In September, MVC hosted two virtual workgroup presentations – the first, a sepsis workgroup focused on Henry Ford Health Macomb’s efforts to build a structured emergency department (ED) triage process specifically for patients diagnosed with sepsis. The second, a health in action workgroup focused on the recent MVC Common Conditions and Procedures Report and included an overview of how to combine this push report with MVC registry data. The MVC Coordinating Center hosts workgroup presentations twice per month covering a variety of topics including post-discharge follow-up, sepsis, cardiac rehab, rural health, preoperative testing and health in action.
Sepsis Workgroup September 9, 2025
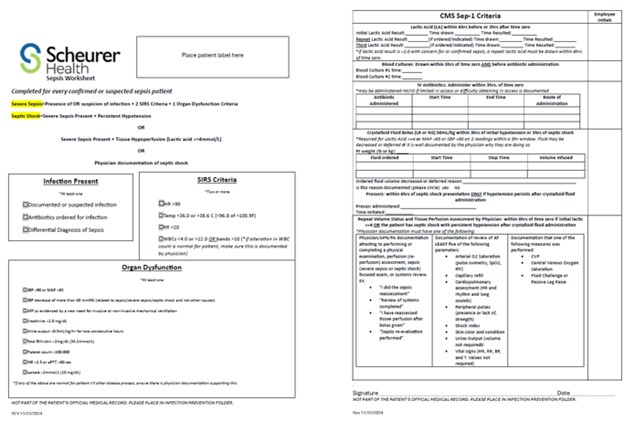
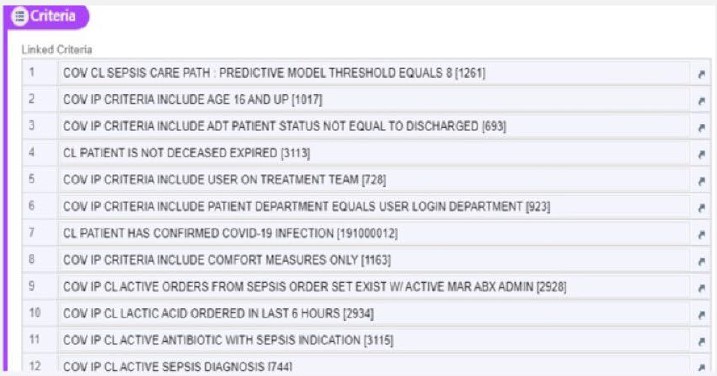
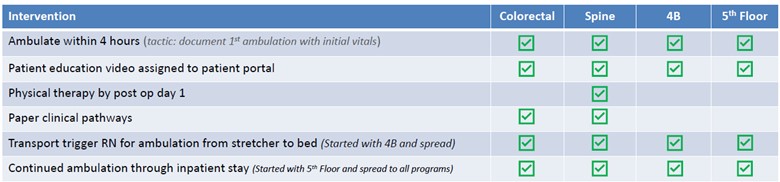
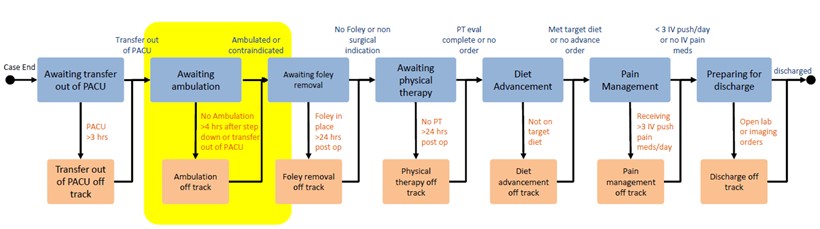
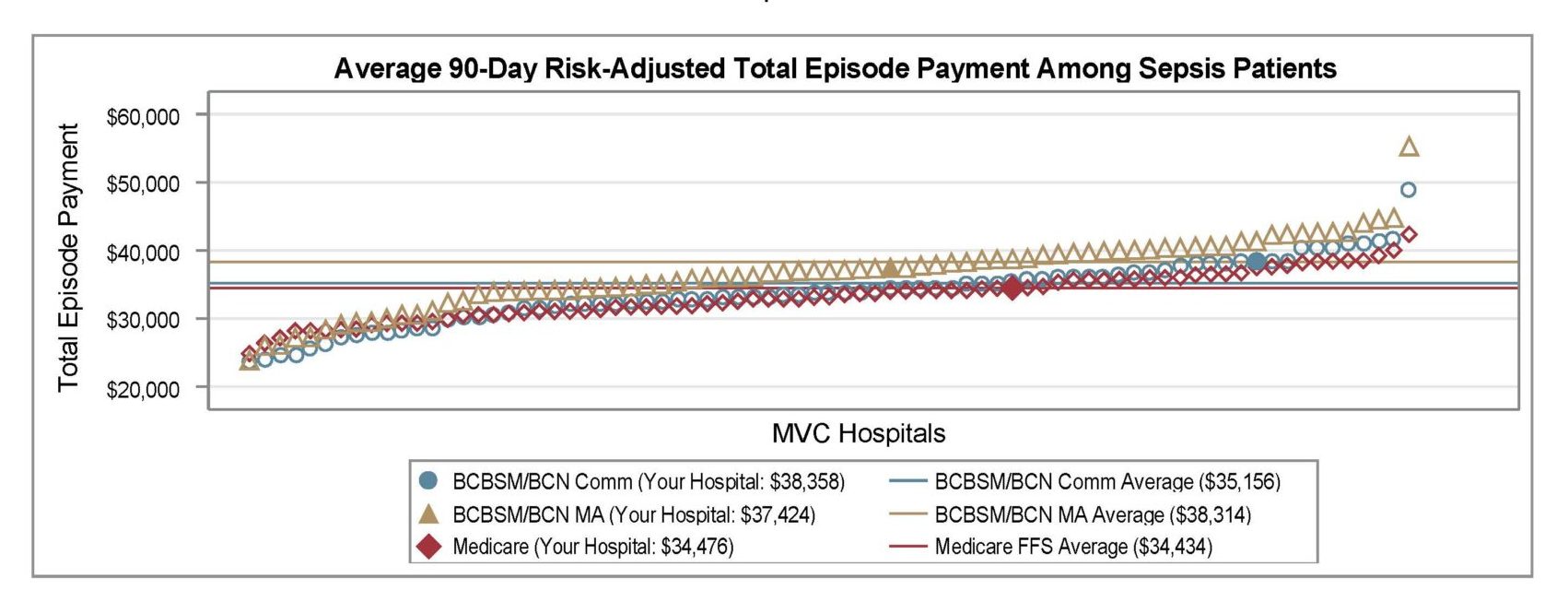
As Brandie DeVos, RN, MSN, Sepsis Coordinator explained at the beginning of the presentation, sepsis continues to challenge hospitals due to its time sensitive nature. Delays in recognition or treatment can lead to worse outcomes. Henry Ford Macomb Hospital’s ED sepsis team – composed of Michigan Hospital Medicine Safety Consortium (HMS) coordinators, internal sepsis program, and ED leadership – was established to combat just this issue. Their mission, to build a structured ED triage process, with specific attention to patients suspected of sepsis who present with abnormal vital signs to ensure the rapid identification, prioritization, and early intervention in suspected sepsis cases (Figure 1).
Co-presenters, DeVos and Errin Couck, BSN, RN, HMS Sepsis Coordinator, emphasized that having a consistent, structured triage process has helped to ensure cases of sepsis are not missed in the chaos of the ED. They recognized that prior to the initiation of a triage process directed at identifying sepsis, patients were being placed throughout the ED regardless of the presence of symptoms, vital signs indicating organ dysfunction, or indications of systemic inflammatory response syndrome (SIRS) criteria.
Figure 1. Walk-In Triage Process for Sepsis
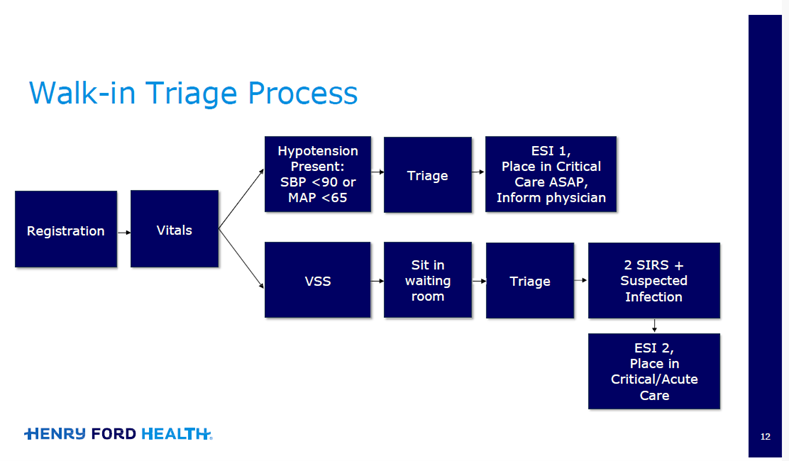
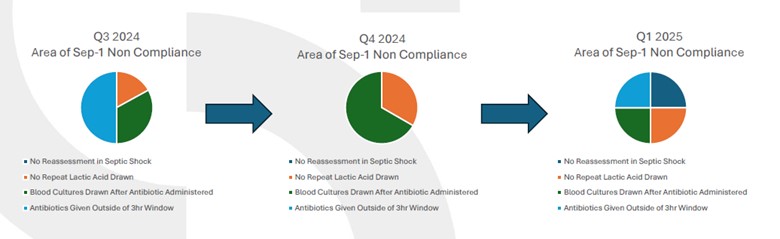
However, the triage system does more than mechanically screen vitals; it incorporates clinical judgement and risk indicators to prioritize patients with abnormal temperatures, elevated heart rate, hypotension, or altered mental status (Figure 2). The optimized identification of at-risk patients increases adherence to evidence-based sepsis bundle elements such as early labs, cultures, antibiotics, and fluid resuscitation within the defined time windows, a crucial step to improving performance in quality metrics.
Figure 2. Code Sepsis Activation Process
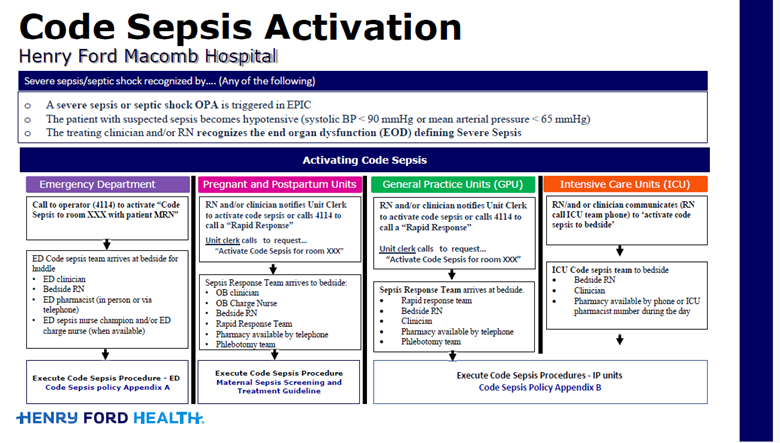
However, in practice, the sepsis program requires the support of a multidisciplinary team. DeVos and Couck note the most common roadblocks to this initiative were staff push back, untrained RNs in the triage area, and RN fatigue. They encourage aligning all stakeholders early and sustaining communication channels. They also noted great success with positive encouragement (i.e., celebrating the small wins), requiring triage RNs to have at least one year of ED experience, and routine triage RN rotations (every four hours).
Since initiating the new triage process, the presenters noted the following positive outcomes:
- A 36% increase in antibiotics given within three hours of arrival for septic shock patients
- For emergency medical services (EMS) patients, vital signs are obtained, triage completed, and patients roomed appropriately in an average of 12 minutes
- 90% of lobby patients have vital signs obtained within 5-10 minutes
- Overall, less patient triage complaints
The presenters ended the presentation by discussing a challenge they have experienced when attempting to expand their sepsis ED triage process to other sites within their own system. Hospitals differ – in size, resources, patient volume, and staffing. DeVos and Couck encouraged participants to pilot, learn, and iteratively refine their workflows locally.
This workgroup session served as both a practical guide and a rallying call – a structured ED triage for suspected sepsis should not be optional. It’s a critical defense against delays that cost lives.
MVC Sepsis Workgroup Sept. 9, 2025
Health in Action Workgroup September 25, 2025
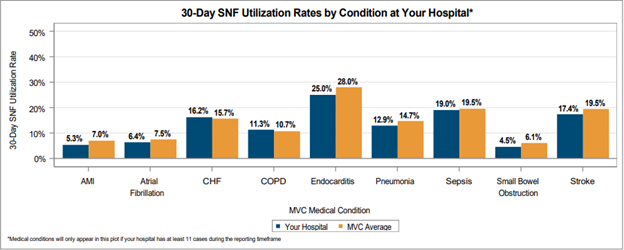
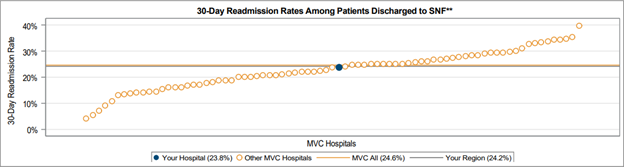
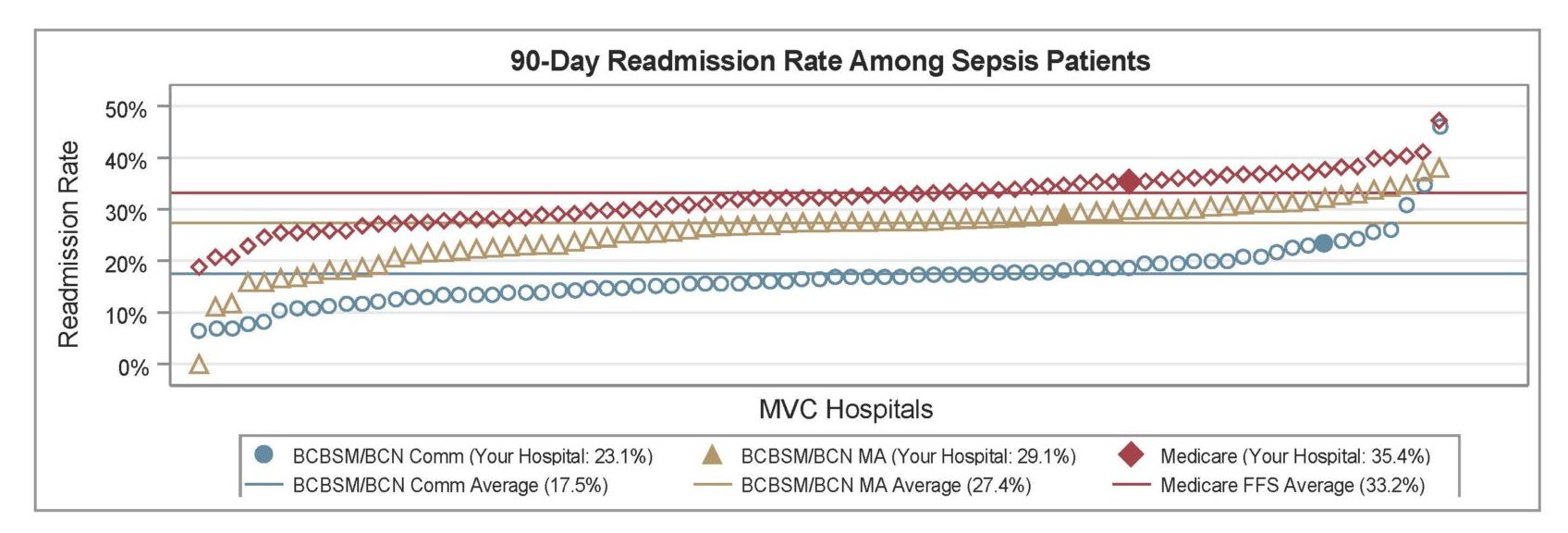
The September health in action workgroup featured a presentation by MVC’s Site Engagement Coordinator Emily Bair, MS, MPH, RDN, CSP. The presentation focused on the recent MVC Common Conditions and Procedures Report and included an overview of how to utilize the MVC registry to compliment analyses included in this push report.
The Common Conditions and Procedures Report was developed as a structured data tool aimed at providing individualized, comprehensive, high-impact trends in commonly seen chronic conditions and a selection of procedures across participating hospitals. The most recent version of this report was shared with members in July. Two previous versions of the report were shared in 2024 and 2023.
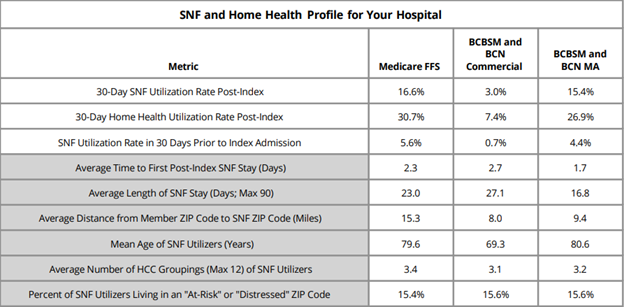
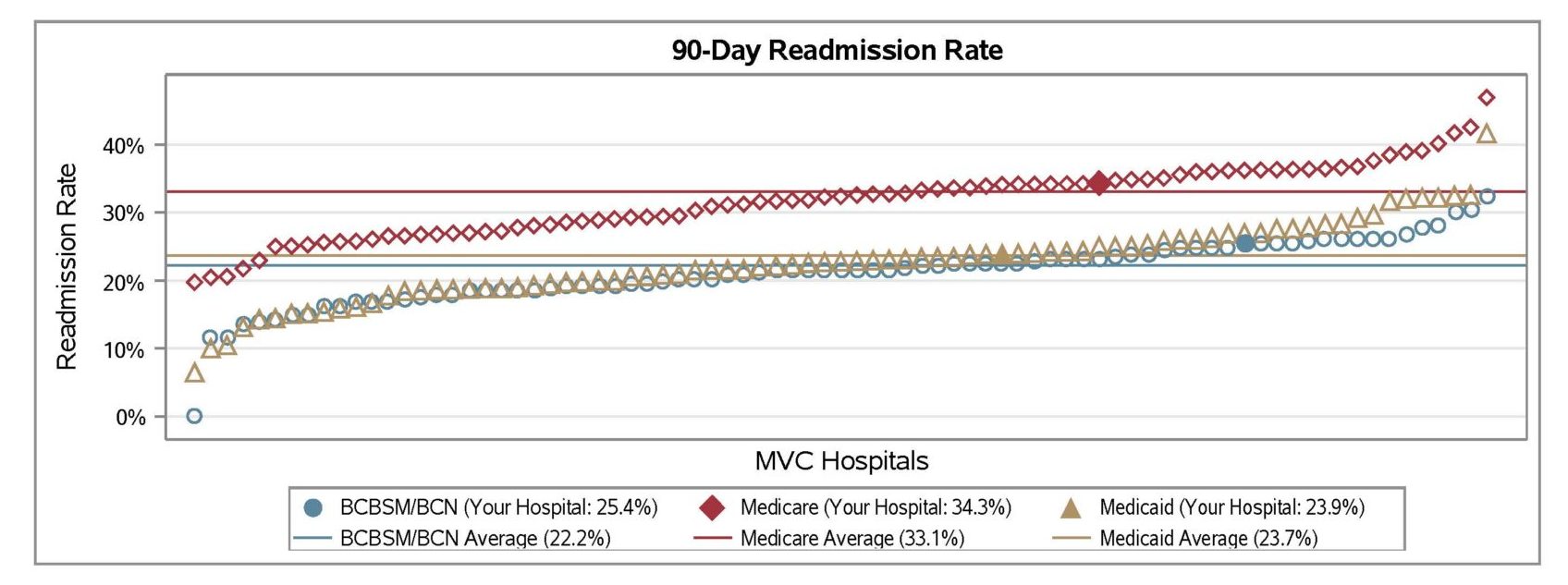
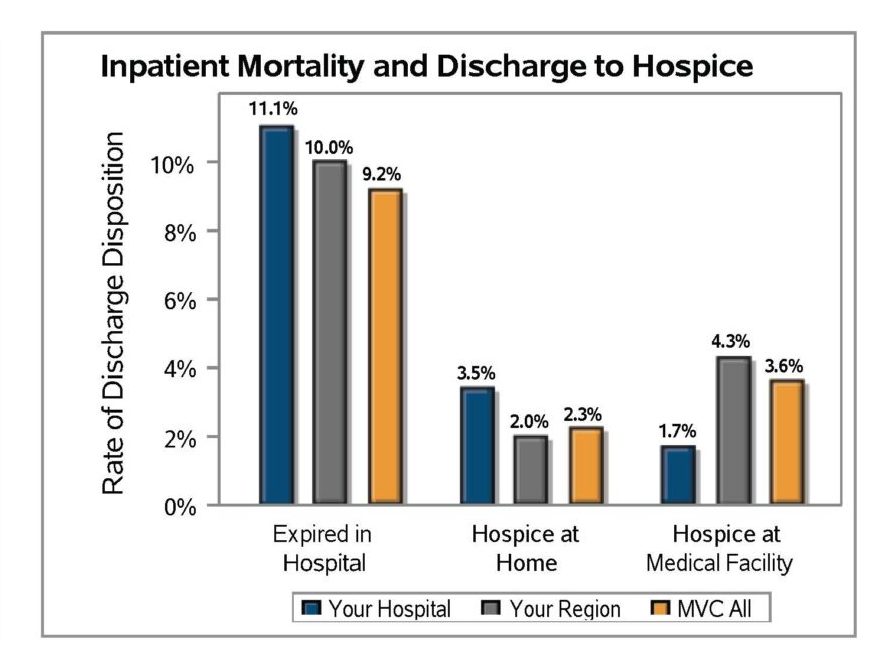
Similar to previous iterations of the report, the most recent Common Conditions report included 30-day inpatient or surgical episodes created from two years of index admissions between January 2023 – December 2024. Exclusions included patients who had an inpatient hospital transfer, died in the hospital during their index hospitalization, or were discharged to hospice. Payors included Blue Care Network HMO Commercial and Medicare Advantage, Blue Cross Blue Shield of Michigan PPO Commercial and Medicare Advantage, Medicare Fee-for-Service, and Michigan Medicaid.
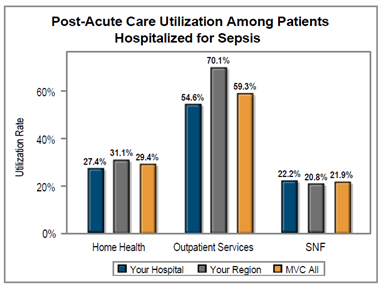
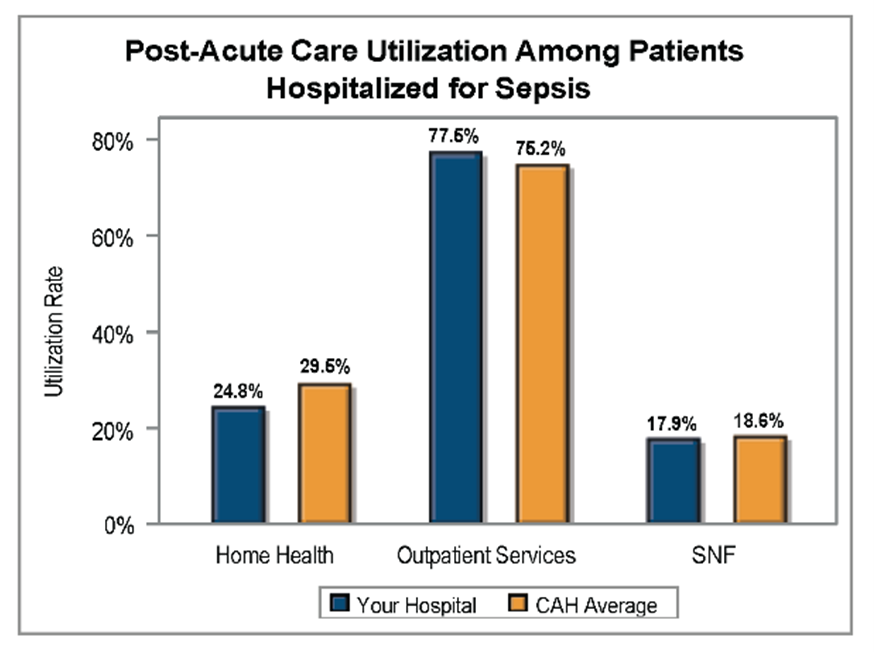
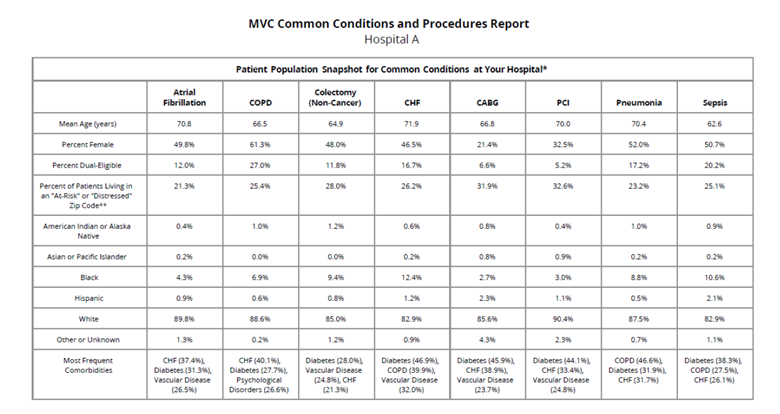
Within each report each site has an individualized patient population overview table that displays the patient population for each common condition (Figure 3). This table illustrates the distribution pattern of the population within each common condition but is not necessarily indicative of the distribution of patient demographics for the outcome of interest. In addition to age, gender, and race/ethnicity categories, the table includes zip code level data based on the Economic Innovation Group’s Distressed Communities Index (DCI) 2015-19, dual-eligible status, and common comorbidities.
Figure 3. Common Conditions Patient Population Snapshot for Hospital A (Blinded Data)
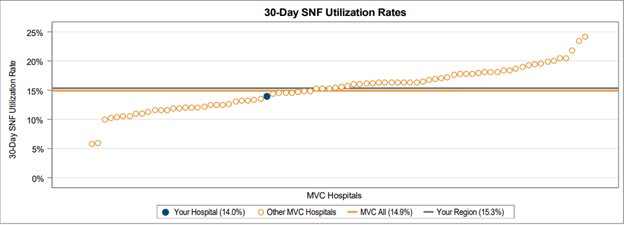
The report then features a variety of analyses for each condition/ procedure with an emphasis on:
- Benchmarking: the report allows each hospital to see how it compares to peers on metrics like readmission rate, post-discharge care utilization, and episode cost
- Longitudinal trends: by presenting trends (6-month intervals) hospital leadership can detect historical problems or successes
Figure 4. Common Conditions Report Page for Atrial Fibrillation for Hospital A (Blinded Data)
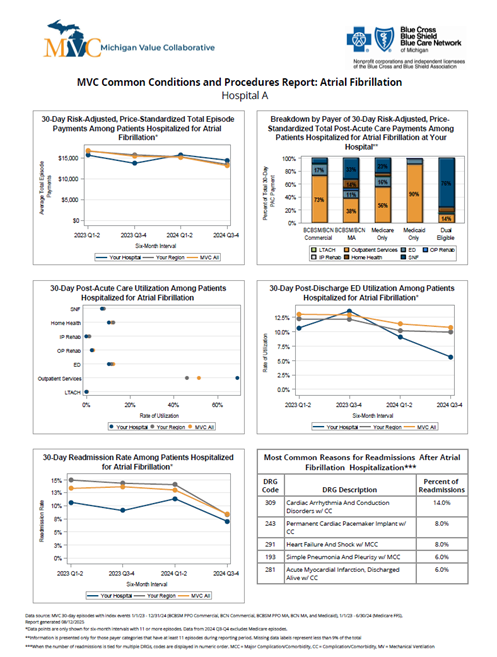
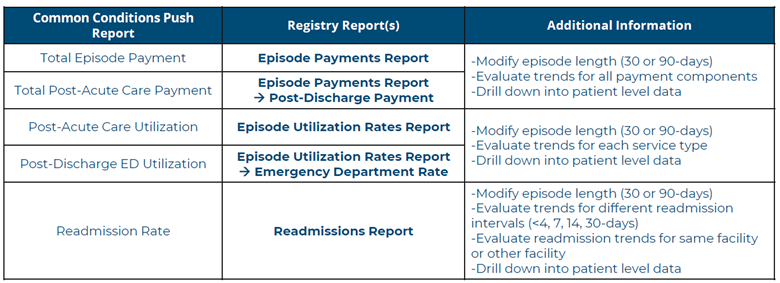
The design of this workgroup is part of MVC’s broader efforts to support hospitals not just with data, but with actionable insights and engagement strategies. As Bair points out, data alone isn’t enough – it’s the interpretation and follow-through that drives real change. Bair followed her review of the Common Conditions report with a walk-through of relevant online data registry reports (Figure 5).
Figure 5. Summary of Relevant Reports on MVC Data Registry
In an effort to continue to support hospitals to move from simply viewing data to implementing quality improvements, Bair outlined a few key MVC engagement strategies:
- Outreach and coaching: MVC offers one-on-one coaching to support members with data interpretation and connections to peers
- Custom analytic report development: MVC may facilitate the development of deeper data analyses
- Peer learning and collaboration: MVC aims to catalyze dialogue across sites, encouraging sharing cross-hospital learning
- Iterative feedback: MVC welcomes feedback from members to support the evolution of data tools
MVC Health in Action Workgroup Sept. 25, 2025
Interested in access to the MVC data registry?

Once a registry request is received, the MVC team will confirm your request with your specified site’s MVC Site Coordinator (primary contact). Once confirmed, you will be sent an MVC website confidentiality agreement (WCA), and upon receiving the completed WCA, MVC will provide you with a username and directions to login via email.
If you are interested in pursuing a healthcare quality improvement project, MVC has data specialists available to help you navigate our data resources and create custom analytics reports to support your efforts. Please reach out to us by email if you would like to learn more about MVC data or engagement offerings!