The Michigan Value Collaborative (MVC) held its first semi-annual meeting of 2022 last Friday. A total of 158 leaders joined the MVC Coordinating Center’s virtual meeting, representing 68 different hospitals and 15 physician organizations (POs) from across the state of Michigan. “Turning Data and Collaboration into Action” was the theme of this year’s first semi-annual, putting the spotlight on quality initiatives that successfully leveraged data or collaboration to bring about improvements in healthcare.
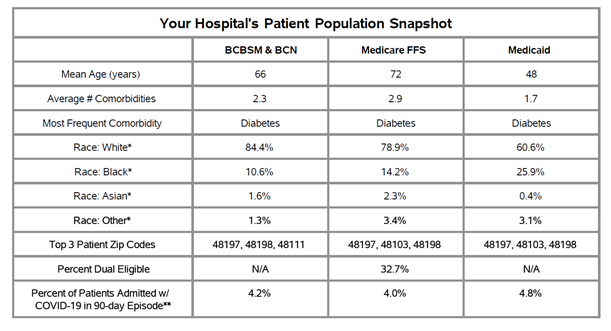
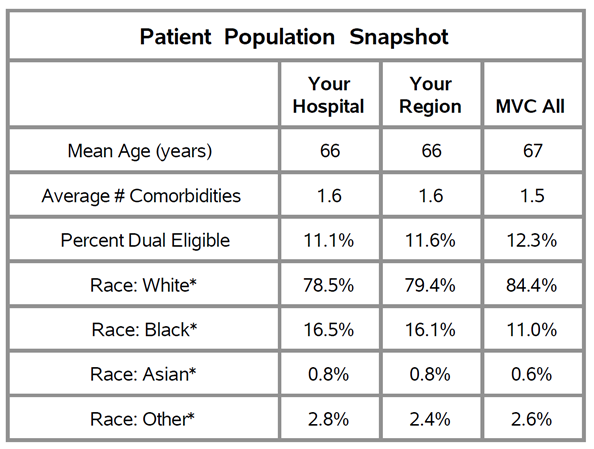
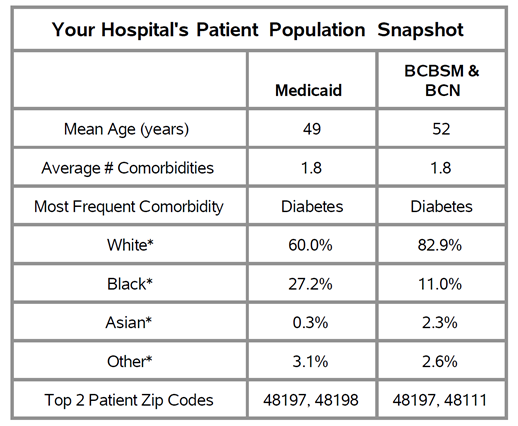
MVC’s Director, Dr. Hari Nathan, kicked off Friday’s meeting with an update from the MVC Coordinating Center. He welcomed two new collaborative members, McLaren Caro Region and UP Health System - Bell, as well as MVC’s newest team member, Engagement Associate Chelsea Andrews. Dr. Nathan also highlighted the successes delivered by the Coordinating Center during the first six months of 2022. This included the incorporation of Medicaid data into MVC’s suite of push reports to provide a more complete view of the collaborative’s patient population, the launch of three new push reports (colectomy, pneumonia, and P4P), and the incorporation of additional demographic data into MVC's reporting.
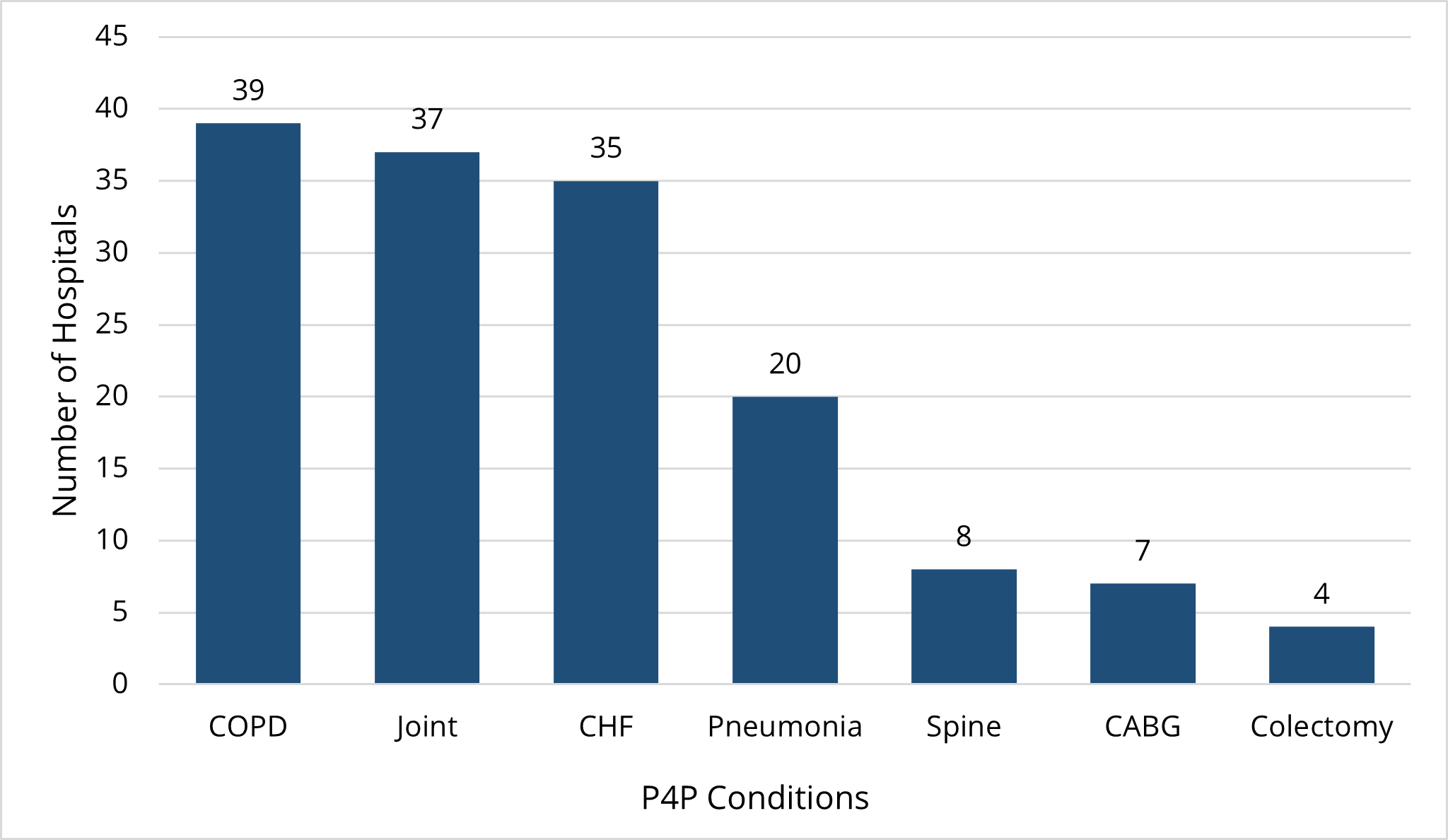
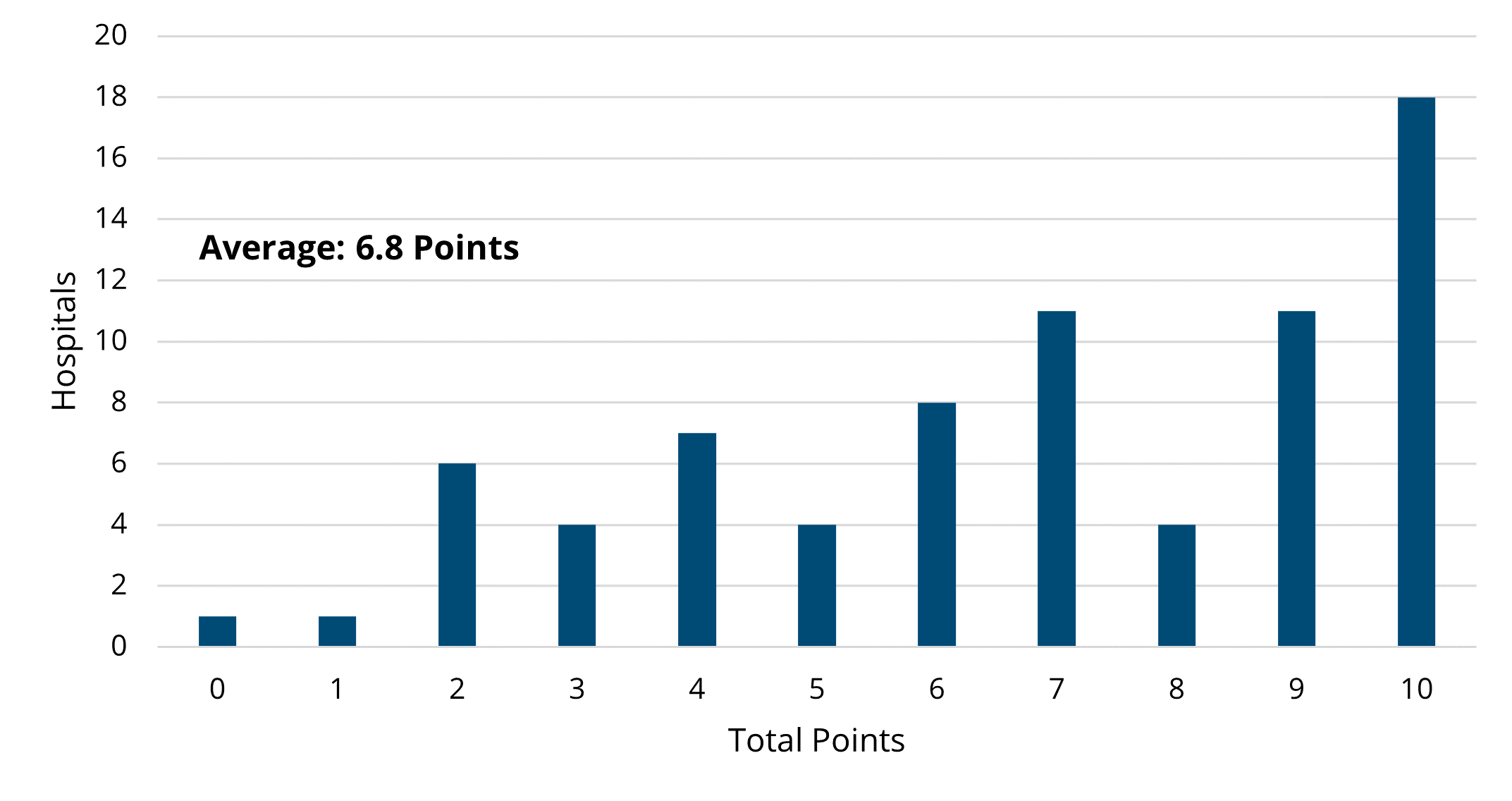
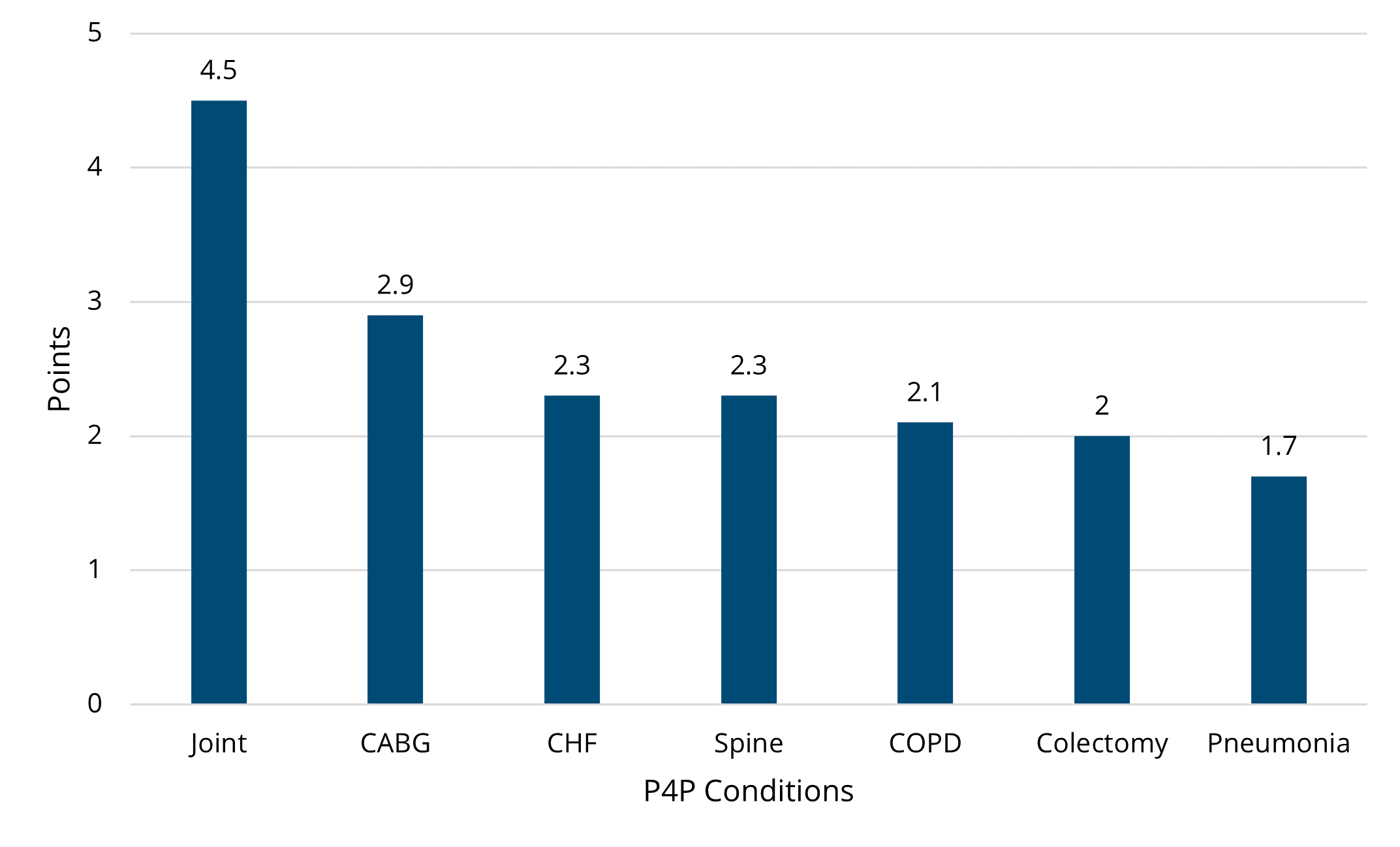
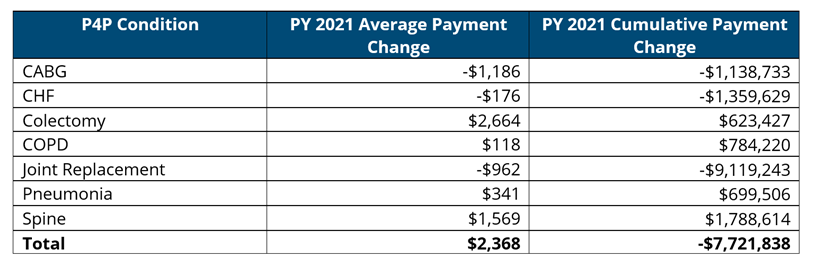
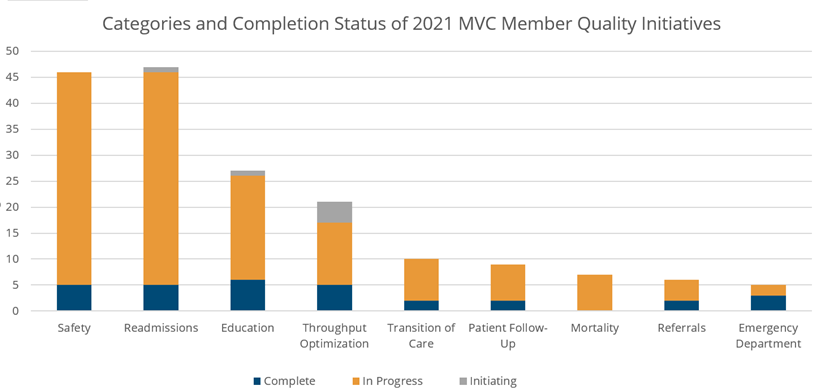
MVC’s recent Qualified Entity accreditation was also highlighted, representing a breakthrough for the collaborative that will allow the relaxation of certain data use agreement regulations and improve the granularity of data available to members. As part of extending this improved access, the Coordinating Center will reach out to site coordinators to have authorized representatives at each institution complete a new data use form. To align with the security requirements of the Qualified Entity program, the MVC registry will also begin requiring multi-factor authentication for users upon login. More information on each of these elements will be shared with the collaborative in the coming weeks. Chelsea Abshire Pizzo, MVC’s Manager of Analytics, rounded off the meeting welcome by sharing some highlights from Program Year 2021 of the MVC Component of the Blue Cross Blue Shield of Michigan Pay-for-Performance (P4P) Program.
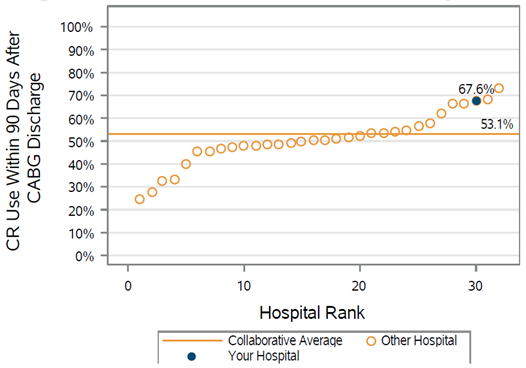
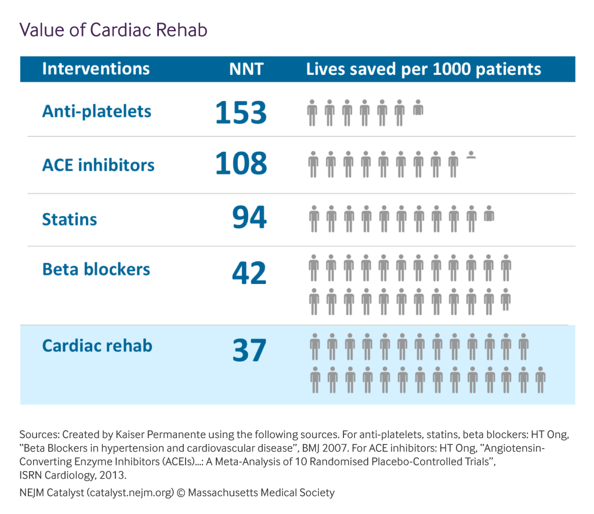
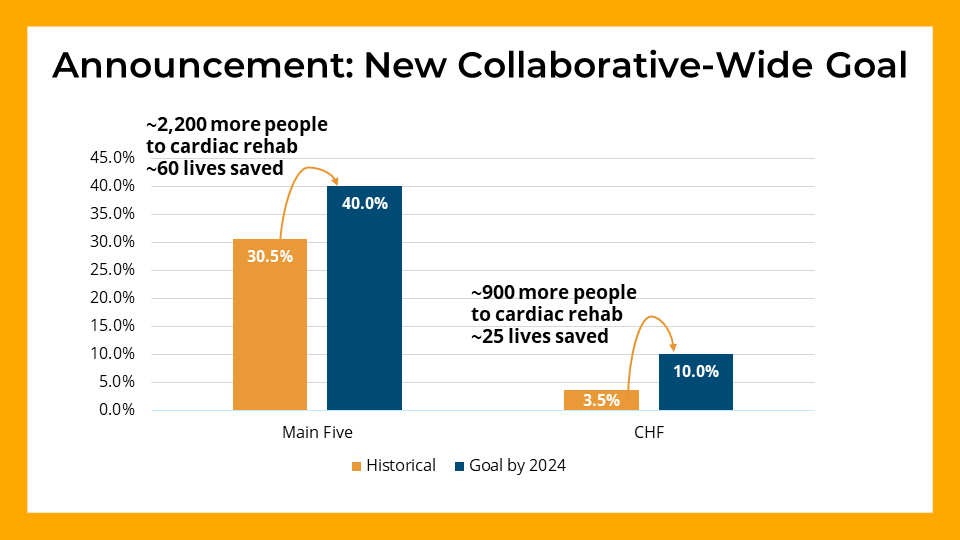
Showcasing opportunities where MVC data can drive change was a focal point for the meeting. Utilizing unblinded data from the collaborative, MVC Analyst Jessica Yaser led attendees through a data session focused on MVC’s two Value Coalition Campaigns (VCCs): Preoperative Testing and Cardiac Rehab. This allowed attendees to see their preoperative testing and cardiac rehab utilization rates compared to their peers. Hospitals performing well were invited to offer insights as to how this was achieved and what mechanisms other hospitals could adopt to improve performance levels. Jessica also announced new collaborative-wide goals around cardiac rehab utilization rates (see Figure 1), which will continue to be promoted and highlighted in the months ahead.
Figure 1.
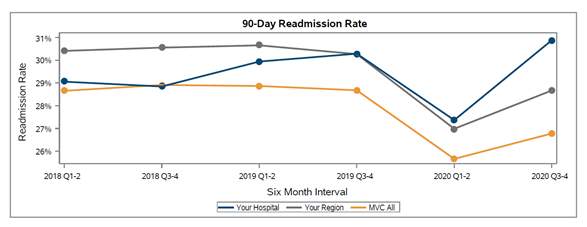
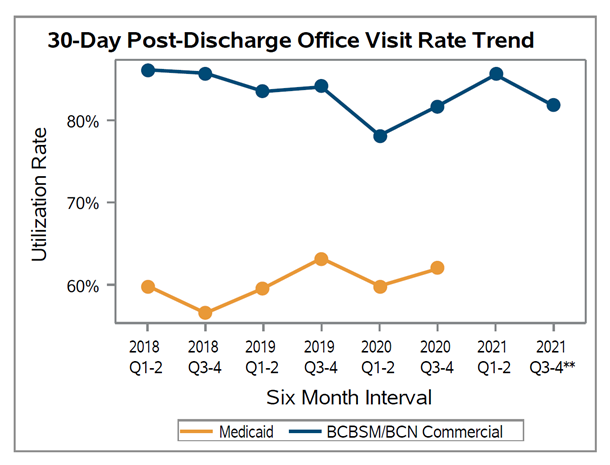
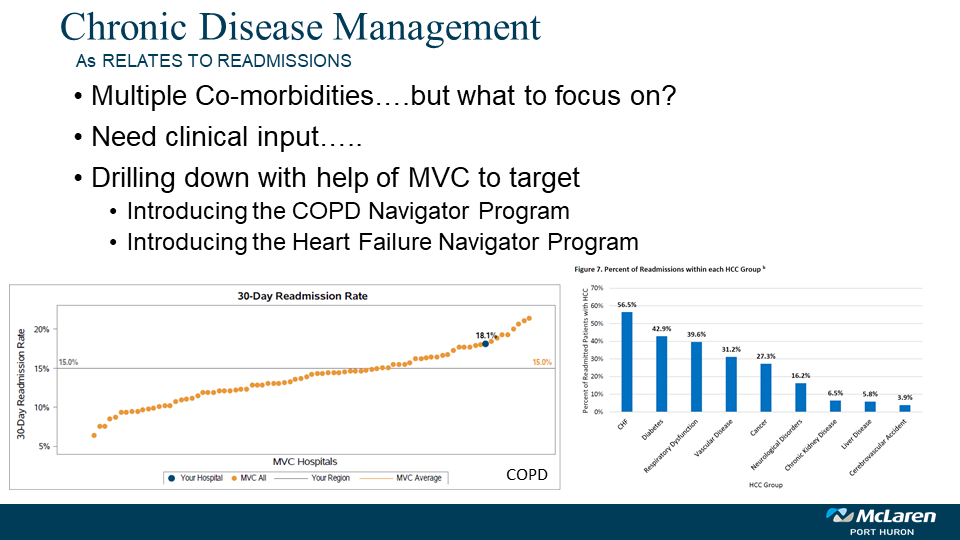
With the scene set, MVC welcomed guest speakers Mary Pool and Holly Gould from McLaren Port Huron hospital. Mary and Holly provided attendees with an overview of how they have used MVC data to help tackle high readmission rates for the congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD) patient populations at McLaren Port Huron. Specifically, data provided by the Coordinating Center helped confirm the suspicion that although follow-up rates were high across the institution, this wasn’t being translated into a reduction in readmissions. Stratifying these data further helped McLaren Port Huron introduce tailored initiatives in the form of their COPD and Heart Failure Navigator Programs, aimed at driving the effectiveness of follow-up visits (see Figure 2).
Figure 2.
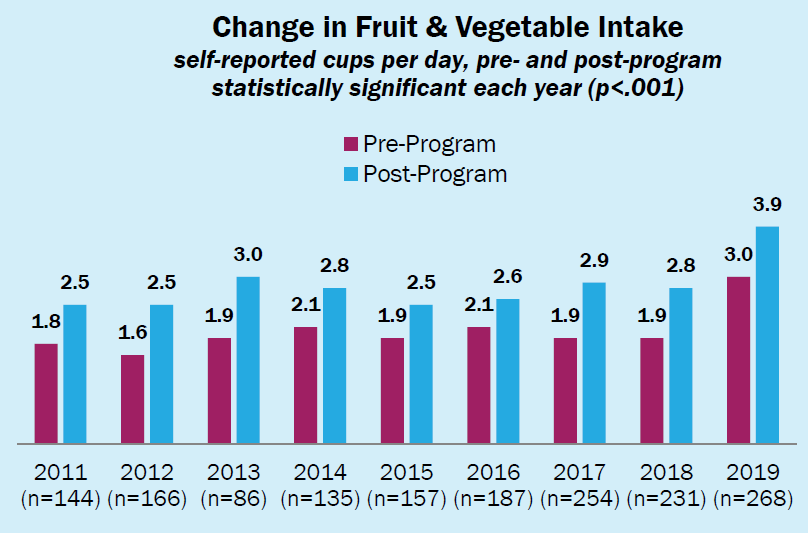
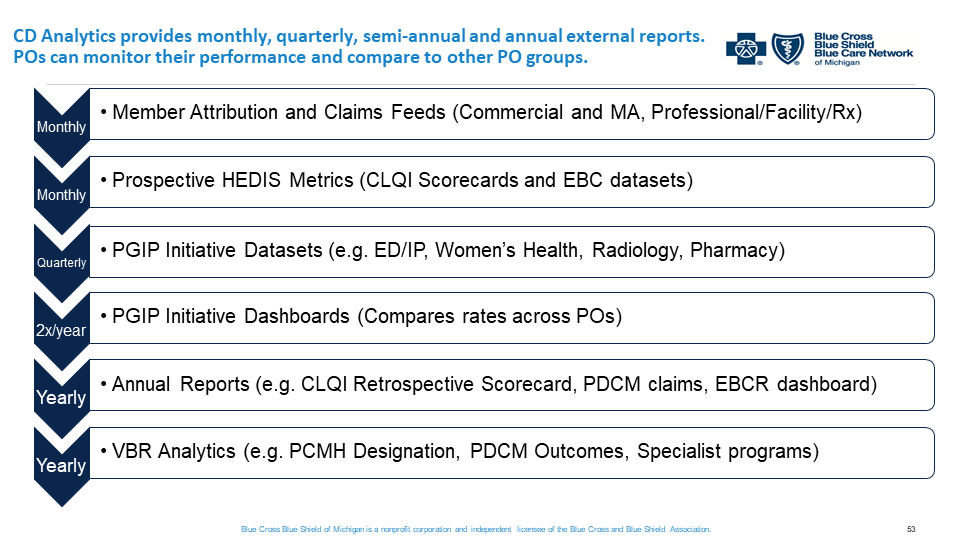
After hearing from McLaren Port Huron, Michelle Marchese from BCBSM provided an overview of how their Physician Group Incentive Program (PGIP) platform supports value-based care. As part of this, Michelle provided a walk-through of the current state of BCBSM data and report sharing, outlining how these all fit together to provide valuable healthcare insights for physician organizations (POs) (see Figure 3). MVC’s ongoing partnership with BCBSM to identify PO-level opportunities for improvement was also highlighted – a collaboration that will continue moving forward to enhance the level of support available to POs across the state. Michelle then passed the baton to Dr. Shannon Martin from MyMichigan Health who shared how MyMichigan has used its internal data to develop, implement, and assess its “Health Aging Program.” This initiative is aimed at decreasing the use of high-risk medications in the elderly population, saving many seniors from the harm of adverse drug effects.
Figure 3.
The meeting concluded with a summary of the day and key upcoming activities, led by MVC Engagement Associate Chelsea Andrews. The recording from Friday’s meeting is available here. If you have questions about any of the topics discussed at the semi-annual or are interested in finding out more about MVC, please reach out to the Coordinating Center. MVC’s next semi-annual meeting will be in person on Friday, October 28 at the Radisson in Lansing – we look forward to seeing you all then!