MVC will soon distribute the 2023 version of its chronic disease management follow-up reports to members. This refreshed version provides summary data on patients eligible for follow-up care after discharge from hospitalizations for congestive heart failure (CHF) or chronic obstructive pulmonary disease (COPD).
MVC defines timely follow-up care as receipt of an in-person or remote outpatient follow-up visit within 30 days of hospital discharge to home or home health care and before any readmission, emergency department (ED) visit, or procedure. Patients admitted to a skilled nursing facility, long-term acute care hospital, or inpatient rehab within the 30-day episode were excluded. MVC’s follow-up analyses was performed using claims-based episodes of care with index hospital admissions between 7/1/2019 and 06/30/2022 for Blue Cross Blue Shield of Michigan (BCBSM) PPO Commercial and Medicare Advantage (MA), Blue Care Network (BCN) HMO Commercial and MA, and Medicare Fee-for-Service insurance plans. For each of the two chronic conditions included in the report, hospitals with at least 11 episodes per year for a given condition received that condition-specific data.
The report offers a comparison of demographic characteristics for CHF and COPD patients who received a follow-up visit within 30 days versus those who did not receive follow-up. Demographic characteristics tabulated for each condition include the percent of patients living in “at-risk” or “distressed” Zip codes as defined by the Economic Innovation Group’s Distressed Community Index, patients’ average number of comorbidities, the mean age of patients, and the distribution of race and ethnicity. MVC recently refined and expanded its reporting of race and ethnicity identities, and these updates were reflected in the report. Patients are grouped as Hispanic if their insurance provider categorized their combined race/ethnicity as Hispanic or their ethnicity as Hispanic. Additionally, MVC no longer combines smaller groups and discontinued its use of the terms “other” and “unknown.”
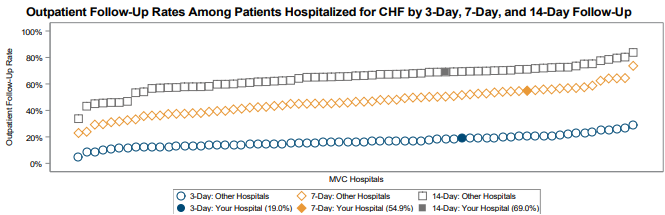
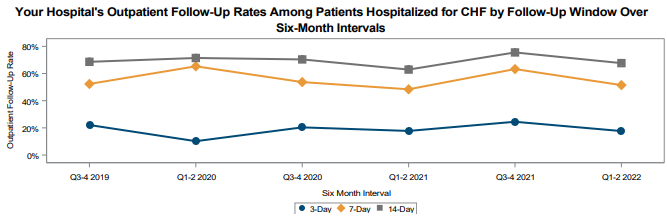
On the first page provided for each condition, hospital follow-up rates are provided for three windows of time compared to those at other MVC hospitals (Figure 1), as well as trends over time for each follow-up window (Figure 2). For CHF, follow-up rates are provided in 3-day, 7-day, and 14-day time windows. For COPD, follow-up rates are provided in 7-, 14-, and 30-day time windows.
The second page of condition-specific feedback includes a summary of average 30-day risk-adjusted, price-standardized total episode payments by follow-up status compared to statewide and regional averages. Among general acute care hospitals included in the analysis, the statewide total average payment for CHF episodes was $17,235 for patients who received follow-up and $20,069 for those who did not; for COPD episodes, the statewide average payments were $13,815 among those with follow-up and $16,056 among those without. In reports generated for Critical Access Hospitals (CAHs), payments were compared to averages across all MVC CAH members. Rates of 30-day follow-up were also compared by payers across the same groups.
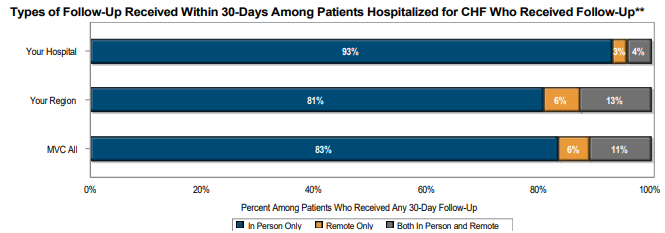
The final figure (Figure 3) in the report for each condition is a summary of follow-up method among those who received any follow-up care. Patients who received follow-up were categorized as having received only in-person follow-up visit(s), only remote follow-up, or both in-person and remote follow-up. MVC found that more than 80% of CHF and COPD patients statewide exclusively received in-person follow-up after a hospitalization.
If you have any questions or feedback about this report, please contact the MVC Coordinating Center.