health insurance providers that could be attributed to a decrease in post-surgery diabetes medication prescription fills.
The analysis used bariatric surgery episodes for Roux-en-Y Gastric Bypass (RYGB) and sleeve gastrectomy hospitalizations. It was limited to bariatric surgery patients with a diagnosis of Type 2 diabetes who filled an outpatient diabetes medication prescription prior to their discharge. The analysis focused on episodes with index admissions between 2015 and 2021 for Blue Cross Blue Shield of Michigan (BCBSM) PPO Commercial and BCBSM Medicare Advantage plans for individuals who were continuously enrolled in a prescription sub-plan. This amounted to 760 patients with Type 2 diabetes undergoing gastric bypass (22%) or sleeve gastrectomy (78%) between 2015 to 2021.
In the 120 days prior to surgery, MVC found that 88% of patients filled an outpatient oral diabetes medication prescription, 30% filled an insulin prescription, and 21% filled a GLP-1 receptor agonist prescription. From the 120 days pre-surgery to the 120 days post-surgery, there was a significant decrease in fills for any diabetes medication (p<.001). The most frequent change in medications between pre- and post-surgery was from oral diabetes medication to no diabetes medication. In the 1 to 120 days following surgery, half (50%) of patients filled no diabetes medication prescriptions, and in the 121 to 240 days following surgery, most patients (63%) filled no diabetes medication prescriptions (see Figure 1).
Figure 1.
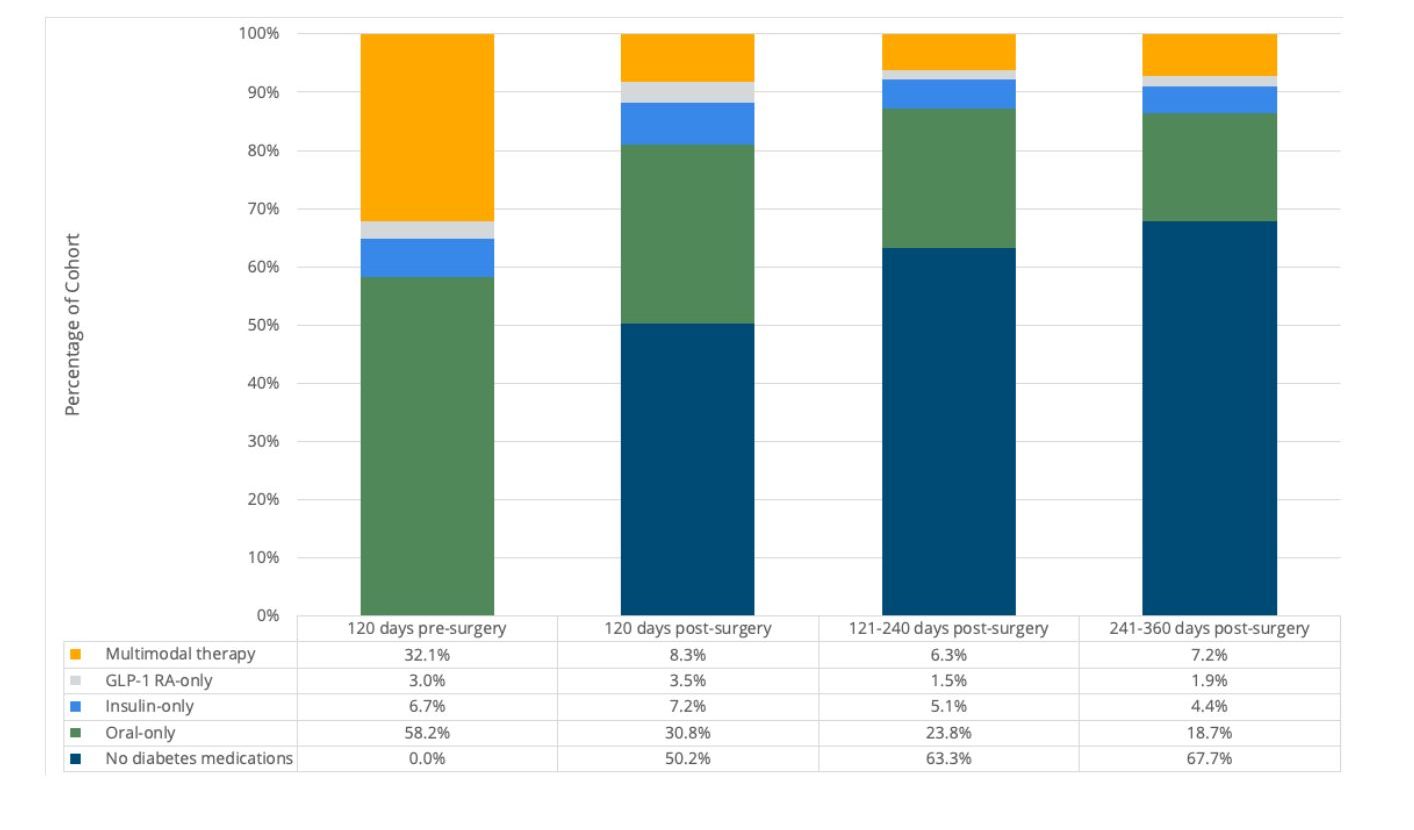
This amounted to an average decrease in diabetes prescription payments made by the insurance provider of approximately $4,133 per patient in the first year following surgery. Given that 34% of bariatric surgery patients have diabetes and 54,454 bariatric surgeries were performed in Michigan between 2015 and 2021, MVC estimated that insurance providers in Michigan saved $76.5 million on diabetes medications in the 360 days following bariatric surgeries in 2015-2021. In addition, data suggest that savings would continue to increase in future years due to long-term diabetes remission and cost benefits from optimized diabetes management. These results provide evidence of significant statewide clinical outcome improvement and cost savings for Type 2 diabetes following bariatric surgery.
These findings and their implications were also highlighted recently during an MVC workgroup featuring Dr. Oliver Varban of MBSC as the guest speaker. See below for a complete recording of his insightful presentation about bariatric surgery, its impact on chronic disease management, and more.
MVC’s expertise and data frequently result in partner projects like this; MVC completed three other CQI impact assessments last year (Figure 2). These projects are an example of MVC’s interest in CQI collaboration, which is also demonstrated through new condition and report development, data analysis and metric consultation, and data matching exercises that pair clinical and claims-based data.
Figure 2.
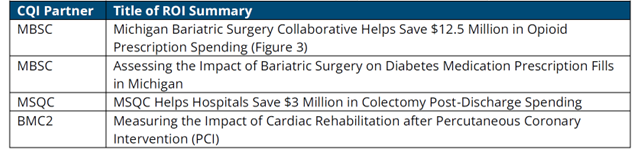
To request a copy of any of MVC’s completed impact assessments from 2022 or prior, please contact the MVC Coordinating Center.