As we start the second half of 2022, the MVC Coordinating Center is taking a moment to pause and reflect on the tremendous work that has been accomplished over the past six months. Here is a look back at some of the highlights.
JANUARY
MVC Workgroups consist of a diverse group of representatives from Michigan hospitals and POs that meet virtually to collaborate and share ideas related to various topics. January kicked off with the launch of MVC’s new Health Equity Workgroup! The inaugural meeting featured speakers from the Michigan Social Health Interventions to Eliminate Disparities (MSHIELD) Collaborative. The Health Equity Workgroup has two more meetings in 2022 and we’d love to see you there! Visit the MVC 2022 Events Calendar to register and check the calendar for additional Workgroup offerings focused on Chronic Disease Management, Diabetes, Health in Action, Joint Replacement, and Sepsis.
FEBRUARY
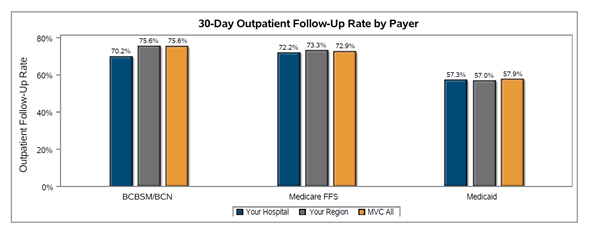
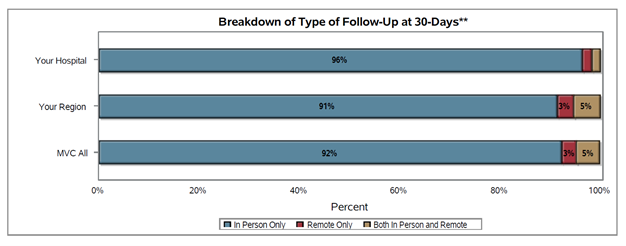
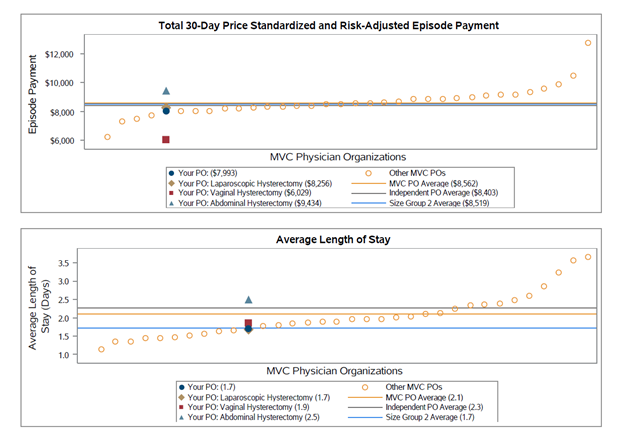
MVC launched two new push reports in February, with the release of the new Physician Organization (PO) Colectomy Report, shared with 35 of MVC’s PO members, and the first-ever Pneumonia Push Report, distributed to 89 MVC hospital members[1]. To meet the needs of MVC’s growing hospital members, a subset of the Pneumonia Push Reports was tailored to meet the specific data needs of our Critical Access Hospital members.
MARCH
After completing 58 hospital site visits in 2021, MVC announced the creation of a robust quality improvement (QI) initiatives database, developed to track QI initiatives across the collaborative. The database, searchable by QI focus area and project status, allows MVC to understand common themes and challenges among all its members as well as within subgroups such as hospital size or region. In 2022, the MVC team is hosting site visits with our PO members and will be gathering QI initiatives to add to the QI initiatives database. The database is being used as a resource for custom analytic requests and a library of practice standards for members. If you are an MVC PO interested in participating in a virtual site visit, please contact the MVC Coordinating Center to schedule.
APRIL
In April, MVC distributed a refreshed Sepsis Push Report, developed in collaboration with the Michigan Hospital Medicine Safety Consortium. These customized reports provide hospitals with new insight on demographics for their sepsis patients, including the percentage of COVID-positive patients to illustrate how COVID has impacted their sepsis data, along with race, top comorbidities, and most common zip codes, stratified by payer.
MAY
MVC held its first collaborative-wide meeting of 2022 in May, with a focus on “Turning Data into Action.” Held virtually, a total of 158 leaders representing 68 different hospitals and 15 physician organizations (POs) from across the state of Michigan participated in the event. Save the Date for our next in-person collaborative-wide meeting, scheduled for Friday, October 28th at the Radisson Hotel Lansing!
JUNE
In June, the MVC Coordinating Center hosted its first in-person event since 2019, with a Regional Networking Dinner for our Eastern Michigan sites (Region 3). The dinner provided an opportunity for MVC hospital and PO members to come together to network, share ideas and discuss key priorities, including health equity initiatives. MVC’s next Regional Networking Event for Southeast Michigan (Region 4) is scheduled for Tuesday, September 27th. For identification of your MVC designated region, please see the MVC Regions Map here.
AND COMING SOON…
Along the way, the MVC team has been hard at work preparing for two new exciting developments:
- MVC’s first Northern Summer Meeting (RSVP here) is scheduled for Thursday, August 18th at Traverse City’s Great Wolf Lodge. The agenda is tailored to highlight unique opportunities and challenges facing the Northern Michigan healthcare community. Interested MVC members serving Northern Michigan, the Upper Peninsula, and small/rural communities are encouraged to The University of Michigan Medical School designates this live activity for a maximum of 3.75 AMA PRA Category 1 Credit(s)™. This meeting will feature presentations from:
-
- Michigan Center for Rural Health
- MyMichigan Medical Center – Sault
- Munson Healthcare Grayling Hospital
- Region 9 Area Agency on Aging
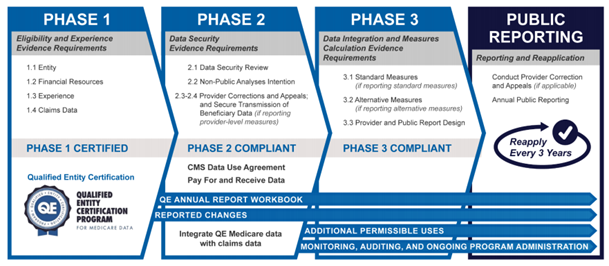
- MVC will soon launch the Qualified Entity section on MVC’s registry, which will provide hospital members with data access to some more granular patient-level Medicare data. Additional details coming soon!
To learn more about these initiatives and other MVC happenings, visit the MVC blog!
Footnote
[1] Hospitals and POs not meeting case count thresholds did not receive a report.