The healthcare system has an immense wealth of information at its digital fingertips. Big data is constantly expanding from sources such as digitized patient records, patient wearables, medical apps, genome datasets, monitoring devices, and more. A critical challenge facing hospitals and health systems today is in effectively identifying strategies and personnel to utilize big data in a way that influences clinical care. Those that succeed in this task will find themselves in a much better position to advance care and improve patient outcomes.
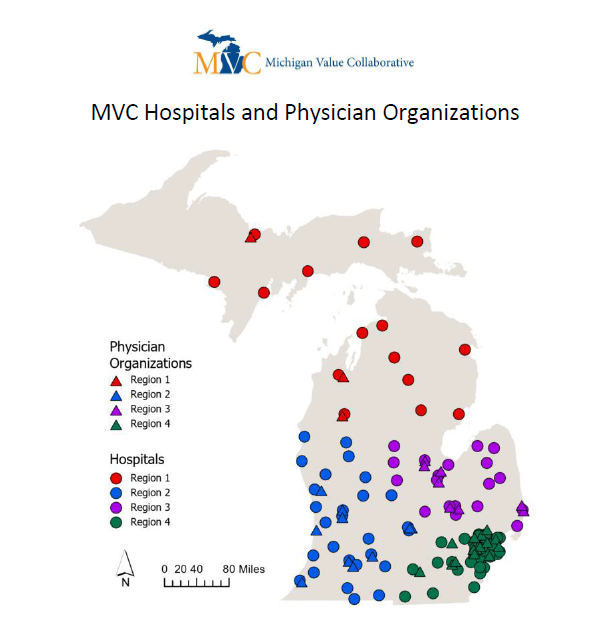
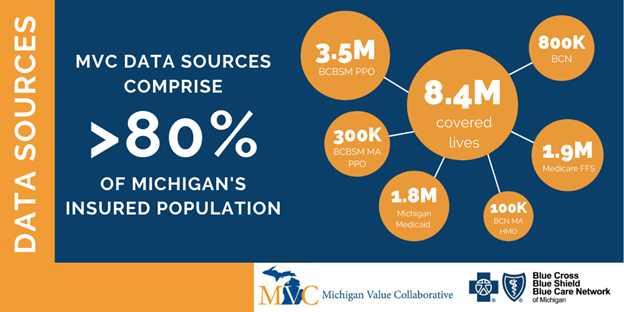
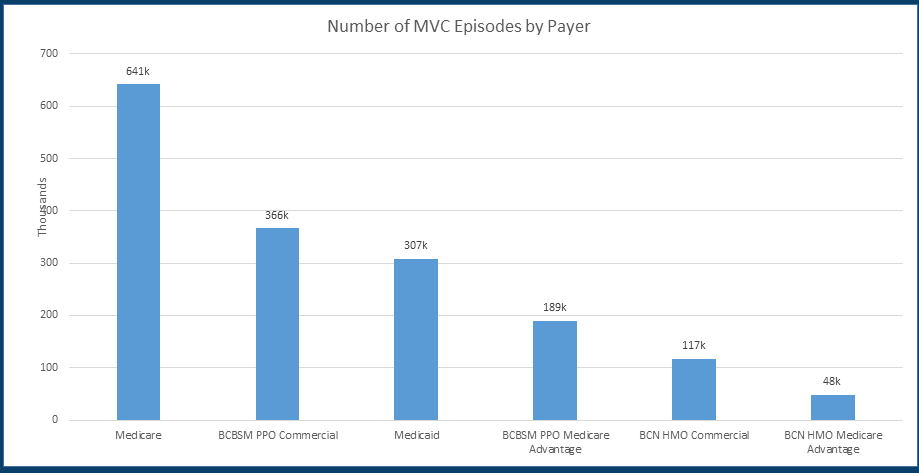
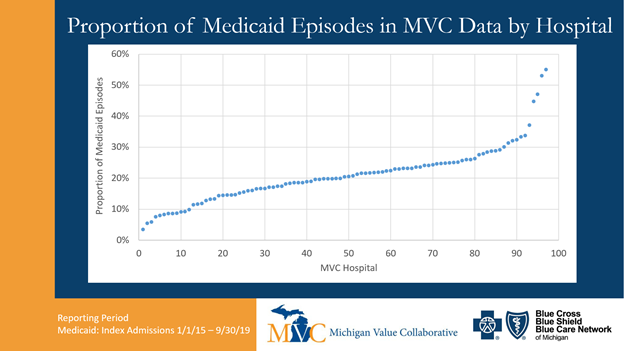
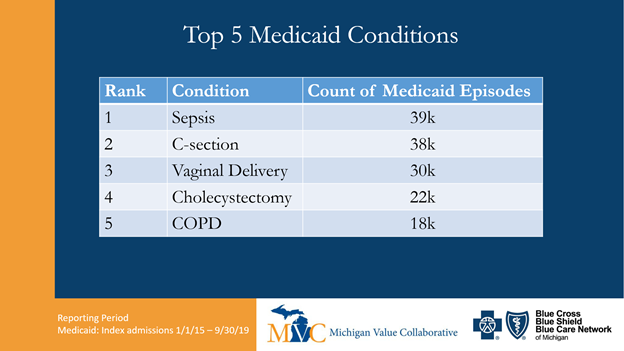
One developing strategy to convert big data sets into improved patient outcomes is the use of predictive analytics, an approach that differs from what many hospital quality improvement departments are currently utilizing. For example, the Michigan Value Collaborative (MVC) Coordinating Center has been helping hospitals identify opportunities for quality improvement since 2013 by aggregating and analyzing payor claims data and presenting the results on the registry and in analytics reports. The goal of these efforts is to help hospitals compare utilization against peers and draw important insights across a range of medical and surgical procedures. This retrospective approach helps MVC members to learn from their past performance in order to pursue meaningful, observable improvements within their buildings. It is one piece of the big data puzzle. Predictive analytics, on the other hand, allows clinicians to utilize big data before their patient experiences significant healthcare services or treatments. As its name denotes, this approach identifies prevention opportunities before the incidence of disease by predicting a patient’s risk. This is especially important for diseases that require early detection for optimal treatment and survival.
Unlike Robotic Process Automation (RPA), which is also on the rise in health systems across the country, predictive analytics is performed by Artificial Intelligence (AI). This means that computer systems will perform tasks typically requiring human intelligence, including analyses and decision-making. In some ways, this strategy mimics what physicians have long been doing at a patient’s bedside: collecting a patient’s medical history and risk factors in order to tailor their treatment and advice. This process is essential in evaluating a patient’s risk of developing chronic diseases, which often run in their family or are more likely due to socioeconomic factors. An article from the University of Illinois Chicago posits that predictive analytics represent a significant potential for cost savings if they help clinicians and their patients prevent the onset of chronic diseases, one of healthcare’s costliest areas.
“On a population-wide level, predictive analytics can help greatly cut costs by predicting which patients are at higher risk for disease and arrange early intervention, before problems develop,” the article stated. “This involves aggregating data that are related to a variety of factors. These include medical history, demographic or socioeconomic profile, and comorbidities.”
The Centers for Disease Control and Prevention (CDC) states that, “90% of the nation’s $3.8 trillion in annual health care expenditures are for people with chronic and mental health conditions.” So the potential cost savings from reducing chronic disease treatment are significant.
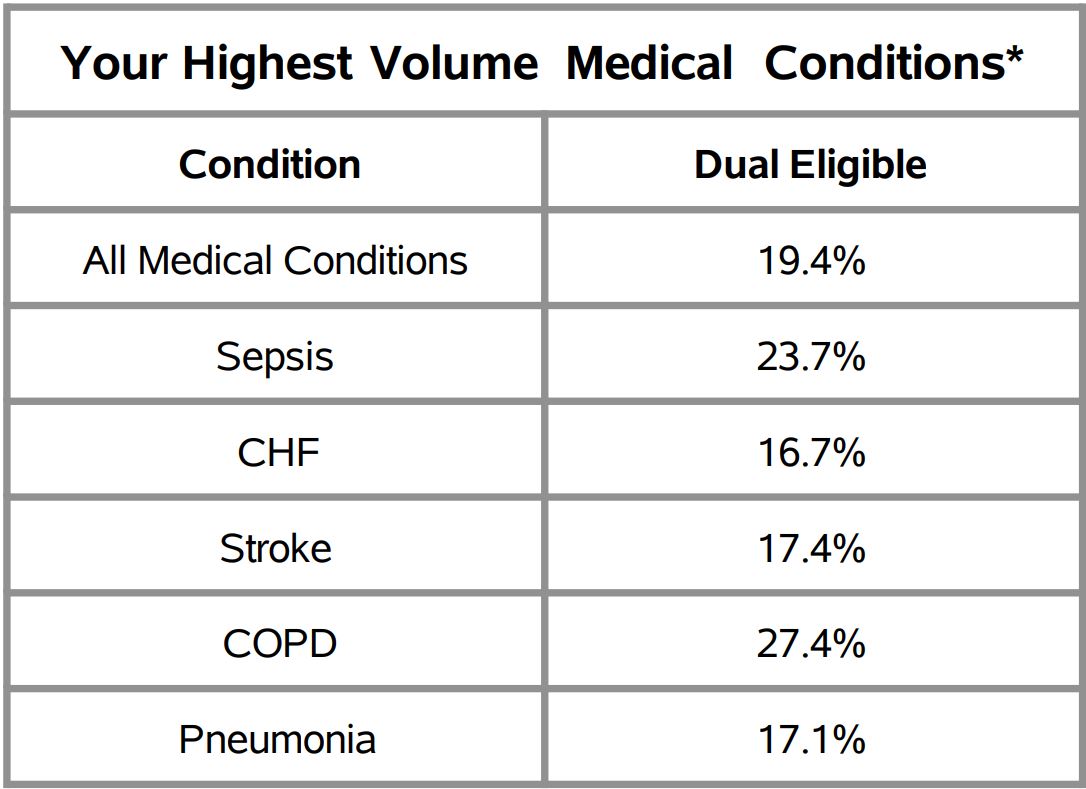
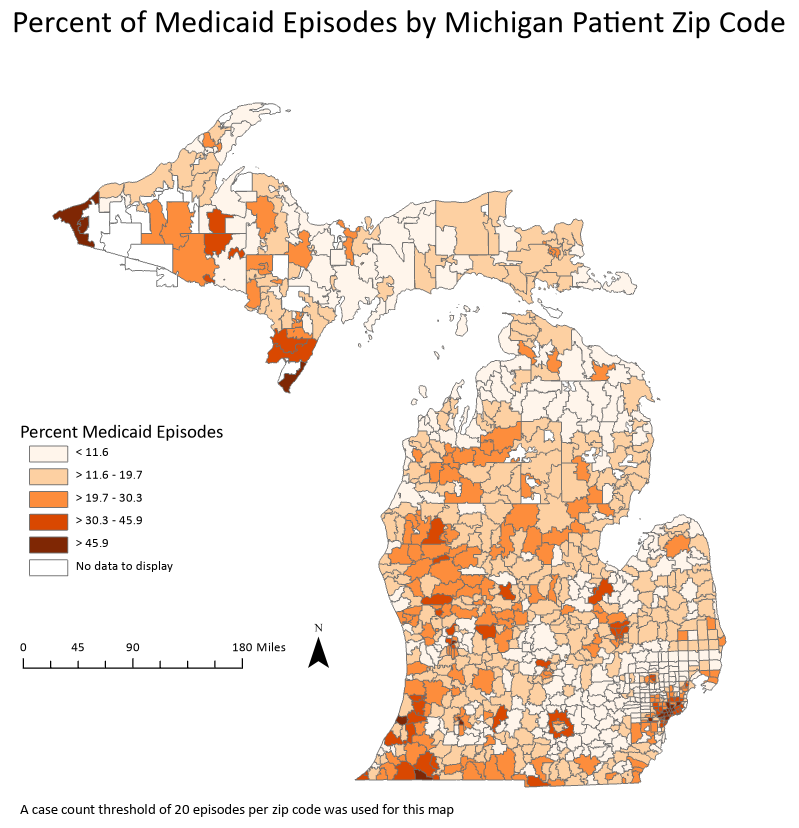
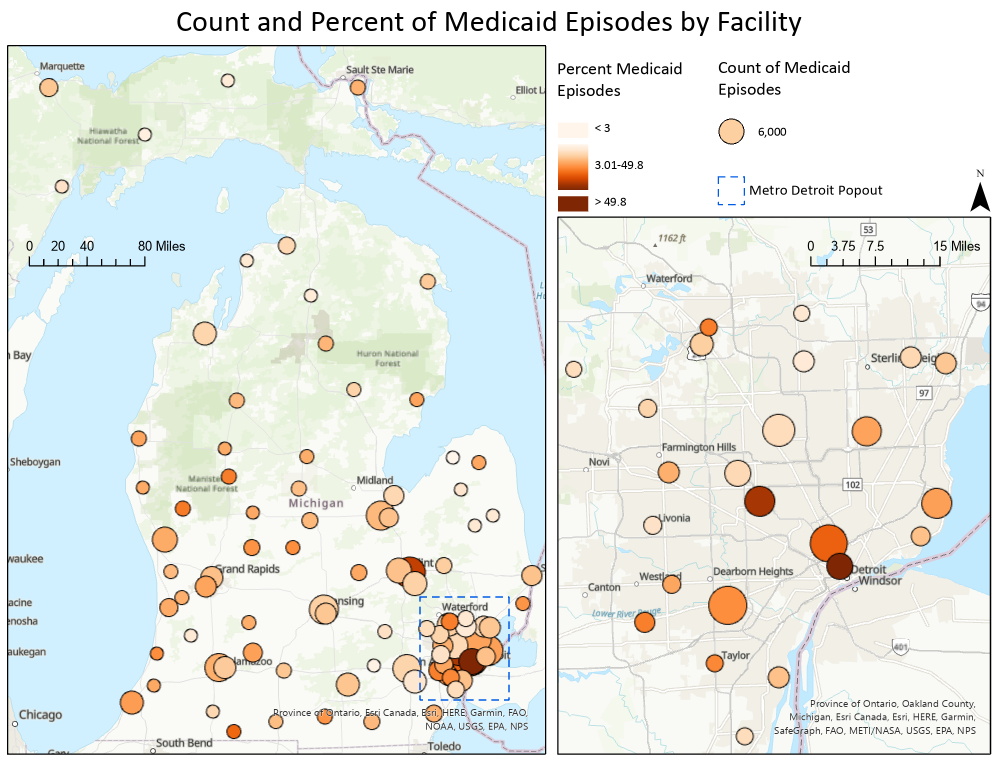
Using predictive analytics in a clinical setting can leverage both patient records and socioeconomic factors. Medical records will often include family history of chronic diseases such as cancer, diabetes, and heart disease, which would make a patient more likely to develop the condition themselves. In addition to family history, a patient’s socioeconomic factors (e.g., education, employment, and environment) and lifestyle choices are significant predictors of chronic disease. A study in the American Journal of Preventive Medicine outlines how researchers used predictive analytics to screen for cardiovascular disease risk from social determinants of health, and ultimately guide clinician treatment options. The researchers also suggest that large databases about social determinants of health variables, especially environmental ones, are not as readily available as they should be, and are an important area of opportunity for future data collection efforts.
A similar application of this technology was used in a study published by Cancer Immunology Research to predict lung cancer immunotherapy success. In the study, researchers used an AI algorithm to identify changes in patterns from CT scans that were previously not detected by clinicians, which ultimately predicted how well a patient would respond to immunotherapy. This suggests that predictive analytics can help improve the accuracy of diagnoses and treatment.
Of course, the applications for predictive analytics extend beyond chronic disease prevention and treatment. In the past year, researchers have also used predictive analytics to forecast outcomes for patients positive for COVID-19. In The American Journal of Emergency Department Medicine, a published study validated a tool that helps physicians predict adverse events among patients presenting with suspected COVID-19. The study suggests that the algorithm and scores can help physicians decide when to hospitalize or discharge patients during the pandemic. Therefore, predictive analytics appear to also provide insights that enhance treatment.
Many additional articles (such as one article from Health IT Analytics) and published studies recommend predictive analytics for its potential benefits. As with any technology, however, it is not without its risks. The use of AI brings about concerns for privacy, especially since hospitals must properly steward patient data and comply with HIPAA regulations. But there are several other considerations identified in a recent Deloitte analysis (see Figure 1), not the least of which is ensuring the algorithm doesn’t introduce bias that disproportionately harms minorities and communities of color. Predictive analytics may also present evaluation challenges. Once algorithms are validated, their widespread use in clinical settings should be confirmed for their efficacy, which requires measuring the absence of disease.