Every February while the nation honors American Heart Month, a subset of heart health advocates spend one week paying tribute to the lifesaving value of cardiac rehabilitation. Last week the Michigan Value Collaborative (MVC) Coordinating Center joined in on Cardiac Rehabilitation Week by helping to increase awareness and promote MVC’s efforts to improve utilization. Over the course of the week, MVC distributed press releases, published a daily cadence of social media content on Twitter and LinkedIn, and launched a video about the importance of cardiac rehab – all in service of inspiring collaboration in this area.
Cardiac rehabilitation (CR) has a Class IA indication for recent cardiac-related events or procedures, meaning there is high-quality evidence that it is beneficial to patients. In fact, individuals who complete the full program of 36 sessions have a 25% lower risk of death and a 30% lower risk of heart attack than those who attend only one session. It also reduces hospital readmissions and saves thousands of dollars per patient per year of life saved. Nevertheless, CR is widely underutilized, with national utilization rates of only 25-50%. It is for this reason that MVC wishes to equitably increase CR participation for all eligible individuals in Michigan. Throughout CR week, therefore, MVC endeavored to define the value of CR, what it entails, and how the actions of MVC members impact CR participation.
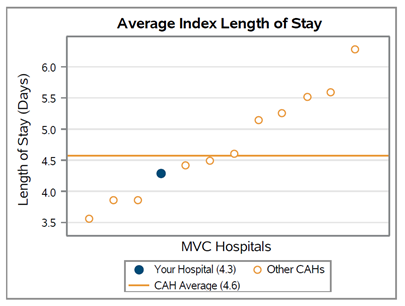
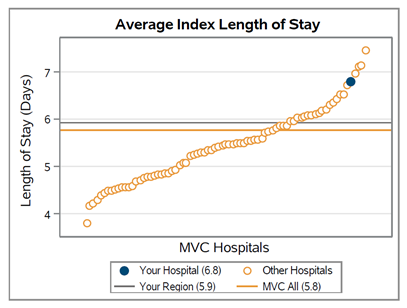
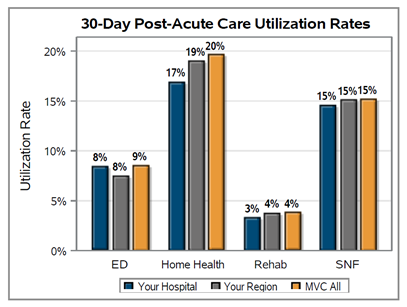
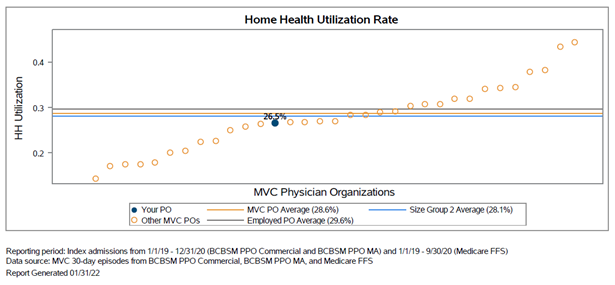
MVC’s role in the CR space is two-fold. One is the preparation of reports using its unique multi-payer data sources, and the second is providing opportunities for MVC members to collaborate. The reports that MVC prepares for members analyze claims data with time-specific hospital-level information on CR enrollment and completed visits within one year of discharge. This allows hospitals to benchmark their performance against peers and identify areas for improvement. There’s a huge amount of variation in CR rates across many dimensions – hospitals, qualifying events, and payers. For example, the hospital with the highest rate of CR after coronary artery bypass graft surgery (CABG) succeeds at sending 75% of their CABG patients to CR, while another only sends 28% of their CABG patients. This variation shows that it is possible to reach high CR rates, and hospitals can learn from each other to make systemic improvements that get more patients into this life-changing (and cost-saving) program.
To support collaboration among its member base of 100 hospitals and 40 physician organizations, MVC hosted a special, one-time workgroup on CR last week as part of its newly launched “Health in Action” workgroup series. This series is meant to drive discussion and collaboration on special topics that rotate throughout the year. Last week’s session featured the expertise of two special voices in the world of CR: Steven Keteyian, Ph.D., Director of Cardiac Rehabilitation/Preventive Cardiology at Henry Ford Medical Group, and Greg Merritt, Ph.D., patient advocate and founder of Patient is Partner. The workgroup was well attended with over 100 guests, who benefitted from informative and inspiring presentations from both speakers.
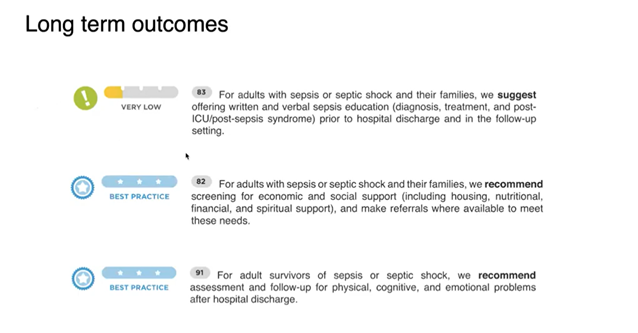
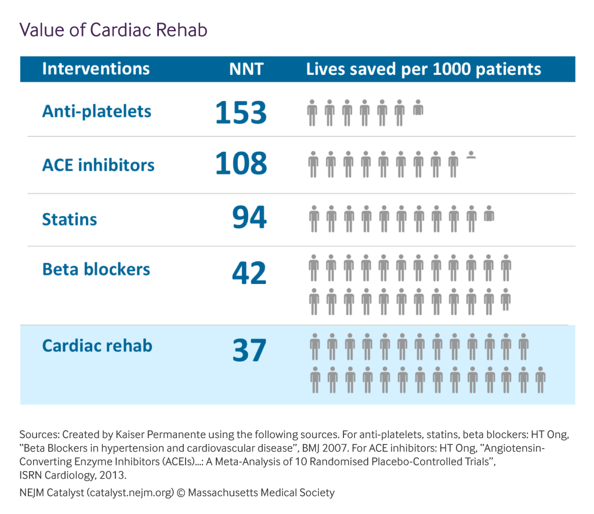
Dr. Keteyian presented updates on the clinical effectiveness of CR as well as some of the key barriers facing the field. There is high-quality evidence that CR is beneficial to patients on a variety of physiological measures, including improved exercise tolerance, decreased risk of future hospitalization, and decreased cardiovascular mortality. He also reiterated the value of cardiac rehab relative to other recommended cardiac interventions, with CR demonstrating more lives saved per 1000 patients than ACE inhibitors, statins, and other common medications (see Figure 1).
Figure 1. Calculating the Value of Cardiac Rehab
The current quality measures for CR suggest a patient’s time to enrollment should occur within 21 days of discharge, and that the patient should attend at least 36 sessions to receive the greatest benefit. The current goal for CR participation set by the Million Hearts initiative is 70%. However, Dr. Keteyian found that of the CR-eligible beneficiaries, only 28.6% participated and only 27.6% of those participants completed all 36 sessions. This represents a significant utilization gap. While discussing related challenges, Dr. Keteyian suggested that hospitals implement EMR-driven automatic referrals, overt provider endorsements, and an inpatient liaison to bridge the gap between referral and enrollment. He also recommended the use of hybrid CR programs that leverage telehealth to offer remote options.
Dr. Merritt’s presentation included his own personal story of surviving a cardiac event and his ensuing participation in a CR program. Following his experience, he became a “patient questionologist” dedicated to finding opportunities for patient and provider collaboration. His story ultimately led to the founding of an organization called Patient is Partner, which is dedicated to the principles of patient-partnered care. Inspired by the writings of behavioral scientists as well as Why We Revolt by Victor Montori, Dr. Merritt outlined a vision for healthcare innovation that invites patients and their unique perspectives to help solve healthcare’s greatest challenges. He encouraged attendees to join the movement and invite more patient voices to contribute to their respective committees and teams.
At the conclusion of the week, the MVC team had helped its audiences connect to educational materials, data, specialists, former patients, and successful peers in this space. The Coordinating Center is eager to continue this momentum from CR Week in pursuit of a variety of goals for 2022 and beyond. If your hospital or physician organization is interested in improving CR utilization rates, you can learn more about how MVC supports members to increase CR enrollment or reach out directly at michiganvaluecollaborative@gmail.com. You can also view a recording of the full CR workgroup here.