In October, MVC’s health in action workgroup featured Hurley Medical Center’s Amanda Escalera-Torres, RD, Director and Nutrition Specialist for their Food FARMacy program. The presentation shared how the program helps support patients with chronic diseases by providing healthy food and nutrition education. The MVC Coordinating Center hosts workgroup presentations twice per month, covering a variety of topics including post-discharge follow-up, sepsis, cardiac rehabilitation, rural health, preoperative testing, and health in action.
Health in Action Workgroup: Hurley Medical Center
Hurley Medical Center’s Food FARMacy initiative was founded in 2017 to address Genesee County’s higher food insecurity rate of 13% (compared to the state average of 11%). It was funded by several grants and the Hurley Foundation to provide support services such as grocery access and nutrition education for Hurley patients. According to a 2024 MVC member survey, programs such as this are becoming more common in health systems across the state to address non-medical drivers of health such as food insecurity, economic and housing instability, and other factors. Food insecurity and being unable to access nutritious food has been linked to an increased risk of chronic diseases such as diabetes, cardiovascular disease, and certain types of cancer (Odoms-Young, 2024).
Patient Eligibility and Enrollment
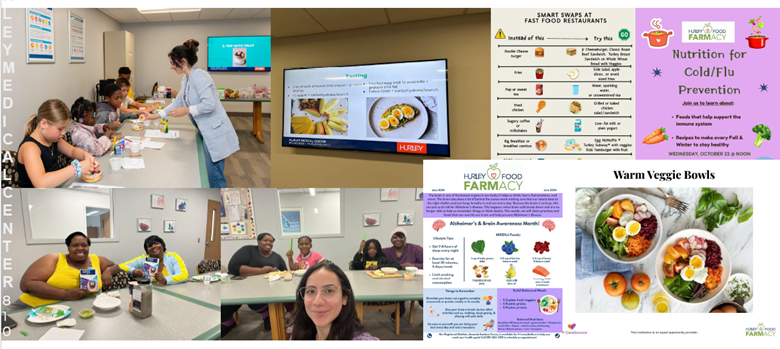
Escalera-Torres shared that patients are eligible to enroll in the Hurley Food FARMacy program if they are both food-insecure and have a chronic diet-related condition (Figure 1). Patients are referred to the program through avenues such as Hurley Medical Center inpatient or outpatient services, community health clinics, or primary care clinics throughout Genesee County. Once enrolled, patients receive monthly grocery support, meal kits, and nutrition classes for up to six months (Figure 2).
Figure 1.
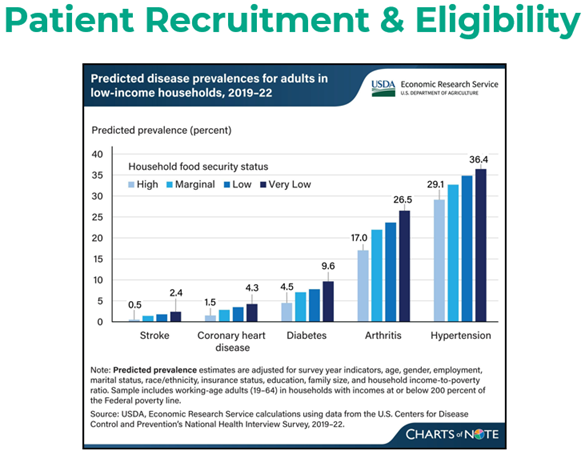
Figure 2.
Food Distribution Process
Each month, Hurley’s Food FARMacy program provides 300–400 patients with food access and education. Groceries are acquired through established contracts with local farmers and vendors and include locally sourced fresh fruits, vegetables, grains, meat, and more.
Program and Participant Success
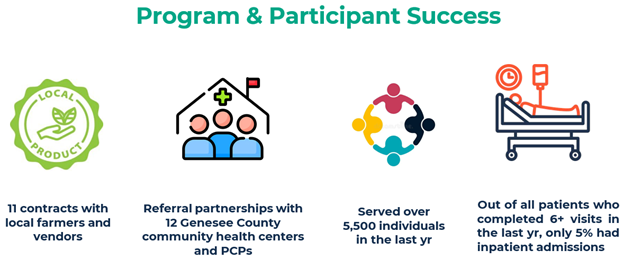
Hurley Food FARMacy expanded their food resources by increasing their farmer and vendor contracts to 11 this past year. This provides more accessibility for food and helps boost the local Michigan economy. The program also established 12 referral partnerships across Genesee County’s community health centers and primary care providers, allowing the program to serve over 5,500 individuals in the last year. Among the population served, only 5% of those who completed six or more Food FARMacy visits in the last year had an inpatient admission (Figure 3).
Figure 3.
Reducing Barriers
Following the presentation, Escalera-Torres answered questions about the ways the program has been able to reduce barriers to access, including how food supply was managed during the off-season and how they accommodated patients with transportation limitations. Escalera-Torres explained that the program did experience some difficulty acquiring fresh produce during the off-season but recently partnered with Great Lakes Farm to Freezer to ensure availability of a robust selection of nutritious foods year-round. To address patient transportation barriers, Hurley Food FARMacy partnered with Door Dash earlier in the year for a trial run of delivering food to participants. The program was well received but ended due to lack of continued funding. Patients with transportation barriers are now able to assign a proxy to pick up their groceries, which has helped reduce accessibility barriers.
The Food FARMacy program will continue to adapt and serve Genesee County patients providing quality food and improving nutritional awareness for chronic diet-related illnesses.
MVC Health in Action Workgroup, Oct. 23, 2025
MVC's cardiac rehabilitation workgroup for October was rescheduled for February 2026. View the complete 2026 workgroup calendar here.
MVC welcomes workgroup presenters from across Michigan to share their expertise, success stories, initiatives, and solution-focused ideas with MVC members. Please reach out to us by email if you are interested in being a workgroup presenter or submit a presentation proposal here.