Last month the Michigan Value Collaborative (MVC) distributed mid-year scorecards for Program Year (PY) 2025 of the MVC Component of the Blue Cross Blue Shield of Michigan (BCBSM) Pay-for-Performance (P4P) Program. This report provided hospitals with their current standing for PY 2025. It also included a preview of measure scoring for the new health outcome variation measure that will be worth one point in PYs 2026-2027.
Each hospital received a mid-year score out of a total of 10 points, including 0 to 4 points for their selected total episode payment metric, 0 to 4 points for their selected value metric, and 0 to 2 points for completed eligible engagement activities. PY 2025 scores achievement and improvement points for each hospital’s selected episode spending conditions and value metrics using index admissions from 2024 performance year data against admissions in 2022 as the baseline year. Hospitals are awarded the higher of their achievement and improvement point scores.
The performance data timeframes included in mid-year PY 2025 scoring were index events 1/1/2024 – 12/31/2024 for BCBSM PPO Commercial, BCBSM Medicare Advantage (MA), BCN HMO Commercial, BCN HMO MA, and index events from 1/1/2024 – 6/30/2024 for Medicare FFS. The engagement points accrued represent all completed activities from 1/1/2025 – 7/31/2025. All scores are subject to change in the final scorecards as the remaining 2024 performance data becomes available and additional 2025 P4P engagement activities are completed and recorded for this year.
Figure 1 illustrates the current distribution of total points out of 10 across the collaborative. The average points scored across the mid-year scorecards was 6.3 out of 10. This average is 0.3 points lower than the average points scored at the conclusion of PY 2024.
Figure 1.
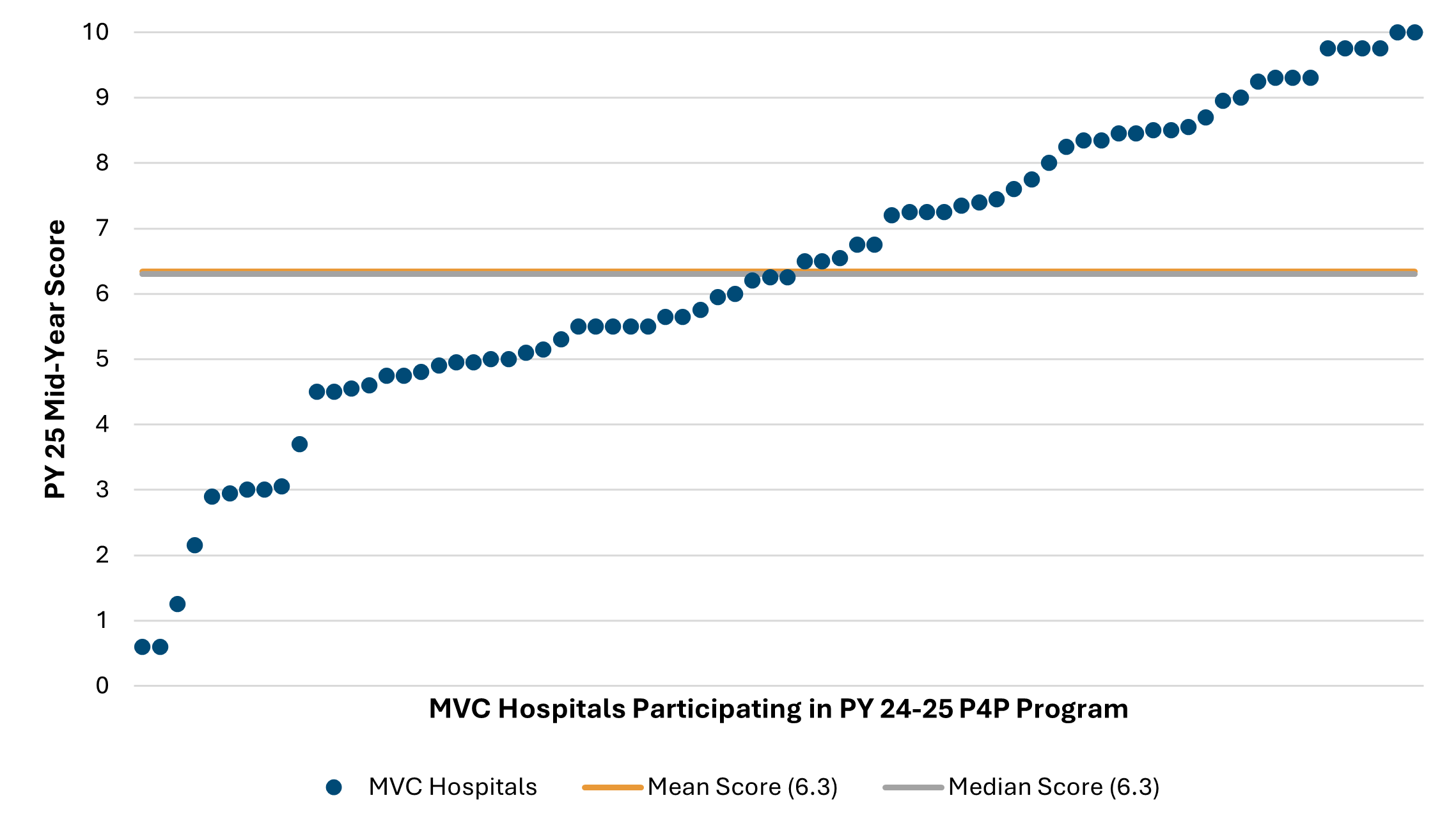
Figure 2 illustrates the breakdown of scoring on average by each program component (i.e., episode spending metric, value metric, engagement points). Hospitals could earn up to four points for their episode spending and value metric selections, and up to two points for engagement activities completed in 2025. Across the collaborative, the average points scored for both episode spending and value metrics was 2.6 points, and 1.2 points for engagement activities.
Figure 2.
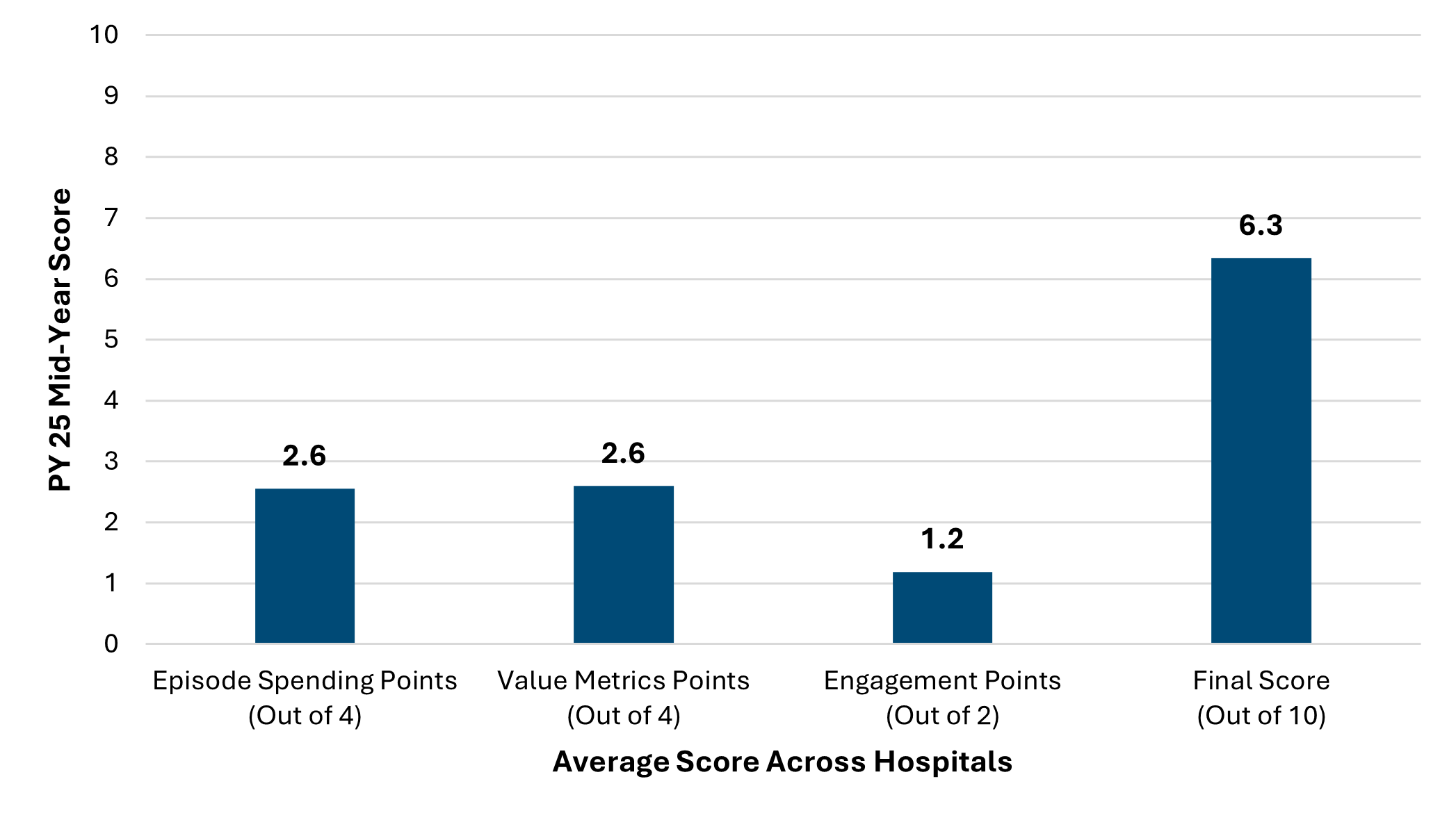
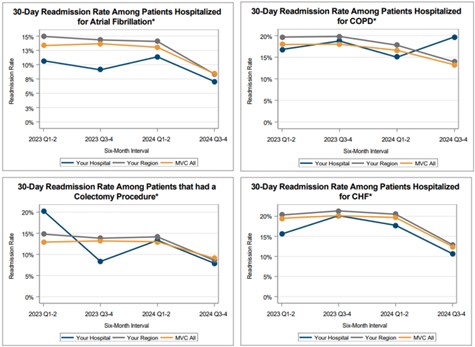
Figure 3 illustrates the breakdown of the average points by episode spending conditions. Coronary Artery Bypass Grafting (CABG) was the highest scoring episode spending condition with an average of 3 points, and this was closely followed by joint replacement with 2.7 points. The lowest scoring episode spending condition was pneumonia with hospitals earning less than 2 points on average.
Figure 3.
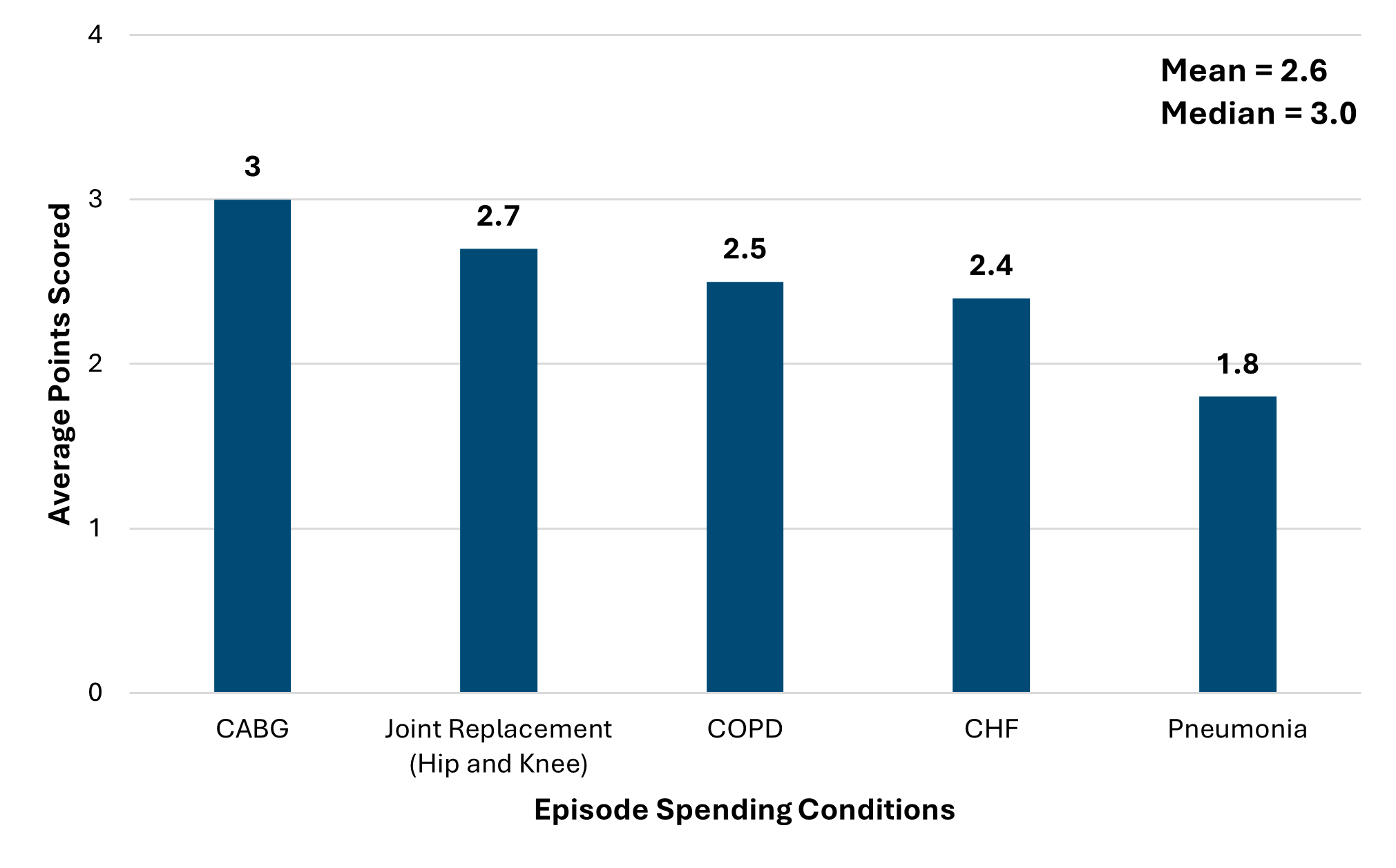
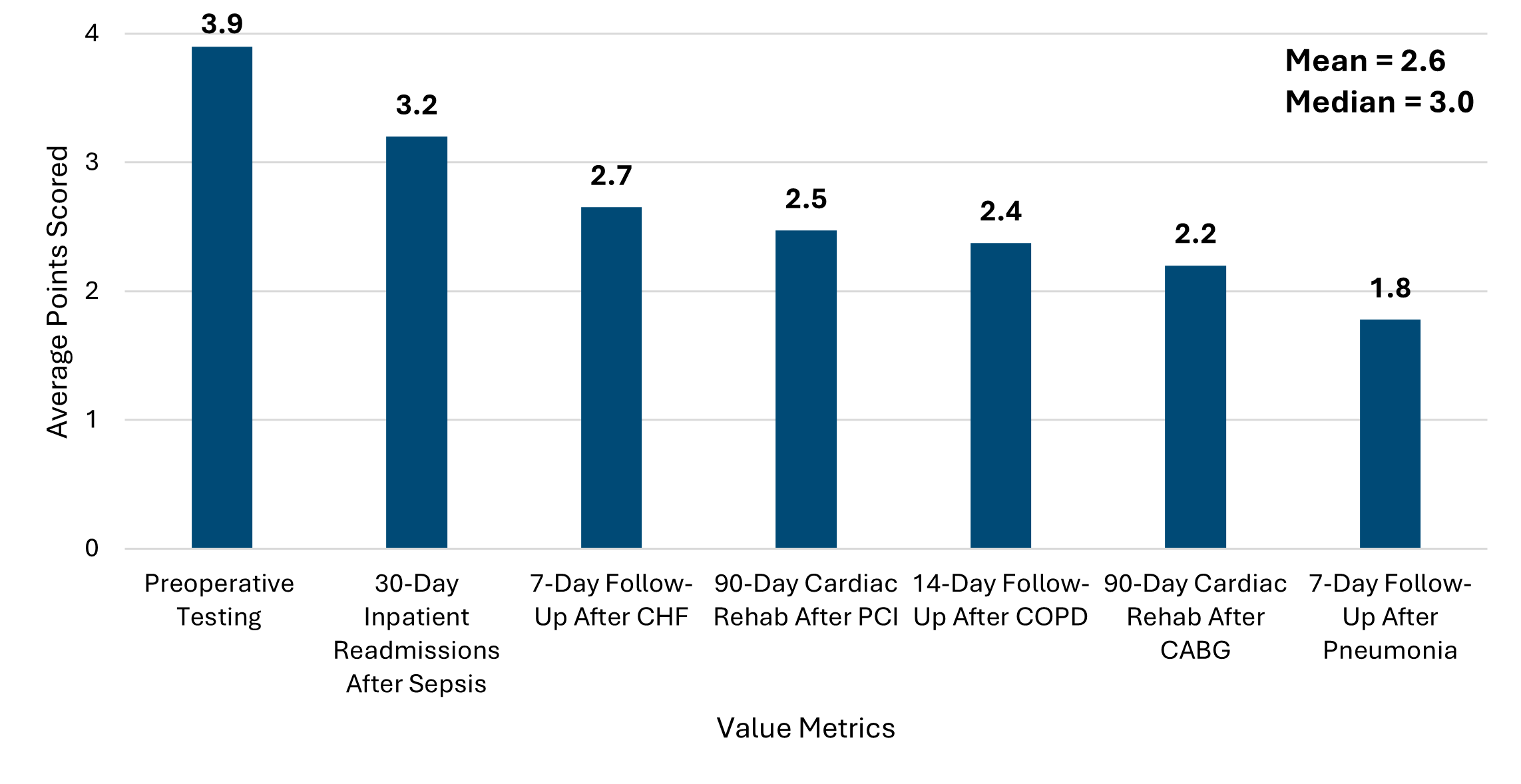
Figure 4 illustrates the breakdown of average points by value metrics. Consistent with PY 2024, the highest scoring value metric was preoperative testing with 3.9 points followed by 30-day inpatient readmissions after sepsis with 3.2 points. The lowest scoring value metric was 7-day follow up after pneumonia and follows the same trend as that of PY 2024 with 1.8 points.
Figure 4.
This is the second year of a two-year (PY 24-25) P4P cycle. The full methodology for this program cycle can be found in the PY2024-2025 technical document.
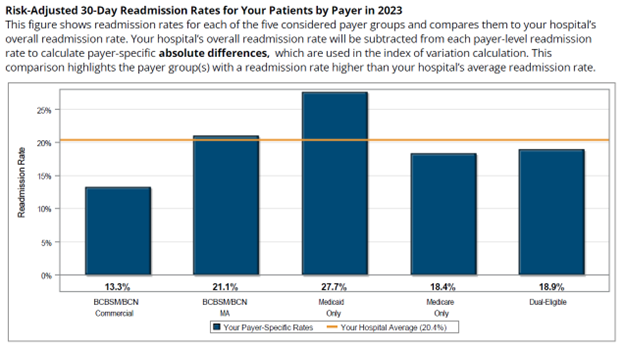
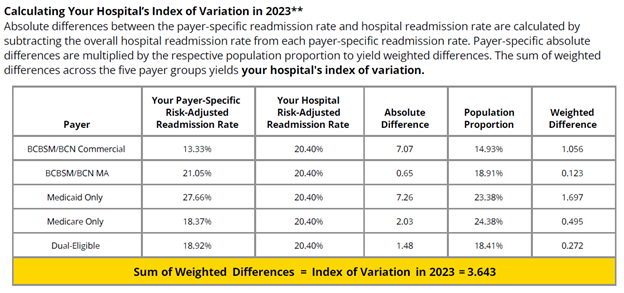
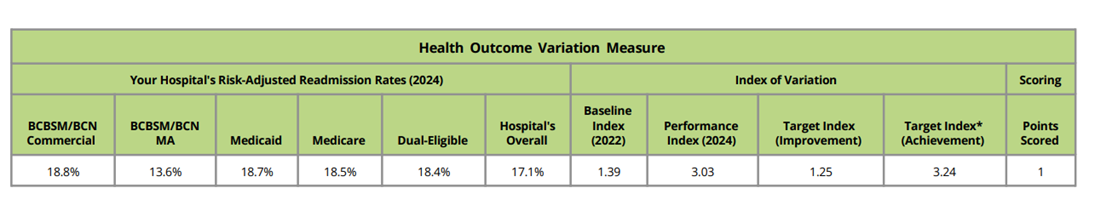
In addition to the PY 2025 mid-year scorecard summary, this report also included a preview of the new health outcome variation measure scoring, which will be worth one point in PY 2026-2027 (Figure 5). The table presents the hospital’s payer-specific risk-adjusted readmission rates in the performance year, the baseline and performance indexes for the hospital, and the target indexes required to score a point via improvement or achievement. This table’s scoring is based on PY 2025 data (i.e., 2024 performance year data and 2022 baseline data). Please note that this table was included to help orient members to the scoring methodology for this new measure and does not impact PY 2025 scores. For detailed information about this measure, please refer to this introductory video and PY 2026-2027 P4P technical document.
Figure 5.
These PY 2025 P4P mid-year scores are subject to change as new data is added. The final scores will be distributed after all 2024 claims are incorporated into the calculations. Hospitals can track their score via the P4P PY 2024-2025 dashboard reports on the MVC registry, which provides all relevant scoring information for both improvement and achievement points. These registry reports can be filtered by selected conditions/metrics to make tracking of P4P points easier. You can also contact the MVC Coordinating Center [EMAIL] for a walkthrough of your hospital’s PY 2025 mid-year scorecard or P4P registry reports.