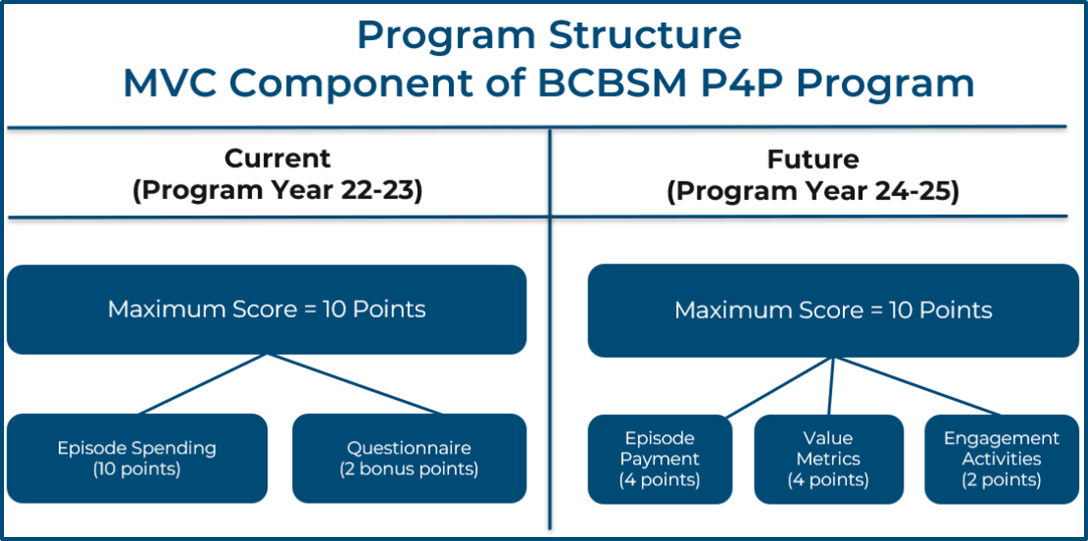
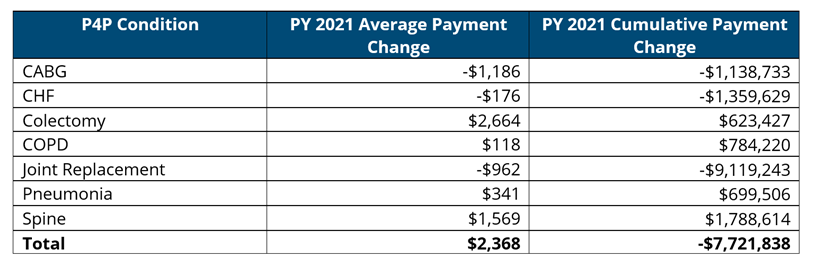
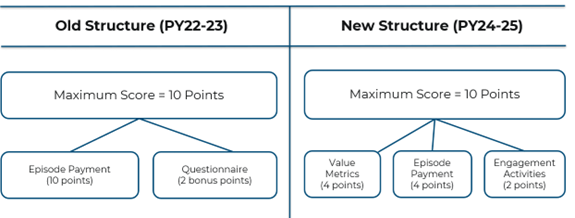
Beginning in 2018, Blue Cross Blue Shield of Michigan (BCBSM) allocated 10% of its Pay-For-Performance (P4P) Program to a metric based on Michigan Value Collaborative (MVC) claims data. In 2022, the BCBSM P4P Quarterly Workgroup approved changes to how hospitals are evaluated in future program cycles. The upcoming two-year cycle including Program Years (PYs) 2024 and 2025 will be the first impacted by these changes, with performance years in 2023 and 2024, respectively (see Figure 1). Hospitals received selection reports for the next cycle this week to aid in their decision-making on metrics within the new program structure.
Figure 1.

What is staying the same?
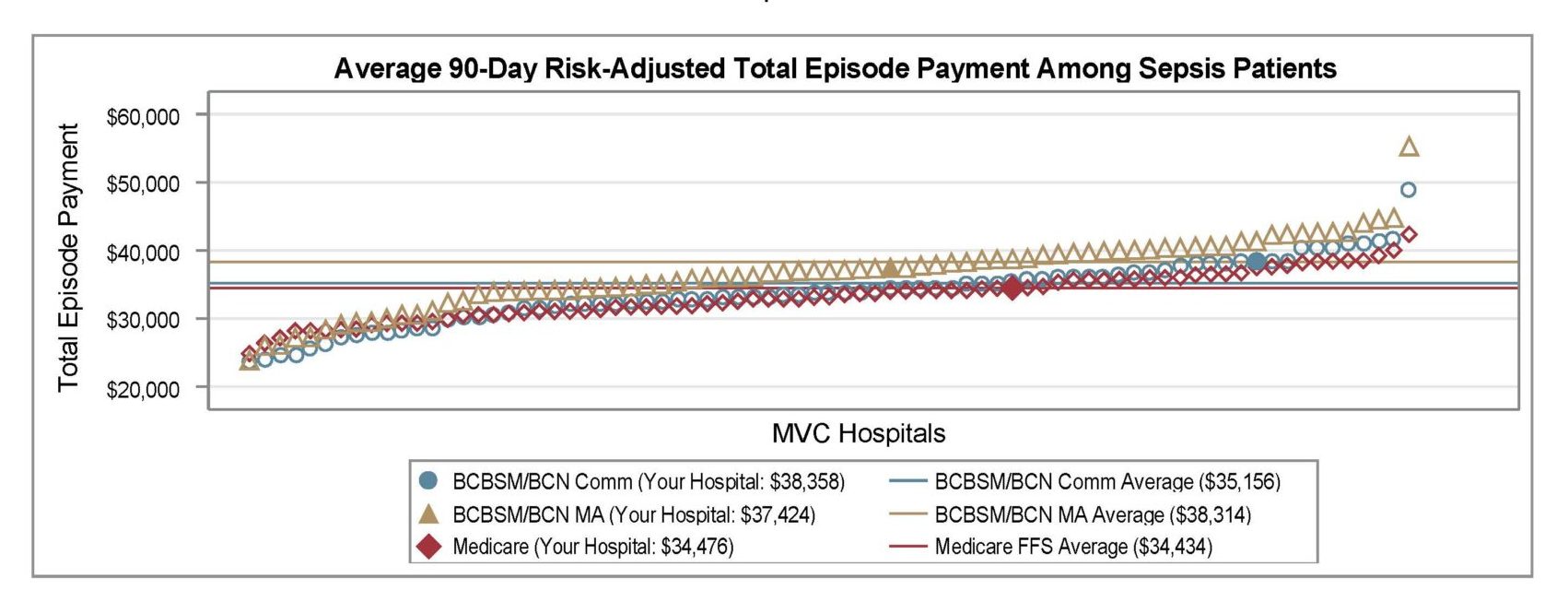
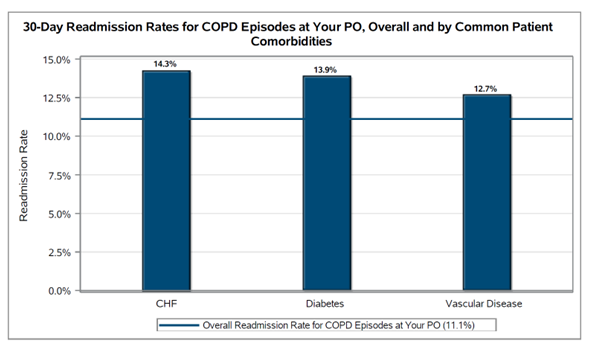
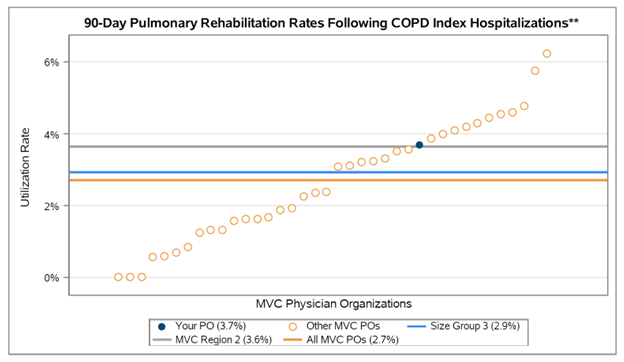
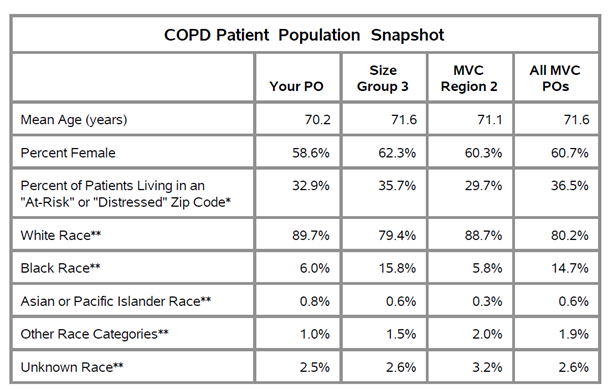
The program will continue to be scored out of 10 points maximum, and hospitals will continue to be evaluated on their risk-adjusted, price-standardized total episode payment, though this will make up a smaller component of the overall program. In addition, most conditions hospitals could select previously for episode payment scoring will still be available for that component of the program. Those include chronic obstructive pulmonary disease (COPD), colectomy (non-cancer), congestive heart failure (CHF), coronary artery bypass grafting (CABG), joint replacement, and pneumonia. Additionally, a hospital’s metric selections will continue to be scored on improvement compared to the hospital’s own past performance and scored on achievement related to an MVC cohort. Each hospital will continue to be awarded the greater of the two scores, either improvement or achievement, which are calculated using Z-scores. Cohort designation is still based on bed size, critical access status, and case mix index.
What is changing?
The PY 2022-2023 program was scored out of 10 points, but 12 points could be earned (10 points from episode spending plus two bonus points). In PYs 2024-2025, the overall program structure (Figure 2) will change so that the maximum score will be 10 points, made up of a maximum of four points from an episode spending metric, a maximum of four points from a value metric (a new component), and a maximum of two points from engagement activities completed in the program year (the calendar year following the performance year). This means that rather than selecting two conditions as in previous program cycles, hospitals will now select one condition for the episode spending metric and select one value metric. In order to be eligible to select a payment condition or value metric, a hospital must be projected to have at least 20 cases in the full baseline year of 2021. No bonus points will be available for PYs 2024-2025.
Figure 2.
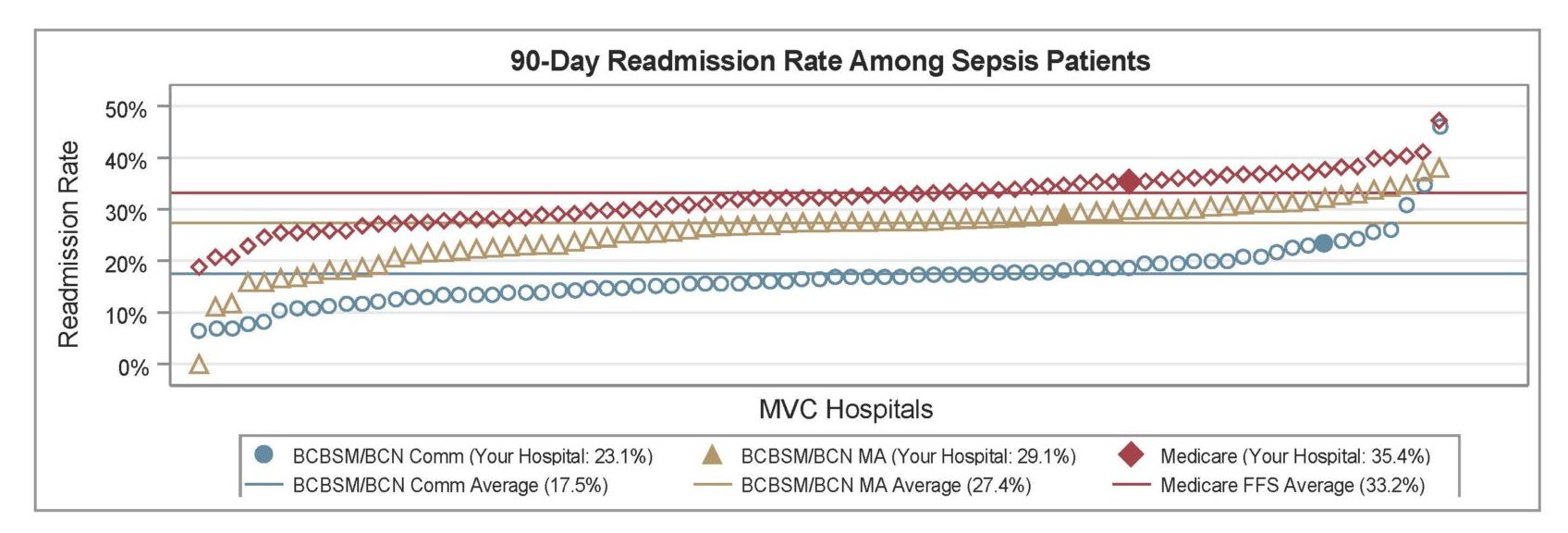
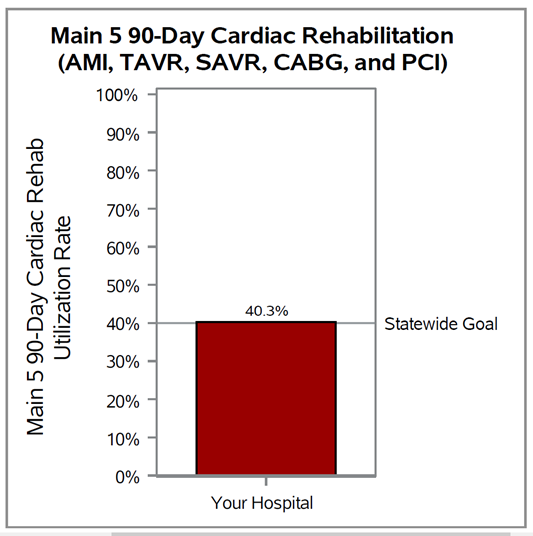
Brand new in PYs 2024-2025 will be value metrics, which are evidence-based, actionable measures that show variability across the state. Hospitals will be rewarded for high rates of high-value services or low rates of low-value services. Seven value metrics are available for hospitals to choose from: cardiac rehabilitation after CABG, cardiac rehabilitation after percutaneous coronary intervention (PCI), seven-day follow-up after CHF, 14-day follow-up after COPD, seven-day follow-up after pneumonia, preoperative testing, and risk-adjusted readmission after sepsis. The preoperative testing value metric is composed of a group of three low-risk procedures: cholecystectomy, hernia repair, and lumpectomy. Each procedure will be scored separately, and points for this value metric will be awarded based on the highest points achieved for a hospital’s eligible procedures.
Finally, engagement in MVC activities will be built into the program’s scoring structure, rather than being offered as “bonus” points. Hospitals will be eligible to earn up to two points by attending and participating in MVC activities throughout each program year. These points are intended to increase engagement with other hospitals and the MVC Coordinating Center. Hospitals may select their own combination of activities but must include at least one activity from each of the attendance and participation categories to earn any points.
The P4P selection reports distributed this week include tables for the various episode spending and value metrics that identify projected case counts, the hospital’s average payment or rate of utilization, the cohort and MVC All average payments or rates, and the projected changes necessary for the hospital to earn 1 – 4 points. Accompanying the reports was an interpretation guide to walk recipients through a blinded sample report. It includes guidance on how to interpret the tables with suggestions for how this data could be used to inform a hospital’s P4P selections. The guide can be viewed here.
A complete summary of changes to PYs 2024 and 2025 is available here. These changes will not be retroactively applied to PYs 2022-2023. For complete details about PYs 2024-2025, please refer to the P4P Technical Document. Contact the MVC Coordinating Center with any questions. MVC requests that member hospitals complete and submit their PY 2024-2025 selections by December 23, 2022.