CHF Workgroup Discusses Value of Outpatient Intravenous Diuresis
The Michigan Value Collaborative (MVC) holds bi-monthly virtual workgroups on six different clinical areas of focus. The goal of these workgroups is to bring collaborative members together to discuss current quality improvement initiatives and challenges. These six different clinical areas include chronic disease management (CDM), chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), diabetes, joint, and sepsis. At the most recent MVC CHF workgroup, the discussion centered around inpatient versus outpatient intravenous diuresis for the acute exacerbation of CHF.
The prevalence of heart failure in the United States is increasing, with one study indicating it affects more than 5.7 million people. The study reports that up to 80% of patients with acute decompensated heart failure (ADHF) visit their emergency departments and that 91.5% of those patients were thereafter readmitted to the hospital for diuresis.
With increasing prevalence comes greater direct and indirect healthcare costs associated with CHF, accounting for approximately $40 billion annually in the United States. For patients over the age of 65, it is a leading cause of hospitalization with annual costs of $11 billion.
Despite significant costs and healthcare burden associated with this condition, the same study finds that no official guidance exists regarding an appropriate location for therapy. Since hospital readmission reduction programs seek to incentivize reductions in readmissions, it is important to simultaneously provide guidance to providers and patients on safe and effective options for outpatient treatment and therapy.
To address this concern, the workgroup discussed the benefits and safety of outpatient intravenous (IV) diuresis and how the outpatient administration of furosemide can be safe and effective. MVC members shared their experiences with setting up these clinics, their inclusion criteria, and other protocols. A standard diuretic protocol could include each patient being given an IV furosemide bolus with continuous infusion within the most appropriate outpatient setting, which could include the patient’s home or in a mobile clinic.
While in the outpatient setting, patients undergoing this treatment would be monitored via cardiac telemetry and appropriate blood panels before and after the infusion. Patients on maintenance medications are instructed to continue their standard dose in the outpatient setting as appropriate based on their individualized treatment protocol. Patients should follow up with their cardiology and primary care teams to maintain their treatment and care maintenance plans. Following the outpatient IV diuresis encounter, the study reported patients had lower costs, fewer hospital stays, and lower mortality risk than CHF patients who did not receive outpatient IV diuresis.
Overall, studies indicate that outpatient CHF IV diuresis treatment is a safe and effective method of relieving CHF symptoms with a low risk of adverse events. The MVC members in attendance had positive thoughts and experiences regarding outpatient IV diuresis clinics and would recommend further discussion on them. The outpatient mobile CHF diuresis clinic was of notable interest to the MVC members in attendance and will be considered for a specialty topic in future workgroups and blog posts.
The MVC Coordinating Center is interested in hearing how your organization is improving CHF patient care and reducing CHF hospital readmissions. If you would like to present at or attend an upcoming MVC workgroup, please contact the MVC Coordinating Center at the michiganvaluecollaborative@gmail.com.
Healthcare Leaders Issue Support for Climate Change Mitigation
The past year forced healthcare to grapple with never-before-seen challenges. In response, facilities and clinicians found ways to think creatively, adapt, and find common ground with peers to best steward the health and safety of our communities. But the pandemic isn’t the only challenge requiring that kind of response. The healthcare industry is placing greater emphasis than ever before on the issue of climate change amidst the news and commitments coming out of the 2021 United Nations Climate Change Conference, also known as COP26.
The greater emphasis following this year’s conference is perhaps related to an increased overall focus on direct impacts to public health as well as the looming presence of a global pandemic that nearly all countries have struggled to manage. Countries like Britain are looking to reduce emissions by piloting a first-of-its-kind zero-emissions ambulance, citing that air pollution contributes to one out of every 20 deaths in the United Kingdom. The new vehicle was parked and promoted at the events in Glasgow. It is also notable that the healthcare industry has been increasingly concerned with variability in health outcomes due to social determinants of health; the impacts to human health by climate change and environmental pollution are also felt disproportionately by vulnerable communities.
The COP26 commitments included one from the U.S. Biden Administration to halve the United States’ greenhouse gas emissions by 2030. According to Health Care Without Harm (HCWH), an international nongovernmental organization concerned with mitigating healthcare’s impact on environmental health, “the U.S. health sector is responsible for 8.5% of U.S. greenhouse gas emissions and 27% of the global health care emissions… Addressing the climate crisis as a core driver of disease must be central to the health sectors’ mission today and in the future. As a fundamental sector in our society, and the only sector with healing as its mission, it makes sense for health care to lead the way to kick our addiction to fossil fuels, improve public health, and save billions of dollars in health costs in the process.”
They posited that healthcare has a unique relationship with climate change because of healthcare's role in bearing the financial costs and human health burden (see Figure 1 from the Centers for Disease Control and Prevention) from “increased disease spread and more frequent extreme weather events.”
This belief is shared by at least 45 million healthcare workers (which represents 75% of the health professionals in the world) associated with letters urging immediate action on climate change. There are already leaders in these efforts throughout the U.S. The Healthcare Climate Council created a playbook (see Figure 2) for operationalizing climate solutions in areas such as energy, food, leadership, operating rooms, purchasing, infrastructure, transportation, and waste.
The playbook contains success stories of facilities that have made meaningful changes, such as one about the Cleveland Clinic saving more than $4 million in 2019 by reducing air changes per hour during non-surgical periods as part of their Operating Room Setback Plan. They save 25 million kWh/year in energy use and $2.5 million annually. Similarly, Ascension deployed a data dashboard to report facility operations (energy, water, temperature, humidity, and air changes) on a real-time basis, and they implemented a pulse oximeter collection project that resulted in 664,000 medical devices collected and 66.4 tons of landfill waste avoided. They reported that this effort required collaboration between green teams, the purchasing department, environmental services, clinicians, facility managers, and the medical device reprocessing vendor.
Quality improvement efforts in healthcare have always been multifaceted, seeking to systematically reduce variation and improve outcomes by standardizing processes and structures. Quality professionals look at technology, personnel, culture, physical capital, leadership, training, operations, and procedures, among other areas. This means that healthcare’s quality improvement teams are uniquely positioned to support their leadership in identifying and implementing climate solutions. These changes that help mitigate climate impacts also often lead to more efficient, sustainable care delivery.
There are a number of professional organizations ready to assist and offer guidelines for practice improvement, including Health Care Without Harm, its sister organization Practice Greenhealth, the Alliance of Nurses for Healthy Environments, the American Society of Anesthesiologists, the Association of American PeriOperative Registered Nurses, and the American Academy of Family Physicians, among others.
Much like with the COVID-19 pandemic, the actions and decisions of one facility, community, or country ultimately have an impact on everyone else, which means a culture of collaboration is a prerequisite for the successful integration of climate change mitigation in healthcare. If your hospital or physician organization has achieved value or outcome improvements that relate to environmental health or sustainability, the MVC Coordinating Center can help share your story. Please contact the MVC team at michiganvaluecollaborative@gmail.com.
Introducing MVC Engagement Associate Chelsea Andrews, MPH
I would like to take this opportunity to introduce myself as the Michigan Value Collaborative’s (MVC) new Engagement Associate. As the Engagement Associate, I will work closely with the Site Engagement Manager and Site Engagement Coordinator to foster collaboration among members and other stakeholders and drive outreach efforts that facilitate statewide cross-institutional learning. I am excited to join the MVC Coordinating Center and look forward to getting to know our sites and members.
Colleagues would call me a well-versed health and wellness leader with an authentic and collaborative approach to program management who creates a positive and high-performing culture. I have worked in healthcare and health research in various capacities over the past 11 years, ranging from direct patient care to administration, and have co-authored multiple medical encyclopedia entries and actively contributed to NIH research. I’m a Michigan State University alumna with a pre-medical Bachelor of Science in human biology; a specialization in bioethics, humanities, and society; and a Spanish minor. After working as a nurse assistant in various specialties, I left the state of Michigan to earn my Master’s in Public Health in health systems, management and policy at the University of Colorado. While in Colorado, I was part of the administrative team for Colorado Medicine’s Department of Obstetrics and Gynecology - Division of Maternal Fetal Medicine. Since my return to Michigan in 2019 and prior to joining the MVC, I worked at the University of Michigan School of Nursing as Program Coordinator for the Alliance to Advance Patient-Centered Cancer Care, where I defined and executed project goals and acted as a liaison between the national program office teams, grantees, and board members.
I am passionate about comprehensive patient-centric operational procedures, community engagement, and reducing healthcare disparities. When I’m not working, you can find me playing with my dog and three cats, adventuring outside, working on cars, or reading next to a fire (I’m always accepting book recommendations). If you have any questions, please reach out to me at andreche@umich.edu.
MVC Component of the BCBSM P4P Program Year 2021 Update
The COVID-19 pandemic impacted hospitals throughout the state in 2020 and the MVC Coordinating Center deemed it necessary to evaluate the effect of COVID-19 on the MVC Component of the Blue Cross Blue Shield of Michigan (BCBSM) Pay-for-Performance (P4P) program. The goal was to determine if adjustments needed to be made to maintain fairness across the collaborative for index admissions in the calendar year of 2020, which will be used to score the 2021 program year.
The MVC Coordinating Center found that 223 of the 25,627 (0.9%) episodes included in the P4P conditions from the first half of 2020 had a code for confirmed COVID-19 infection in the index event or other inpatient settings. Pneumonia and congestive heart failure (CHF) were the most common conditions to have a COVID-19 diagnosis.
The MVC Component of the BCBSM P4P program rewards hospitals for either making improvements over their baseline episode payment or for being less expensive than peer hospitals. The MVC Coordinating Center has also found that episodes of COVID-19 patients are generally more expensive than typical episodes. Additionally, COVID-19 was not present in the baseline year of 2018 that hospitals will be evaluated against and hospitals were impacted differently.
Therefore, with approval from BCBSM, the MVC Coordinating Center will remove any 2020 episode with a COVID-19 diagnosis on an inpatient facility claim during the 30-day episode if the COVID-19 ICD code is one of the first three diagnosis codes on the claim. Please contact the MVC Coordinating Center with any questions at michiganvaluecollaborative@gmail.com.
Fall Semi-Annual Meeting Agenda Highlights Health Equity Topics
The MVC Coordinating Center recently released the full agenda for its forthcoming fall Semi-Annual Meeting on Friday, October 22, 2021, from 10:00-11:30 am. The MVC Coordinating Center holds collaborative-wide meetings twice each year to bring together quality leaders and clinicians from across the state. This year’s theme of “the social risk and health equity dilemma” is reflective of a growing priority within the healthcare system generally, as well as newer activities within the MVC Coordinating Center.
Speakers at semi-annual events are often members who share their stories of success, challenges, barriers, and solutions in pursuing a higher value and quality of care. The speakers outlined on October’s agenda showcase the breadth and depth of knowledge that exists within the collaborative in the health equity space. They also represent a variety of stakeholder groups, including hospitals, physician organizations (POs), Collaborative Quality Improvement (CQIs) programs, and of course MVC Coordinating Center leadership.
The first guest speaker will be Carol Gray, Program Manager of the new Michigan Social Health Interventions to Eliminate Disparities (MSHIELD) CQI. She leads the overall management, performance, and coordination of the MSHIELD program and Coordinating Center team. She has extensive experience managing public health research teams, communicating across and coordinating with multiple partnerships, and linking and engaging with community-based organizations in Detroit and academic faculty at the University of Michigan. Her presentation on, “Aligning Partnerships to Achieve Health Equity,” will speak to that expertise.
The meeting also features the expertise of Dr. Nicole J. Franklin, Assistant Medical Director at the McLaren Bariatric and Metabolic Institute. She provides psychological support to bariatric patients before and after weight loss surgery. In addition, Dr. Franklin is the chair of the Diversity and Inclusion Committee at McLaren Flint and has co-facilitated the Diversity Committee within all three local hospitals’ psychology training programs for the last 10 years. She is an Air Force veteran and a graduate of Wright State University’s School of Professional Psychology. Referencing her work within the greater Flint community, her session will address, “The Health Gap: An Exploration of how one hospital is working to bridge the gaps between health care and social care.”
Another perspective will be brought by Leah Corneail, Director of Utilization and Population Health at the Integrated Healthcare Association (IHA). In this role, she is responsible for leading utilization and cost improvement efforts, ensuring success in risk-based contracts and CMS demonstration programs, and collaborating with community partners to improve population health. Corneail has several years of experience in population health and health policy. Prior to joining IHA, she served as a Senior Project Manager in the Michigan Medicine Population Health Office, where she managed Michigan Medicine’s portfolio of value-based payment models and partnered with operations to implement care transformation initiatives. Leah received her Master of Public Health degree from The George Washington University’s Milken Institute School of Public Health. She will speak to, “IHA Efforts to Screen and Address Patient Social Influencers of Health (SIOH).”
Also representing the approach of a PO will be Melissa Gary, Community Liaison with the Great Lakes Physician Organization (GLPO). In this role, Melissa is responsible for bridging the gap between healthcare providers of GLPO and the local community agencies to better align the mission of GLPO. Utilizing her several years of experience in healthcare and nonprofit organizations, she has built the GLPO social determinants of health process. She is a passionate community servant with the ability to motivate and inspire individuals to identify their own potential and shares in the passion to serve others. Melissa is a graduate from Ferris State University where she studied nuclear medicine and healthcare administration. She has minors in science, biology, pre-pharmacy and paralegal.
Attendees can also expect to hear from MVC Coordinating Center leadership and staff about MVC’s Medicaid data, the MVC Component of the Blue Cross Blue Shield of Michigan (BCBSM) Pay-for-Performance (P4P) Program, and general program updates.
These presentations could be informative and useful for any of the following stakeholders who are welcome to attend:
- MVC Hospital Site Coordinators and Champions
- MVC Physician Organization Site Coordinators
- Quality Leadership
- Clinicians
- Managers and front-line staff in the following clinical areas:
- Population health
- Chronic disease management
- Post-acute care
- Value-based care
- Care coordination
- Discharge planning
- Social work
- Others whose work addresses health equity or social risk factors
In addition, hospitals that have attended both of MVC's 2021 Semi-Annual Events (May 2021 and October 2021) will be eligible for one additional bonus point toward Program Year 2021 of the MVC Component of the BCBSM P4P Program.
Those interested in attending this informative and collaborative meeting should register here. The MVC Coordinating Center looks forward to a fantastic meeting. See you there!
Staffing Shortage Challenges Hospitals Across Michigan
The past 18 months of the pandemic forced healthcare to be creative and responsive to the needs of the moment, and in that time the MVC Coordinating Center heard from members about how they are working to maintain a high quality of care. The challenges and pivots shared by members vary significantly because facilities were impacted at different points in time and with varying levels of severity. However, one challenge echoes loudly and consistently for hospitals big, small, urban, or rural: the staffing shortage. This problem isn’t specific to Michigan. Across the United States, hospitals don’t have enough staff to keep up with their normal standards of care, with many having to turn away patients and ration care.
Health professionals are the lifeblood of healthcare delivery, so attaining or maintaining a high quality of care is only achievable with appropriate staffing levels. The Institute of Medicine framework defines quality care with six aims: that it be safe, effective, patient-centered, timely, efficient, and equitable. Some of those aims have been directly exacerbated by the pandemic—such as health equity or safety—while many have been at least indirectly impeded by the strains on frontline workers.
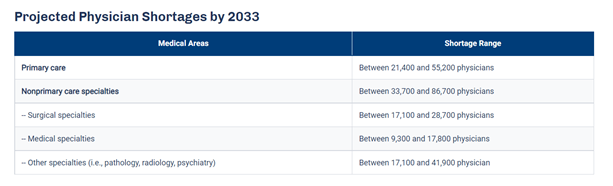
An article published by the Detroit Free Press this month titled, “Michigan hospital staffing shortage nears crisis point as COVID-19 patients rise,” paints the current situation as dire. The article quotes Brian Peters, the CEO of the Michigan Health & Hospital Association, as saying, “I have never heard a consistent theme from across our entire membership like I have on this staffing issue." He adds that the shortage affects multiple sectors of the workforce, such as nurses, physicians, housekeeping, technicians, and food service personnel. These new staffing issues occur within an industry that was already concerned about an expected shortage of primary care physicians (PCPs). The Association of American Medical Colleges (AAMC) published data that predicts an estimated shortage of between 21,400 and 55,200 PCPs by 2033 (see Figure 1), in part due to a population that continues to grow and age.
Figure 1.
Some hospitals suggest burnout as the main culprit for the current staffing shortages. A literature review on the effect of burnout on quality of care defines burnout as a state of fatigue and frustration manifested as physical and emotional exhaustion characterized by dissatisfaction and stress, with symptoms such as, “physical fatigue, cognitive weariness, and emotional exhaustion.” Anyone in that condition cannot perform at their best. So as quality teams try to find treatment efficiencies for conditions such as chronic obstructive pulmonary disease (COPD) or congestive heart failure (CHF), the elephant in the room is that they may not be able to provide treatment if nurses, technicians, and physicians aren’t adequately staffed.
The industry is expecting the shortages to increase slightly in the coming weeks as vaccination mandate deadlines approach. Currently, those health systems requiring COVID-19 vaccination include Henry Ford, Michigan Medicine, Beaumont Health, Trinity Health, Spectrum Health, OSF HealthCare, Ascension Health, and Bronson Healthcare, along with Veterans Health Administration facilities.
A variety of strategies are being proposed to lessen the burden felt by the shortage. Since it takes time to recruit new people into medical fields, these approaches generally fall into one of two categories: 1) retain current staff, and 2) deploy current staff as efficiently as possible.
The approaches that hospitals have mentioned for retaining staff are short-term in nature, ranging from approval of overtime and bonuses to instituting new staff well-being programs and sharing mental health resources. Efficient staffing is a more complex approach, but long-term with the potential to reduce the expected burden from future PCP shortages. The Harvard Business Review published an article that outlines strategies for efficient staffing in response to the PCP shortage, which could be repurposed and applied to other healthcare workforces. Among their suggestions, they highlight Advisory Board research that proposes the threefold answer is, “better use of PCPs targeted at specific populations, greater use of non-physician labor where appropriate, and much broader deployment of technology to increase access to primary care.” These suggestions align with several other priorities often voiced to the MVC Coordinating Center by members, including equitable access to care, expanded telehealth offerings, and improved care coordination utilizing nurse practitioners and physician assistants.
The work ahead will be challenging, as it often is in healthcare. Hospitals will continue to shoulder a shared burden in the months ahead. MVC encourages all members and partners to share resources that may help a peer institution improve the quality of care for Michigan residents. Please continue to bring these ideas to future workgroups and networking events, and contact the MVC Coordinating Center at michiganvaluecollaborative@gmail.com.
Approach to quality improvement unique for rural hospitals
Quality improvement is a key effort for healthcare systems and a driving force behind the work of the Michigan Value Collaborative. It is also an increasingly complex task with significant implications. Not surprisingly, quality improvement is not a one-size-fits-all approach, with the challenges impacting hospitals varying significantly by factors such as size and location. This variability showcases the importance of sharing tailored resources among Collaborative members.
Critical-access hospitals (CAHs) are the newest type of members to join the Collaborative. They play an important role in the healthcare system by caring for rural patients who might not otherwise have access to inpatient services. Defined as hospitals maintaining no more than 25 acute care beds and located more than 35 miles from the nearest hospital, they are unique in their populations, services, and structure. The majority of their patients would have to drive 30 minutes or more for an alternative hospital, and many communities have no alternative. Their offerings and size are reflective of the communities they serve, with services such as emergency care, inpatient care, laboratory testing, rehabilitation, long-term care, maternity care, home health care, and even primary care. As a result, their capacities, priorities, and challenges differ from those of their larger colleagues, as do their quality improvement efforts.
For example, a 2015 report from the National Quality Forum titled, “Performance Measurement for Rural Low-Volume Providers,” highlights several challenges to quality improvement in rural areas including fewer providers, lack of information technology, and fewer people to share the workload. Furthermore, rural hospitals often don't meet patient volume thresholds that are required for meaningful comparative analyses. It is critical, therefore, that CAH facilities are connected to resources tailored to their circumstances. One such resource is the 2021 Small Rural Hospital Blueprint for Performance Excellence and Value, produced by the National Rural Health Resource Center.
The purpose of this Blueprint is to aid rural hospital leaders in taking a comprehensive systems approach to quality improvement using factors and strategies relevant to small rural hospitals. Guided by the components of the Baldrige Framework that first took hold in healthcare over 20 years ago, the Blueprint outlines typical challenges, factors for success, and relevant resources for seven key inter-linked focus areas (see Figure 1): leadership; strategic planning; patients, partners, and communities; measurement, feedback, and knowledge management; workforce and culture; operations and processes; and impact and outcomes.
Figure 1.
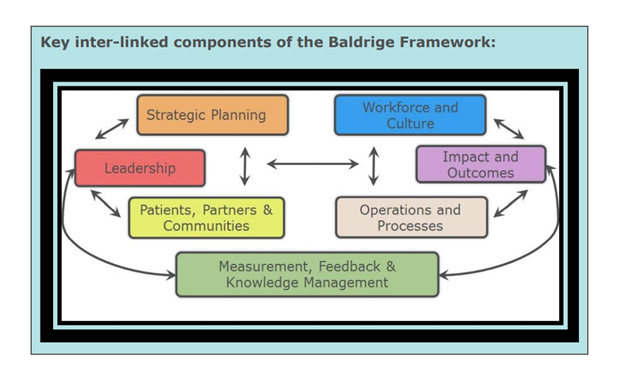
The Blueprint also incorporates specific comments and feedback shared during the Small Rural Hospital Performance Excellence Summit that was held in the spring of 2021. For instance, within the section on leadership, the Blueprint suggests that educating and engaging the CAH’s board members on healthcare trends and issues is a critical factor of success, in large part because board members in rural areas often do not have a healthcare background. A quote from the Summit on this issue reads, “changes in healthcare are complicated, particularly for those that don’t spend all day every day focused on it.” The Blueprint then recommends resources listed in its appendix that are specifically designed for engaging CAH board members. In addition, a full companion resource focused on related strategies and resources for state flex programs is also available.
CAHs are an important piece of the healthcare puzzle and, like their larger colleagues, they stand to benefit significantly from quality improvement efforts. In fact, an October 2019 CMS fact sheet, “CMS Hospital Value-Based Purchasing Program Results for Fiscal Year 2020,” looked at adjustments made for Medicare payments to hospitals based on their performance on a set of quality measures. Compared to urban hospitals, rural and smaller hospitals generally performed better in both efficiency and cost reduction, among other areas.
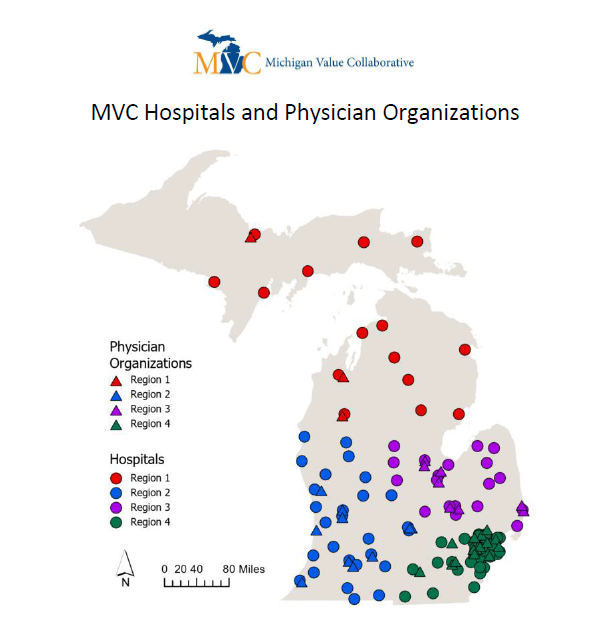
The MVC Coordinating Center established regions within its membership in order to help hospitals network and share practices with their peers. Many of the CAH members within the Collaborative operate in region 1 in the northern parts of the state, and a regional networking event was held for region 1 earlier this week. The Coordinating Center is proud of its diverse membership and continues to encourage facilities and POs to leverage the knowledge of peers who operate in a similar capacity so that, together, members can improve the value of healthcare for Michigan patients. If your facility or PO is utilizing a resource that would benefit the work of a peer institution, please contact the Coordinating Center at michiganvaluecollaborative@gmail.com so it may be shared with the Collaborative.
Joint, CHF Top Members’ Selections for MVC P4P Program
The MVC Coordinating Center recently distributed condition selection reports for Program Years 2022 and 2023 of the MVC Component of the Blue Cross Blue Shield of Michigan (BCBSM) Pay-for-Performance (P4P) Program. The reports were provided in conjunction with details pertaining to the condition selection process, as well as changes to the scoring methodology, cohort assignments, and bonus points available. More details about those changes was published in a previous MVC Coordinating Center blog.
Eligible members were tasked with reviewing these reports and returning their condition selection form at the end of August. Each participating hospital selected two of the seven available conditions for PY22 and PY23: spine surgery, joint replacement, chronic obstructive pulmonary disease (COPD), coronary artery bypass grafting (CABG), congestive heart failure (CHF), colectomy (non-cancer), and pneumonia. The condition that was selected by the most participants was joint replacement with 41 hospitals selecting it, followed closely by CHF with 40 selections. COPD was selected by 32 hospitals. See Figure 1 for a depiction of the total selections for each condition.
Figure 1.
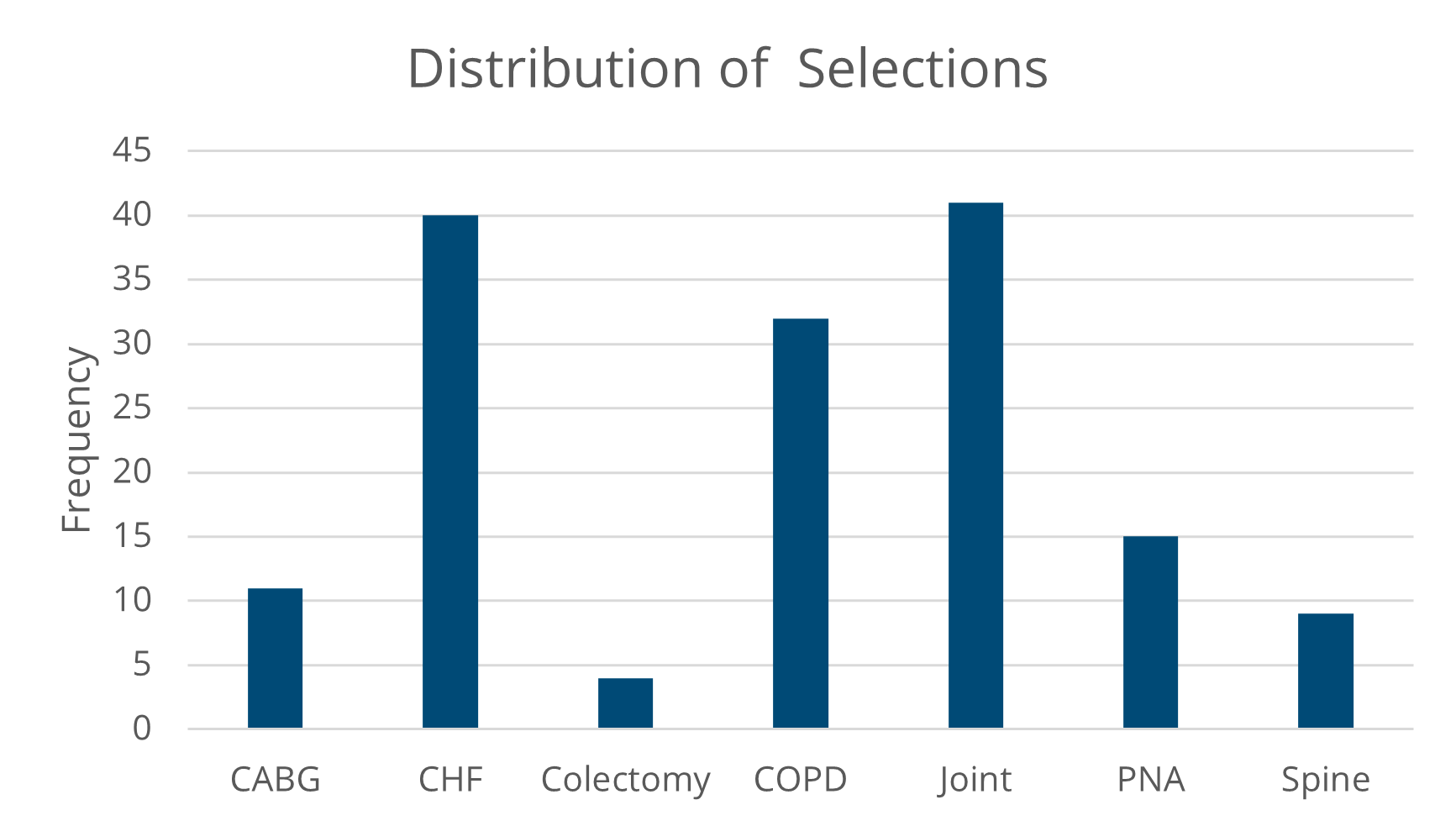
Although the two conditions selected most frequently were consistent across a variety of hospitals, the overall selections varied somewhat from region to region and by hospital size or type. For instance, hospitals with fewer than 100 beds were much more likely to select pneumonia as one of their two conditions than peers with more than 100 hospital beds (see Figure 2).
Figure 2.
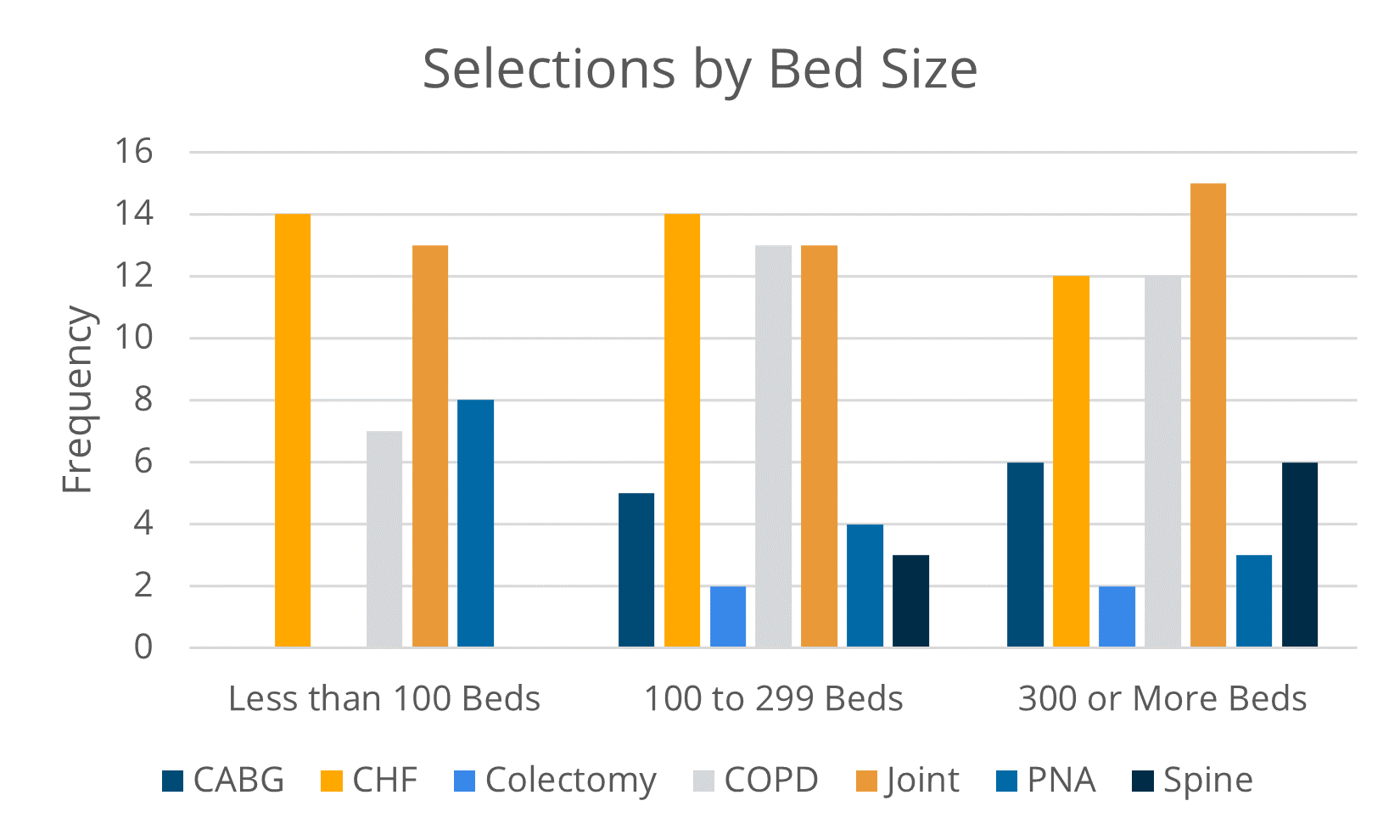
Conversely, larger hospitals that perform more complex procedures made up the totality of selections for spinal surgery, colectomy, and CABG. Still, joint replacement and CHF were the most commonly selected conditions among all hospital sizes.
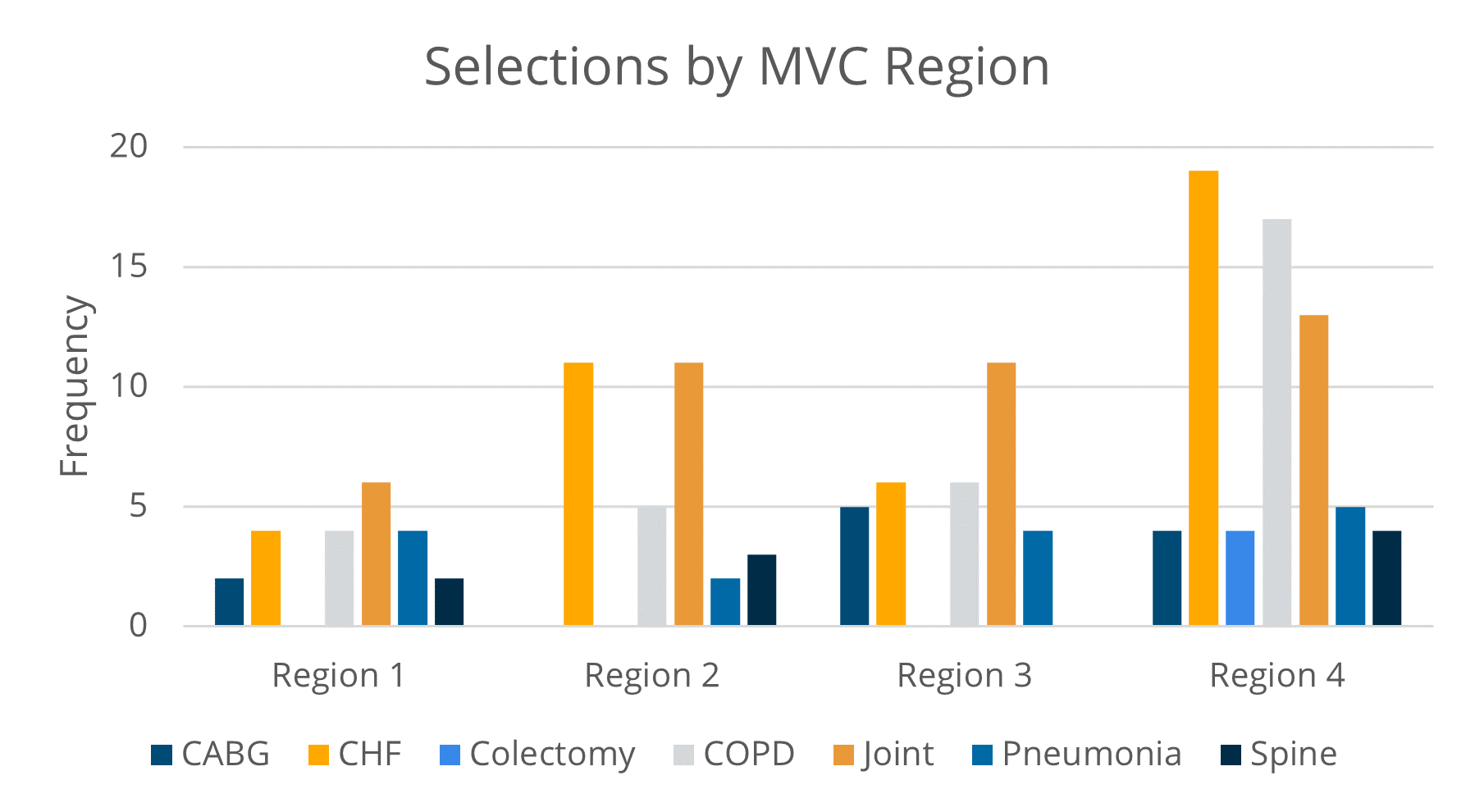
Similarly, CHF and joint replacement were popular among all hospitals regardless of location type, such as urban or rural (see Figure 3), or location within the state (see Figure 4), with the exception of Region 4 hospitals selecting COPD more frequently than joint replacement.
Figure 3.
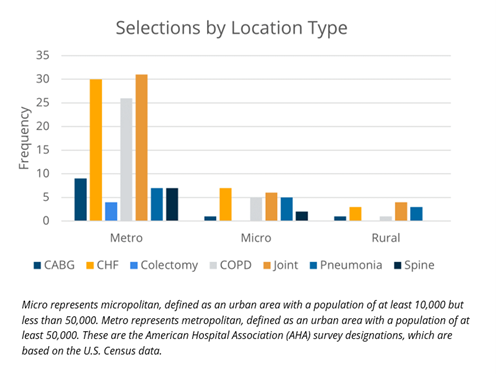
Figure 4.
With the majority of hospitals focusing on both joint replacement and CHF, the MVC Coordinating Center hopes that continued participation at the joint and CHF workgroups will result in meaningful collaboration among members. MVC will also continue to offer events for virtual networking with facilities and physician organizations (POs) within a member’s geographic region (see Figure 5). These regional networking events provide additional opportunities to connect and share knowledge with peers who may share your hospital’s priorities. For instance, the next Coffee, Chat, and Collaborate virtual networking event takes place among hospitals and POs in Region 1 on Monday, September 13, at noon. Members from Region 1 interested in attending can register here.
Figure 5.
P4P cohorts were reassigned for PY22 and PY23. These changes were also detailed in the new technical document, and the new cohort assignments were published on the MVC website. The cohorts were not intended to group hospitals that are exactly alike; rather, they created a reasonably comparable grouping from which MVC can complete statistical analyses.
This program began in 2018, when BCBSM allocated 10% of its P4P program to an episode of care spending metric based on MVC data. This metric measures hospital performance using price-standardized, risk-adjusted 30-day episode payments for BCBSM Preferred Provider Organization (PPO), Medicare Fee-for-Service (FFS), BCBSM Medicare Advantage, Blue Care Network (BCN) Health Maintenance Organization (HMO), and BCN Medicare Advantage.
If you would like to receive notices about the MVC workgroups or have questions about any aspect of the MVC Component of the BCBSM P4P Program, please contact the MVC Coordinating Center at michiganvaluecollaborative@gmail.com.
Predictive Analytics Assist with Chronic Disease Prevention
The healthcare system has an immense wealth of information at its digital fingertips. Big data is constantly expanding from sources such as digitized patient records, patient wearables, medical apps, genome datasets, monitoring devices, and more. A critical challenge facing hospitals and health systems today is in effectively identifying strategies and personnel to utilize big data in a way that influences clinical care. Those that succeed in this task will find themselves in a much better position to advance care and improve patient outcomes.
One developing strategy to convert big data sets into improved patient outcomes is the use of predictive analytics, an approach that differs from what many hospital quality improvement departments are currently utilizing. For example, the Michigan Value Collaborative (MVC) Coordinating Center has been helping hospitals identify opportunities for quality improvement since 2013 by aggregating and analyzing payor claims data and presenting the results on the registry and in analytics reports. The goal of these efforts is to help hospitals compare utilization against peers and draw important insights across a range of medical and surgical procedures. This retrospective approach helps MVC members to learn from their past performance in order to pursue meaningful, observable improvements within their buildings. It is one piece of the big data puzzle. Predictive analytics, on the other hand, allows clinicians to utilize big data before their patient experiences significant healthcare services or treatments. As its name denotes, this approach identifies prevention opportunities before the incidence of disease by predicting a patient’s risk. This is especially important for diseases that require early detection for optimal treatment and survival.
Unlike Robotic Process Automation (RPA), which is also on the rise in health systems across the country, predictive analytics is performed by Artificial Intelligence (AI). This means that computer systems will perform tasks typically requiring human intelligence, including analyses and decision-making. In some ways, this strategy mimics what physicians have long been doing at a patient’s bedside: collecting a patient’s medical history and risk factors in order to tailor their treatment and advice. This process is essential in evaluating a patient’s risk of developing chronic diseases, which often run in their family or are more likely due to socioeconomic factors. An article from the University of Illinois Chicago posits that predictive analytics represent a significant potential for cost savings if they help clinicians and their patients prevent the onset of chronic diseases, one of healthcare’s costliest areas.
“On a population-wide level, predictive analytics can help greatly cut costs by predicting which patients are at higher risk for disease and arrange early intervention, before problems develop,” the article stated. “This involves aggregating data that are related to a variety of factors. These include medical history, demographic or socioeconomic profile, and comorbidities.”
The Centers for Disease Control and Prevention (CDC) states that, “90% of the nation’s $3.8 trillion in annual health care expenditures are for people with chronic and mental health conditions.” So the potential cost savings from reducing chronic disease treatment are significant.
Using predictive analytics in a clinical setting can leverage both patient records and socioeconomic factors. Medical records will often include family history of chronic diseases such as cancer, diabetes, and heart disease, which would make a patient more likely to develop the condition themselves. In addition to family history, a patient’s socioeconomic factors (e.g., education, employment, and environment) and lifestyle choices are significant predictors of chronic disease. A study in the American Journal of Preventive Medicine outlines how researchers used predictive analytics to screen for cardiovascular disease risk from social determinants of health, and ultimately guide clinician treatment options. The researchers also suggest that large databases about social determinants of health variables, especially environmental ones, are not as readily available as they should be, and are an important area of opportunity for future data collection efforts.
A similar application of this technology was used in a study published by Cancer Immunology Research to predict lung cancer immunotherapy success. In the study, researchers used an AI algorithm to identify changes in patterns from CT scans that were previously not detected by clinicians, which ultimately predicted how well a patient would respond to immunotherapy. This suggests that predictive analytics can help improve the accuracy of diagnoses and treatment.
Of course, the applications for predictive analytics extend beyond chronic disease prevention and treatment. In the past year, researchers have also used predictive analytics to forecast outcomes for patients positive for COVID-19. In The American Journal of Emergency Department Medicine, a published study validated a tool that helps physicians predict adverse events among patients presenting with suspected COVID-19. The study suggests that the algorithm and scores can help physicians decide when to hospitalize or discharge patients during the pandemic. Therefore, predictive analytics appear to also provide insights that enhance treatment.
Many additional articles (such as one article from Health IT Analytics) and published studies recommend predictive analytics for its potential benefits. As with any technology, however, it is not without its risks. The use of AI brings about concerns for privacy, especially since hospitals must properly steward patient data and comply with HIPAA regulations. But there are several other considerations identified in a recent Deloitte analysis (see Figure 1), not the least of which is ensuring the algorithm doesn’t introduce bias that disproportionately harms minorities and communities of color. Predictive analytics may also present evaluation challenges. Once algorithms are validated, their widespread use in clinical settings should be confirmed for their efficacy, which requires measuring the absence of disease.
The potential benefits of predictive analytics are variable and significant; however, as healthcare learns to integrate AI technologies, it will be important to keep its risks in mind and address them accordingly. The MVC Coordinating Center endeavors to assist its members through their data analytics journey by providing insights into specific data sets. When pursuing additional technologies or analytic tools, the Coordinating Center encourages members to volunteer as a sounding board and resource for other members. If your hospital or physician organization is currently utilizing AI or considering it with your patient data, we encourage you to reach out so MVC can share your experience with others. You can reach the MVC Coordinating Center at michiganvaluecollaborative@gmail.com.
Subscribe to our blog!
Recent Posts
Categories
- ASCs
- Chronic Disease Management
- Chronic Obstructive Pulmonary Disorder
- Congestive Heart Failure
- Coordinating Center Updates
- CQI Spotlight
- Critical access hospitals
- Current Events
- Diabetes
- Health Equity
- Hysterectomy
- Joint Replacement
- Outcome Variation
- P4P
- POs
- Rural Health
- Sepsis
- Technology
- Uncategorized
- VCCs