In the final months of 2022, the MVC team distributed metric selection reports for Program Years 2024 and 2025 of the MVC Component of the Blue Cross Blue Shield of Michigan (BCBSM) Pay-for-Performance (P4P) Program. These reports were provided in conjunction with details pertaining to the selection process as well as changes to the program structure, scoring methodology, and cohort assignments for the upcoming two-year cycle.
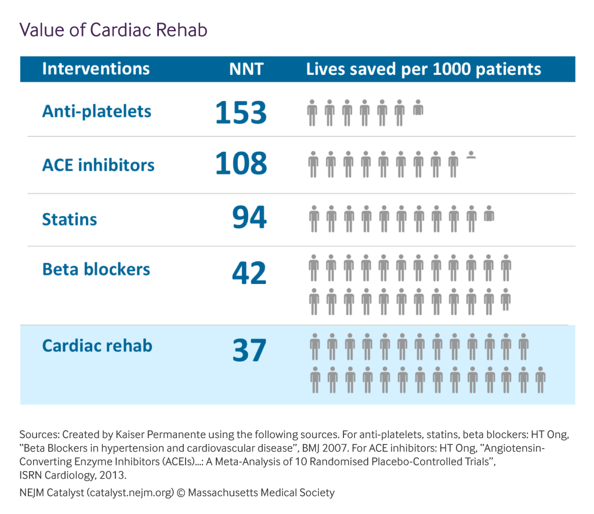
Eligible hospital members were tasked with reviewing these reports and returning their selections in recent months. MVC has now received metric selections for PYs 2024 and 2025. This program cycle will award a maximum score of 10 points, made up of a maximum of four points from an episode spending metric, a maximum of four points from a value metric (a new component), and a maximum of two points from engagement activities completed in the program year (the calendar year following the performance year). Each participating hospital selected one of the six available conditions for the 30-day episode payment component: chronic obstructive pulmonary disease (COPD), colectomy (non-cancer), congestive heart failure (CHF), coronary artery bypass graft (CABG), joint replacement, and pneumonia. The episode spending metric that the most hospitals selected was joint replacement (32), followed by CHF (20). No sites selected colectomy. See Figure 1 for a depiction of the total selections for each condition.
Figure 1.
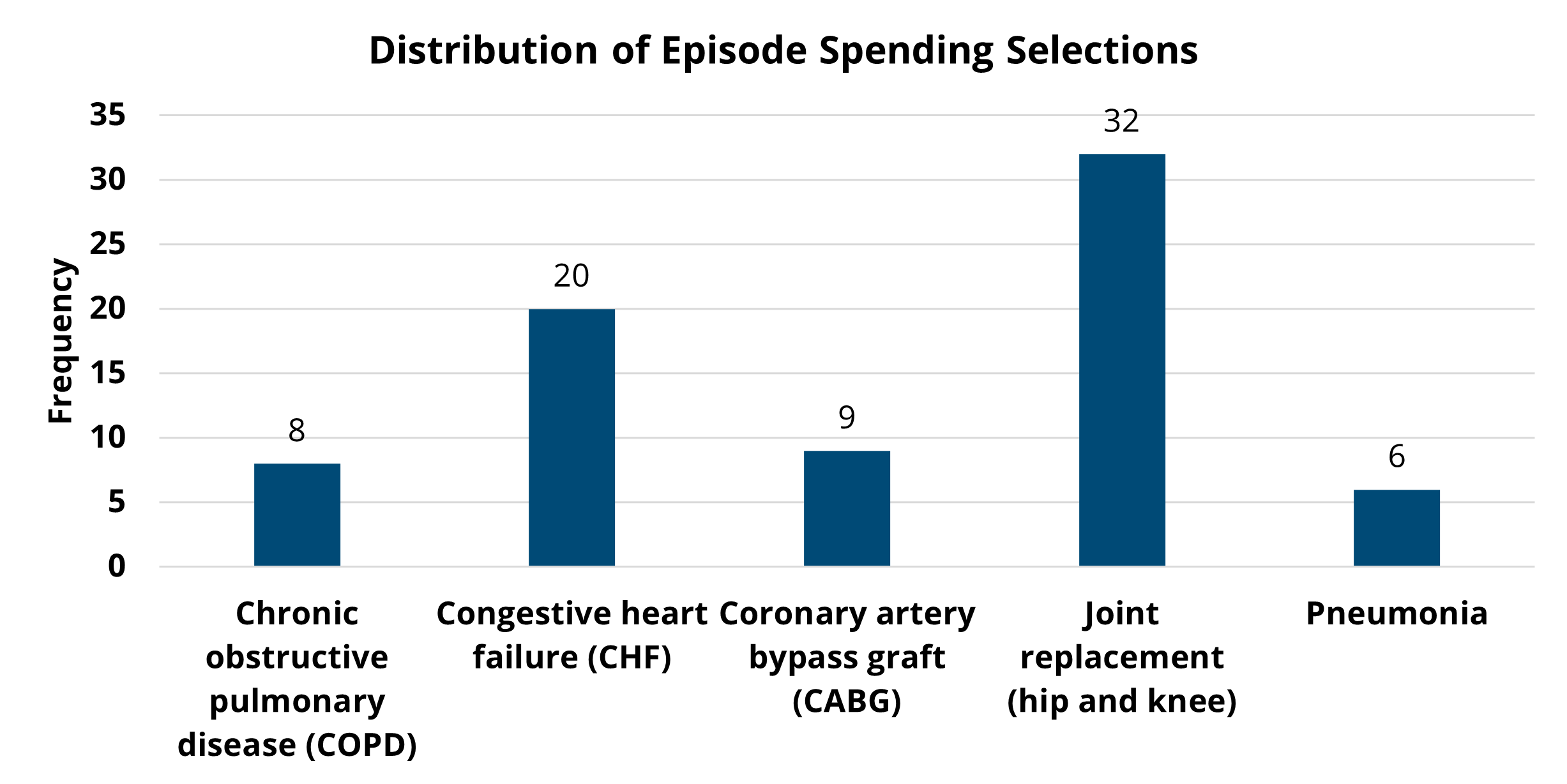
The distribution in episode spending selections was consistent when stratified by MVC region of Michigan; joint replacement was the top choice within all four MVC regions, and CHF was generally the next most common. However, Region 1 (which constitutes Northern Michigan) had a smaller percentage of sites select CHF, with a slight preference for pneumonia. In addition, hospitals located in Region 4 (southeast Michigan) were more likely to select COPD (Figure 2).
Figure 2.
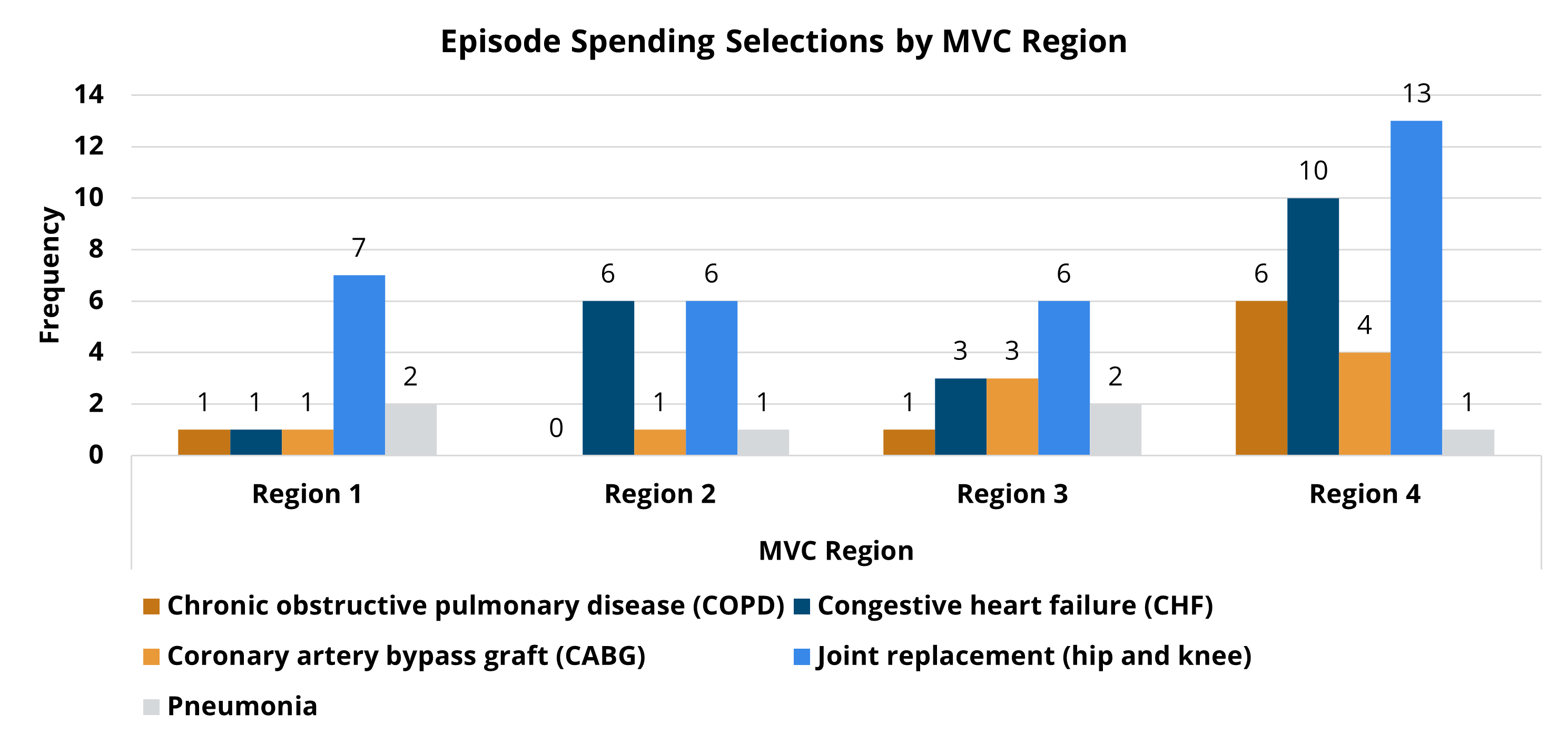
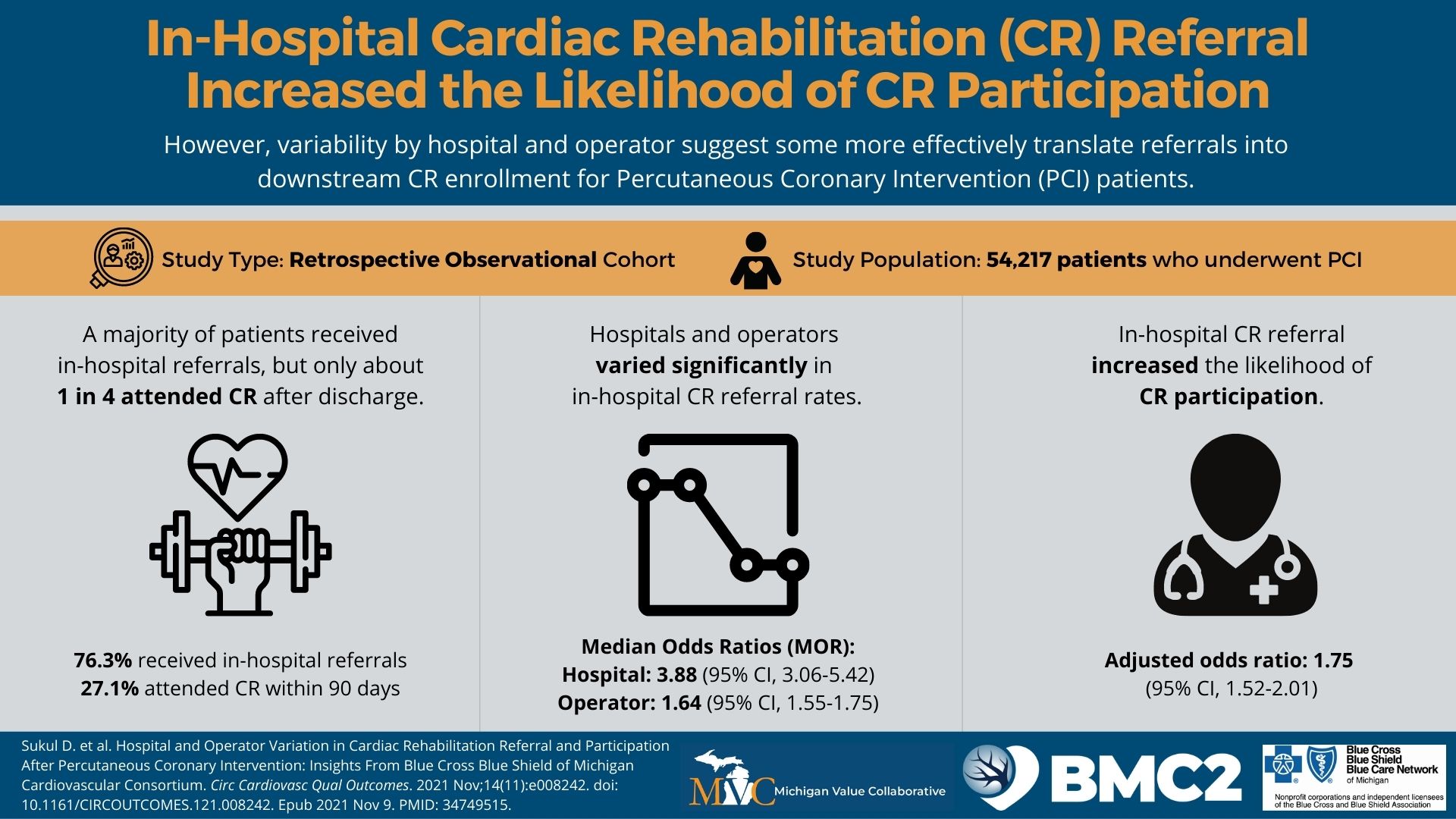
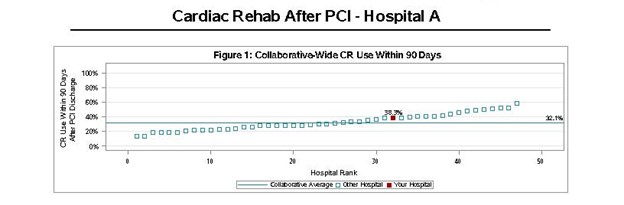
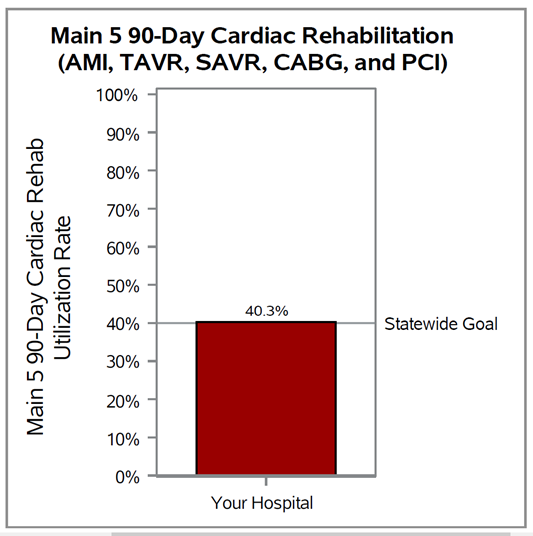
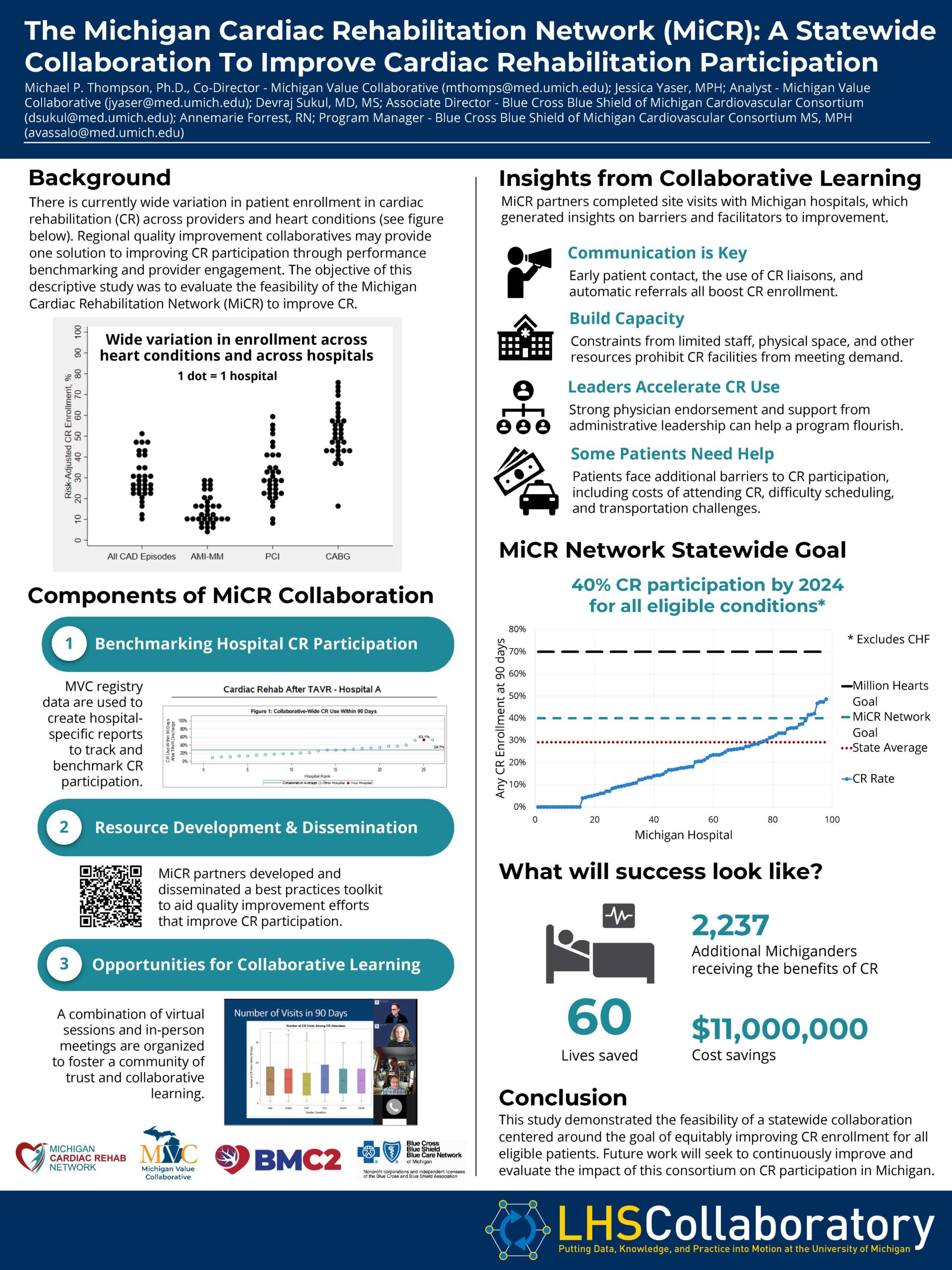
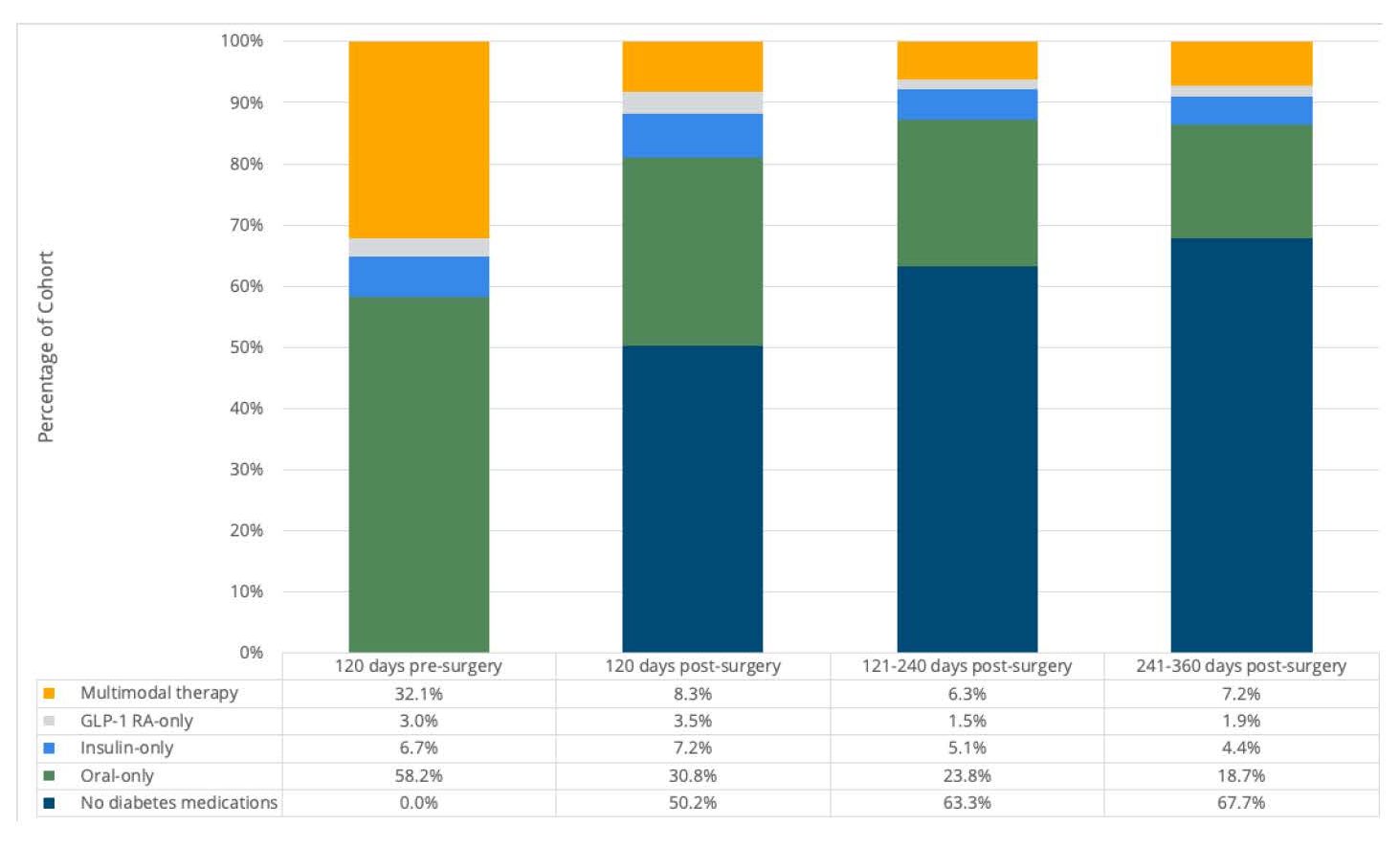
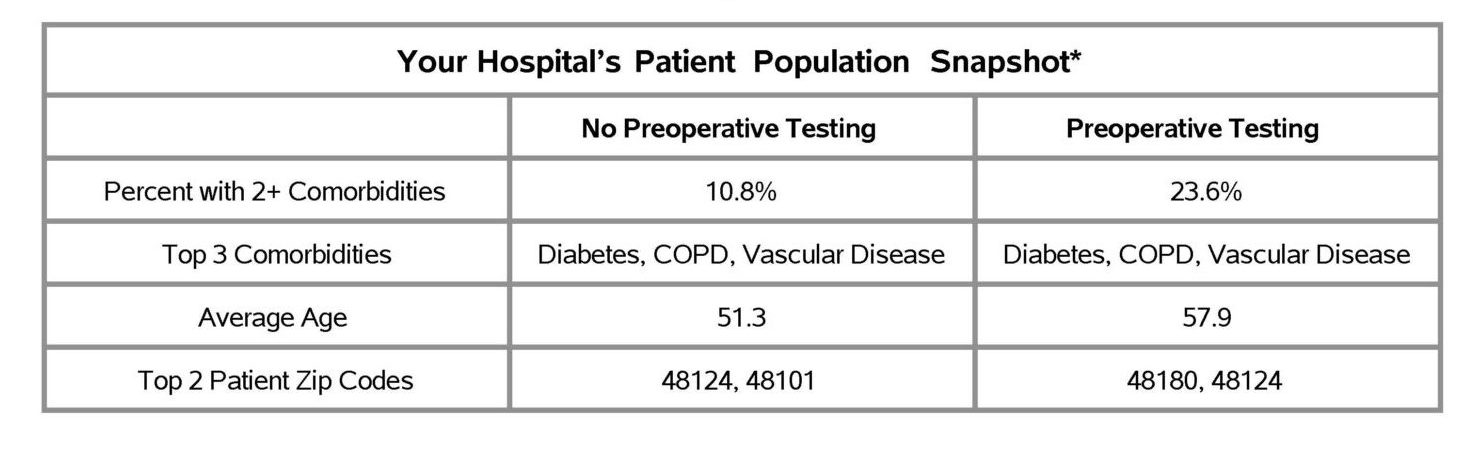
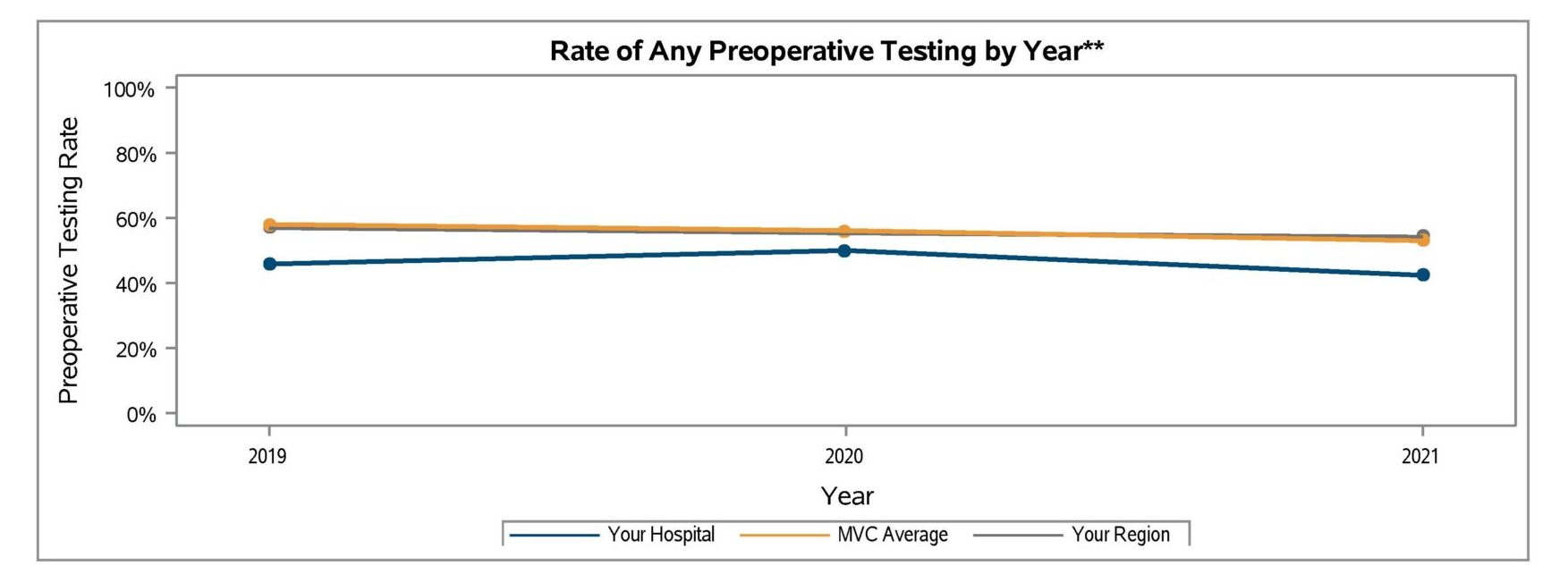
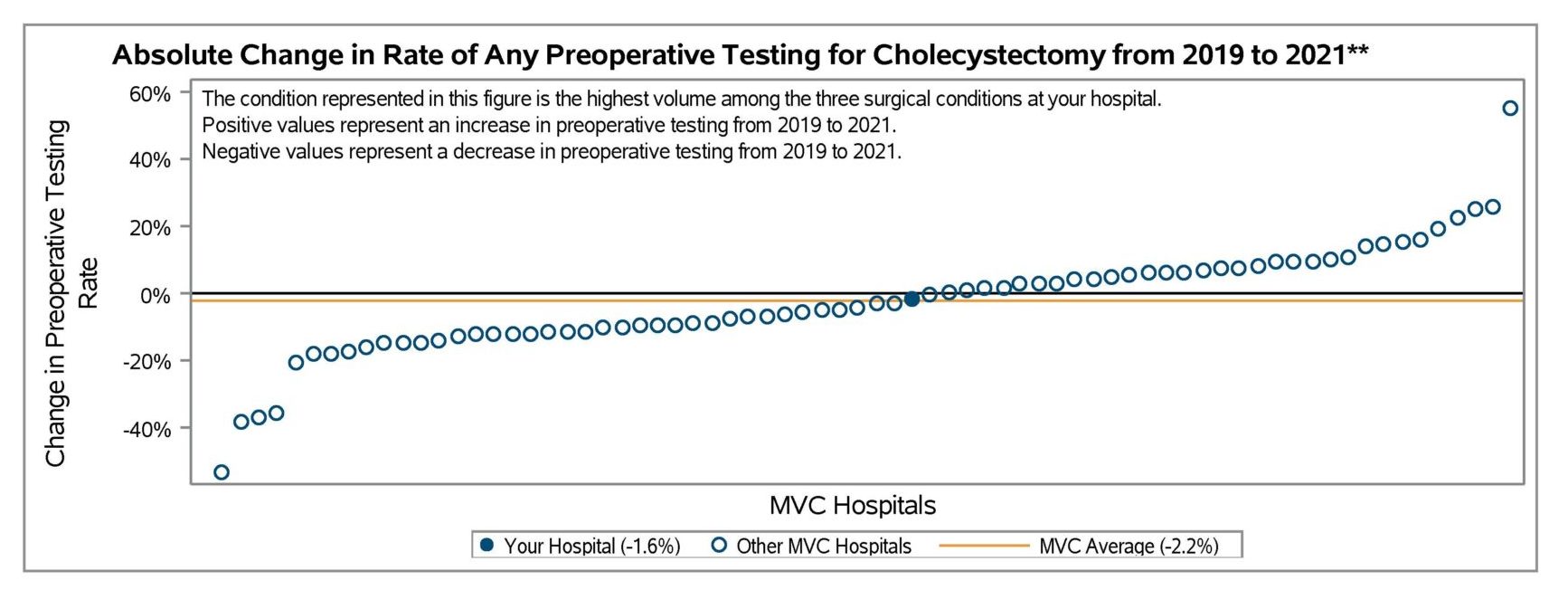
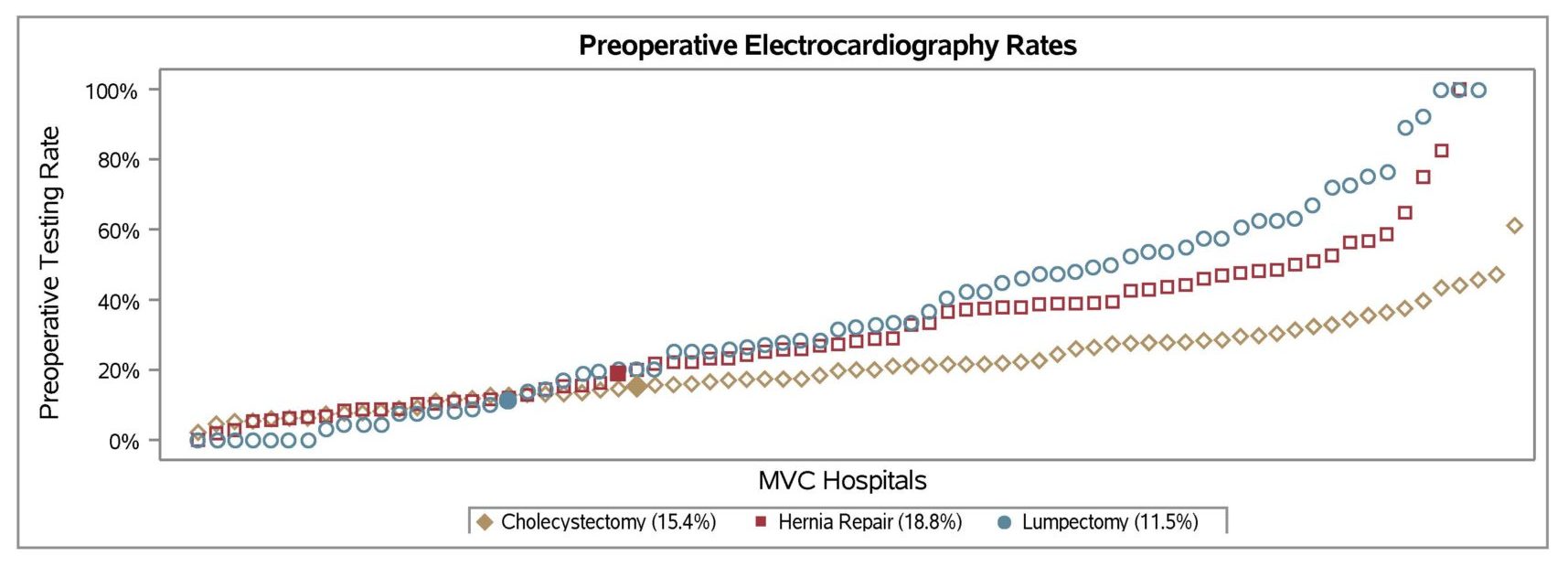
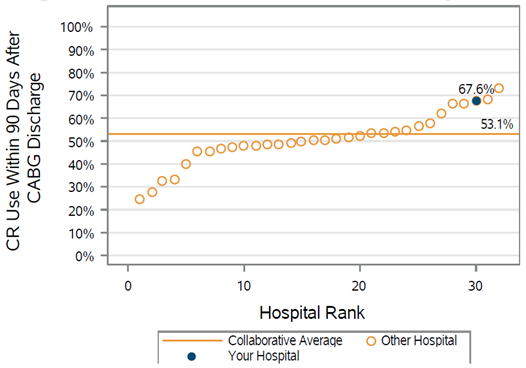
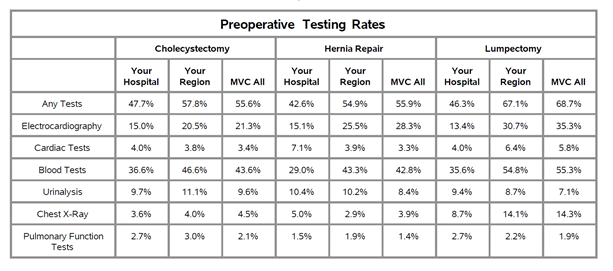
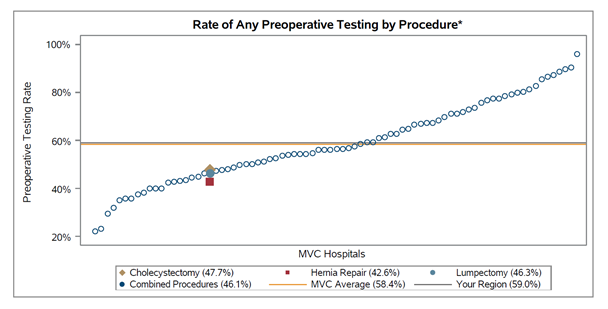
Brand new in PYs 2024-2025 will be value metrics, which are evidence-based, actionable measures with variability across the state. Hospitals will be rewarded for high rates of high-value services or low rates of low-value services. Seven value metrics were available for hospitals to choose from: cardiac rehabilitation after CABG, cardiac rehabilitation after percutaneous coronary intervention (PCI), seven-day follow-up after CHF, 14-day follow-up after COPD, seven-day follow-up after pneumonia, preoperative testing, and risk-adjusted readmission after sepsis. The preoperative testing value metric is composed of a group of three low-risk procedures: cholecystectomy, hernia repair, and lumpectomy. Each preoperative testing procedure will be scored separately, and points for that value metric will be awarded based on the highest points achieved for a hospital’s eligible procedures.
In its first year offering a value metric, MVC found that seven-day follow-up after CHF was selected by the most participants (25). Metrics related to cardiac rehabilitation participation accounted for 23 selections; 17 sites selected cardiac rehabilitation after PCI and five selected cardiac rehabilitation after CABG (Figure 3).
Figure 3.
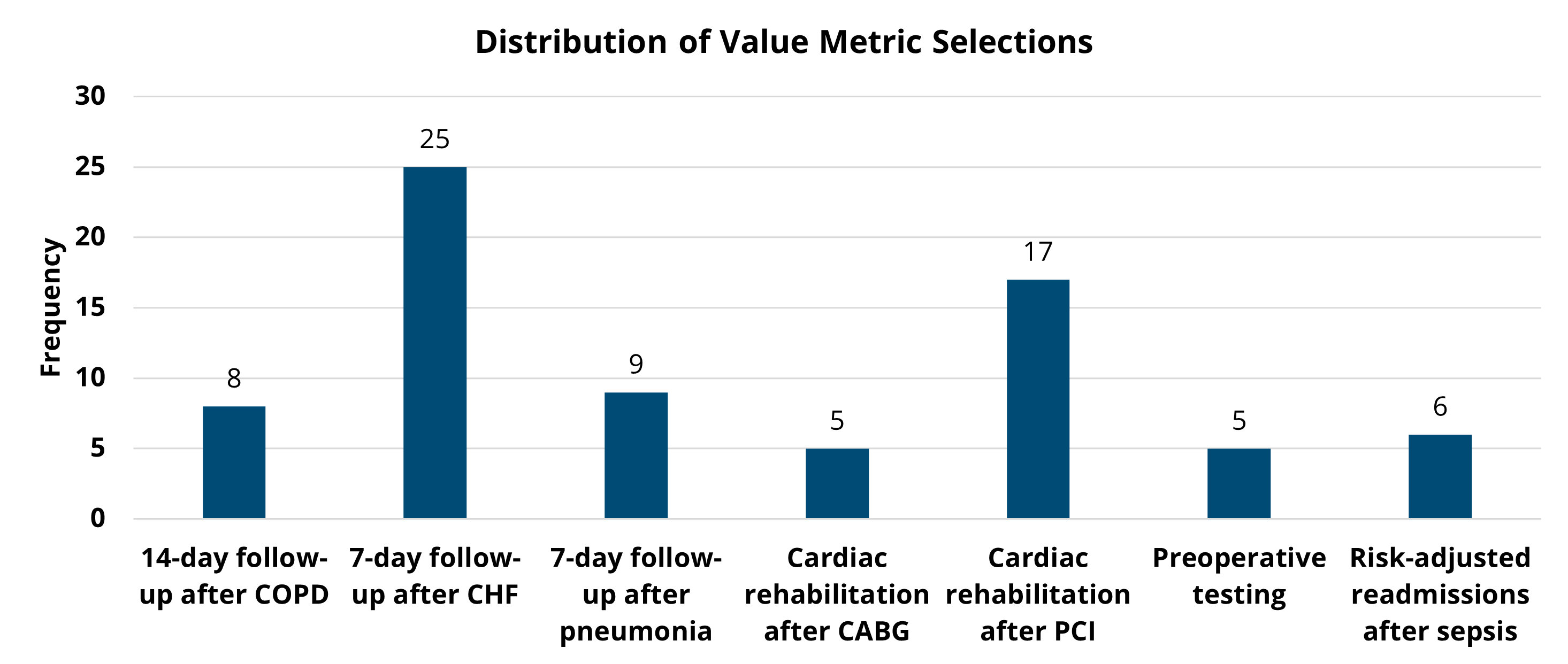
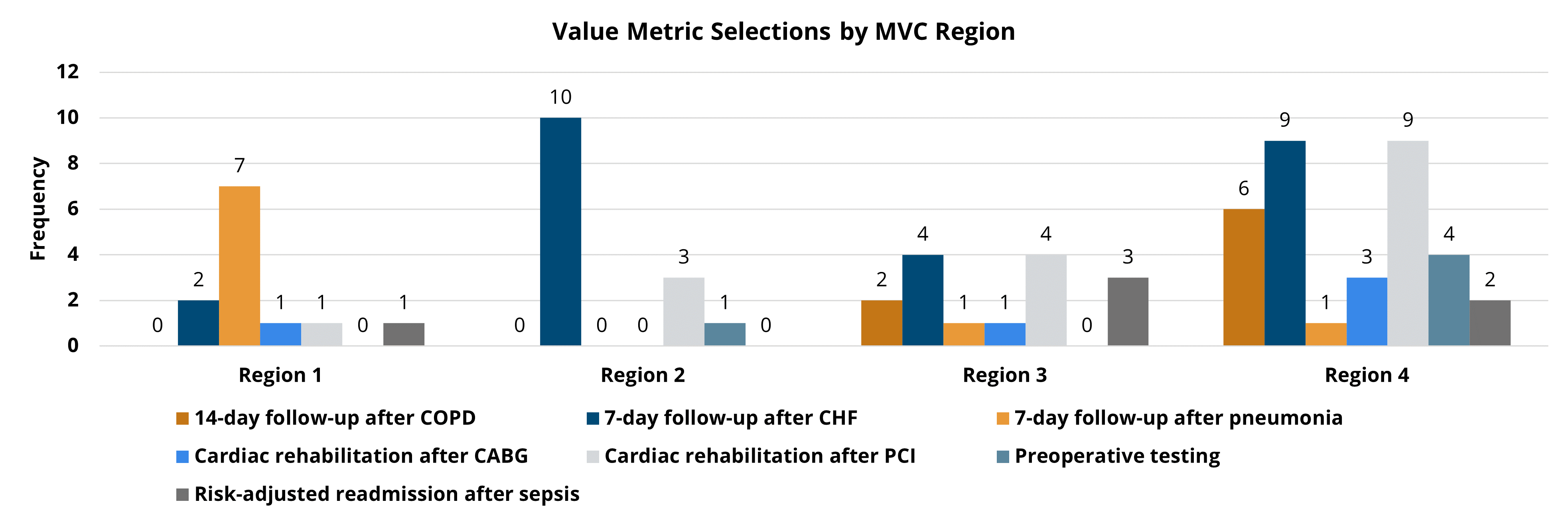
There was more variation by MVC region for value metric selections than for episode spending selections (Figure 4). In Region 1 (Northern Michigan), seven-day follow-up after pneumonia was the most common selection. Nearly all the sites located in Region 2 (west Michigan) selected seven-day follow-up after CHF—this metric accounted for 71% of selections in this part of the state. Region 3 (mid-Michigan and the thumb region) had more sites select risk-adjusted readmission after sepsis, but Region 3 had a more even distribution of selections across the available metrics than Regions 1 or 2. Finally, Region 4 (southeast Michigan) had selections for all the available value metrics. Region 4 also had the most interest in 14-day follow-up after COPD.
Figure 4.
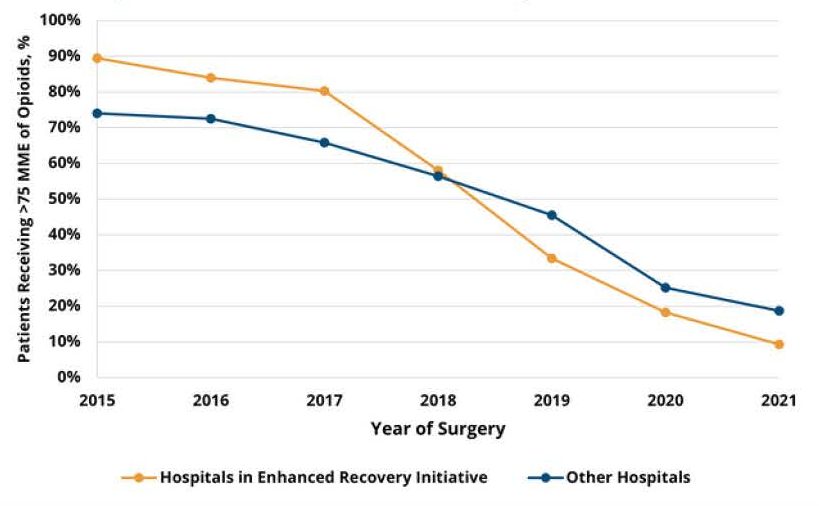
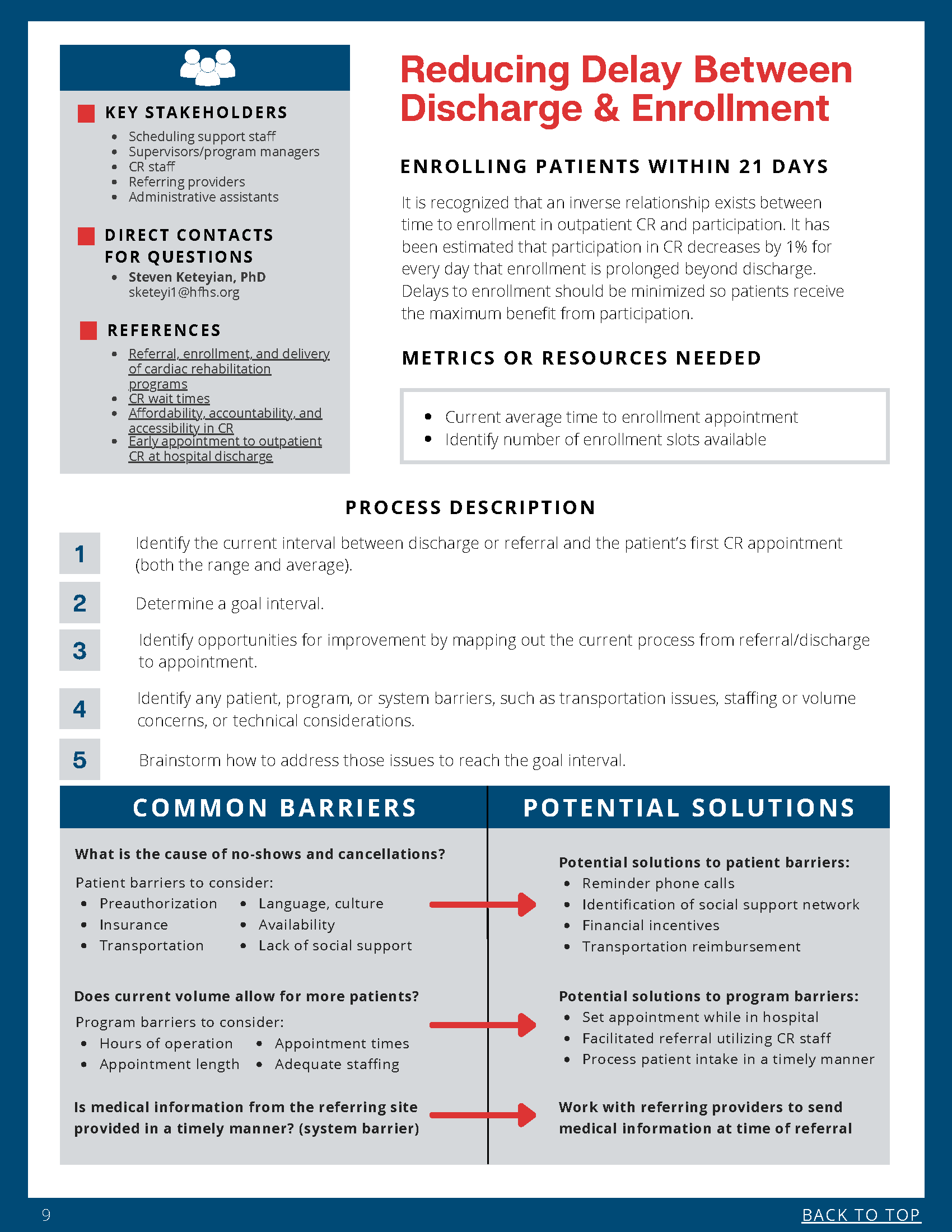
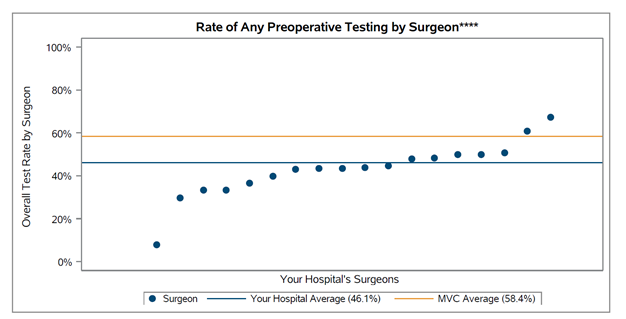
Two of MVC’s new value metrics align with existing value campaigns for which MVC is offering additional support. MVC established campaigns for both cardiac rehabilitation and preoperative testing in October 2020. Since then, MVC has developed reports on these two areas of healthcare utilization, which have historically been shared biannually. In addition, beginning in 2023, MVC is offering workgroups tailored to these value metrics. MVC’s first cardiac rehabilitation workgroup of 2023 took place on Feb. 16 during cardiac rehabilitation week featuring guest presentations by Haley Stolp of Million Hearts and Mike Thompson, PhD, MPH, Co-Director of MVC and Co-Director of the Michigan Cardiac Rehabilitation Network. A full recording of this session is available here. MVC’s first preoperative testing workgroup of 2023 will take place next week on Wed., March 15, from 1-2 p.m., featuring MVC Director Hari Nathan, MD, PhD. Those interested in learning about ready-to-use tools and strategies for the de-implementation of low-value testing may register here. Attending hospital sites will be encouraged to share their experience thus far with quality improvement related to preoperative testing, such as resources in use or in development and common barriers to change.
P4P cohorts were reassigned for PYs 2024 and 2025. Those cohort assignments and the new technical document have been published on the MVC website’s P4P page. The cohorts were not intended to group hospitals that are exactly alike; rather, they create a reasonably comparable grouping from which MVC can complete statistical analyses.
MVC’s P4P measure began in 2018 when BCBSM allocated 10% of its P4P program to an episode of care spending metric based on MVC data. If you would like to receive notices about the MVC workgroups or have questions about any aspect of the MVC Component of the BCBSM P4P Program, please contact the MVC Coordinating Center at Michigan-Value-Collaborative@med.umich.edu.