This year in the United States, cardiovascular disease will be responsible for one in every four deaths. Despite its prevalence, few cardiac patients eligible for cardiac rehabilitation utilize this life-changing program. In response, the Michigan Value Collaborative (MVC) and the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2) recently established the new Michigan Cardiac Rehab Network (MiCR) to collaborate on efforts that heighten awareness of these programs and support meaningful improvement in Michigan.
Cardiac rehabilitation (CR) is a comprehensive program encompassing supervised exercise, nutrition education, smoking cessation, mental health resources, skills training for heart-healthy lifestyles, and peer support from others who are experiencing a similar life event. It has a Class IA indication for recent cardiac-related events or procedures, meaning there is high-quality evidence that it is beneficial to patients. In fact, individuals who complete the full program of 36 sessions have a 47% lower risk of death and a 31% lower risk of heart attack than those who attend only one session. The evidence is clear that CR extends life and improves quality of life for patients with a recent cardiac-related event or procedure. Unfortunately, only one in three eligible Michiganders participates—a rate well below the Million Hearts nationwide goal of 70% participation.
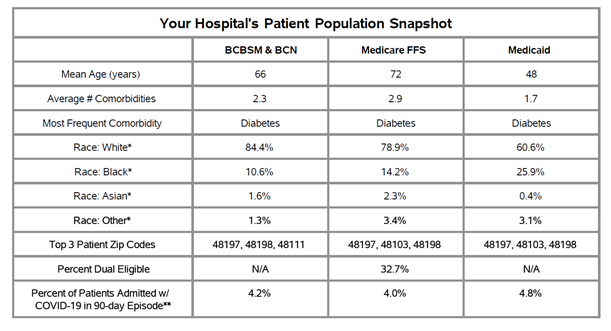
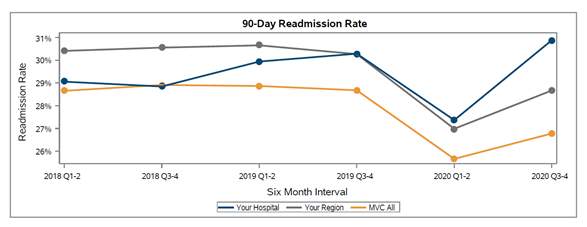
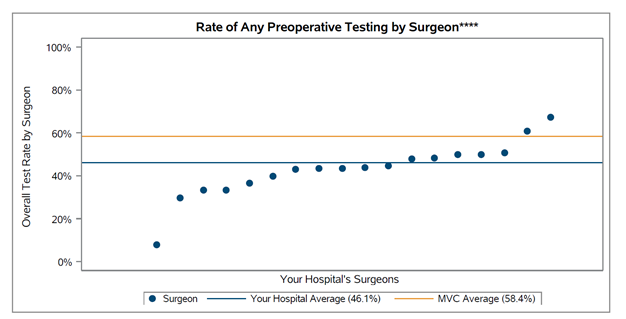
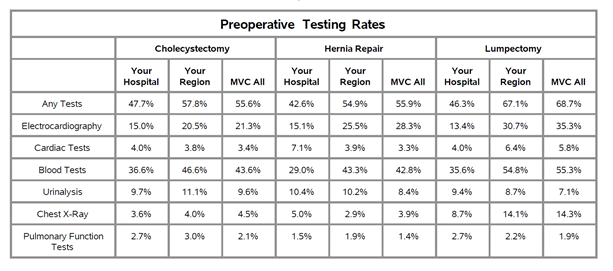
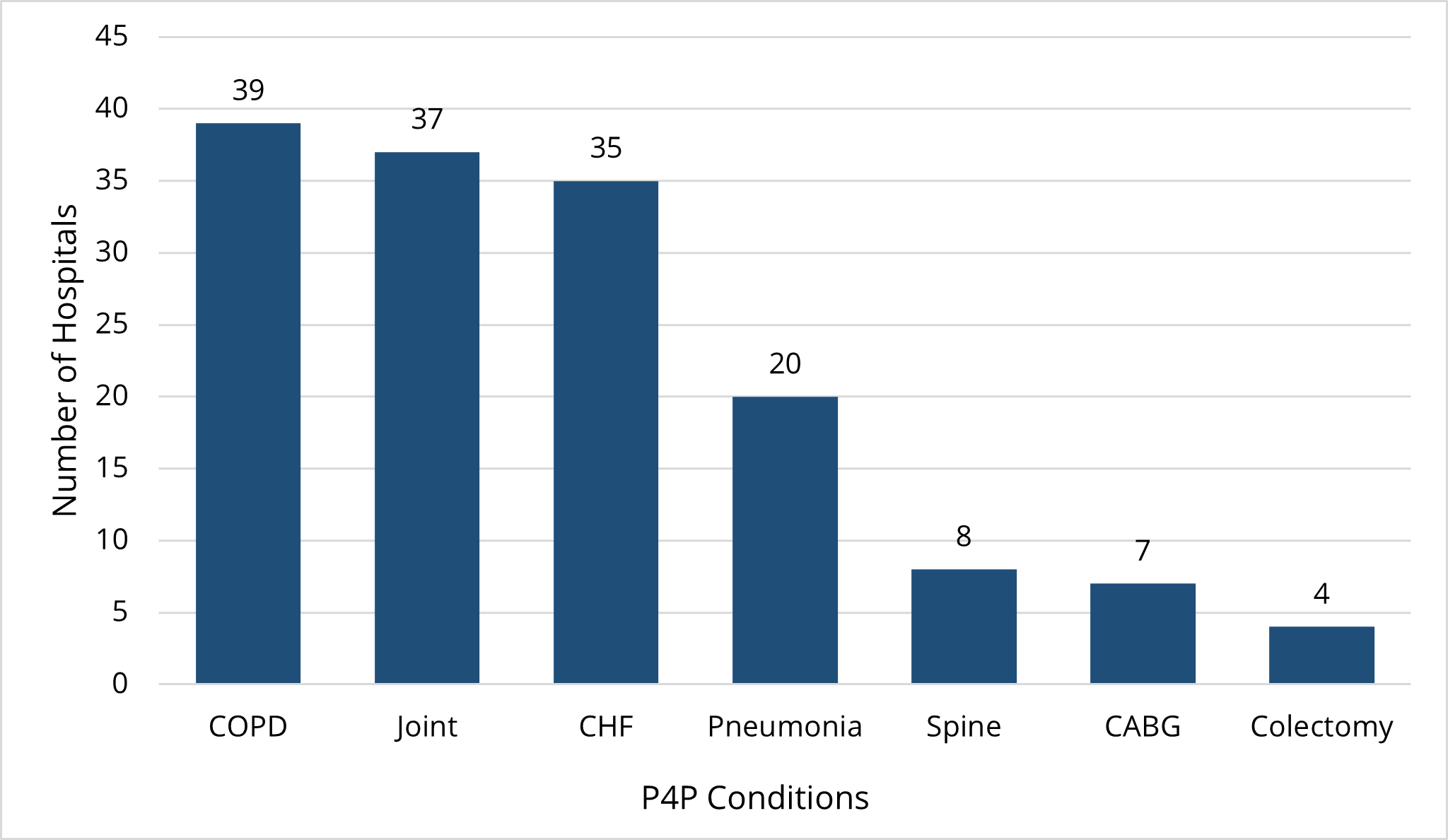
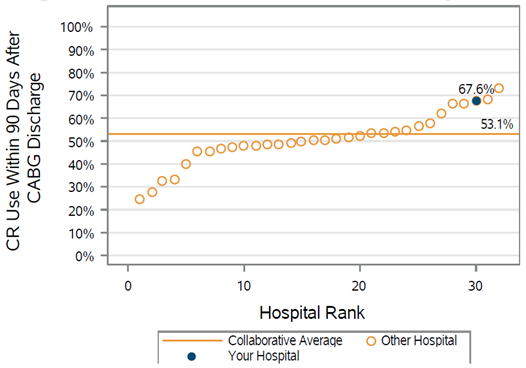
Using claims data, MVC can assess both initiation and adherence – whether and when someone starts CR, and how long they keep going. There is wide variability in CR rates between MVC’s member hospitals (see Figure 1 for a sample plot from a recent blinded report). The site with the highest rate of cardiac rehab after coronary artery bypass graft surgery (CABG), for example, succeeds at sending 75% of their CABG patients to CR, while another only sends 28% of their CABG patients. This variation shows that it is possible to reach high CR rates, and hospitals can learn from each other to make improvements that save lives and reduce costs.
Figure 1. Collaborative-Wide CR Use Following CABG Discharge
MiCR was developed for this reason and will work to equitably increase CR participation for all eligible individuals in Michigan. Serving as Co-Directors of MiCR are Mike Thompson, Co-Director of MVC, and Dr. Devraj Sukul, Associate Director of BMC2 PCI. MiCR will distribute regular CR utilization summaries to relevant providers, convene regular meetings with its stakeholder and advisory groups, create resources that help hospitals and CR facilities optimize CR utilization, and continue to leverage the expertise of both CQIs.
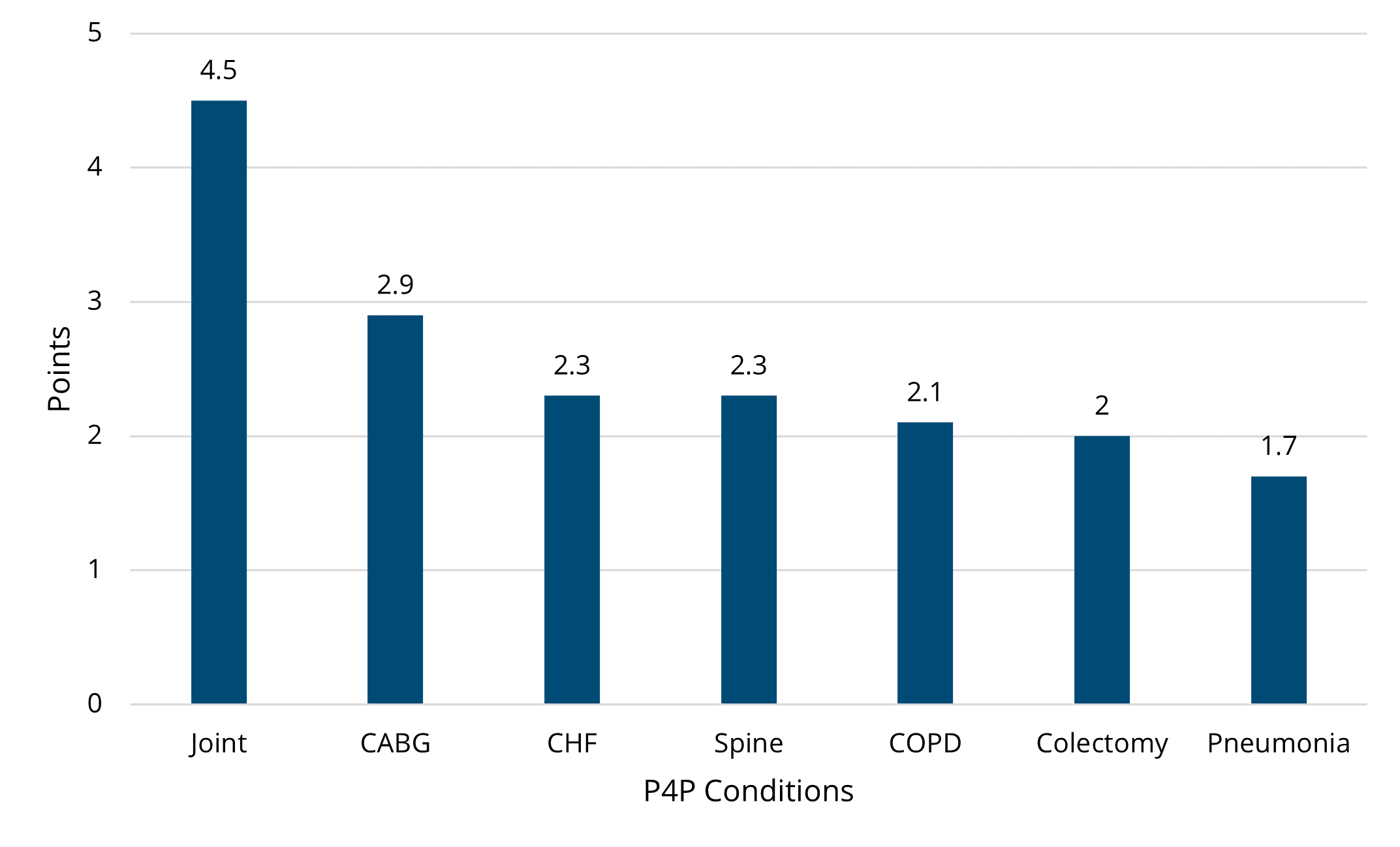
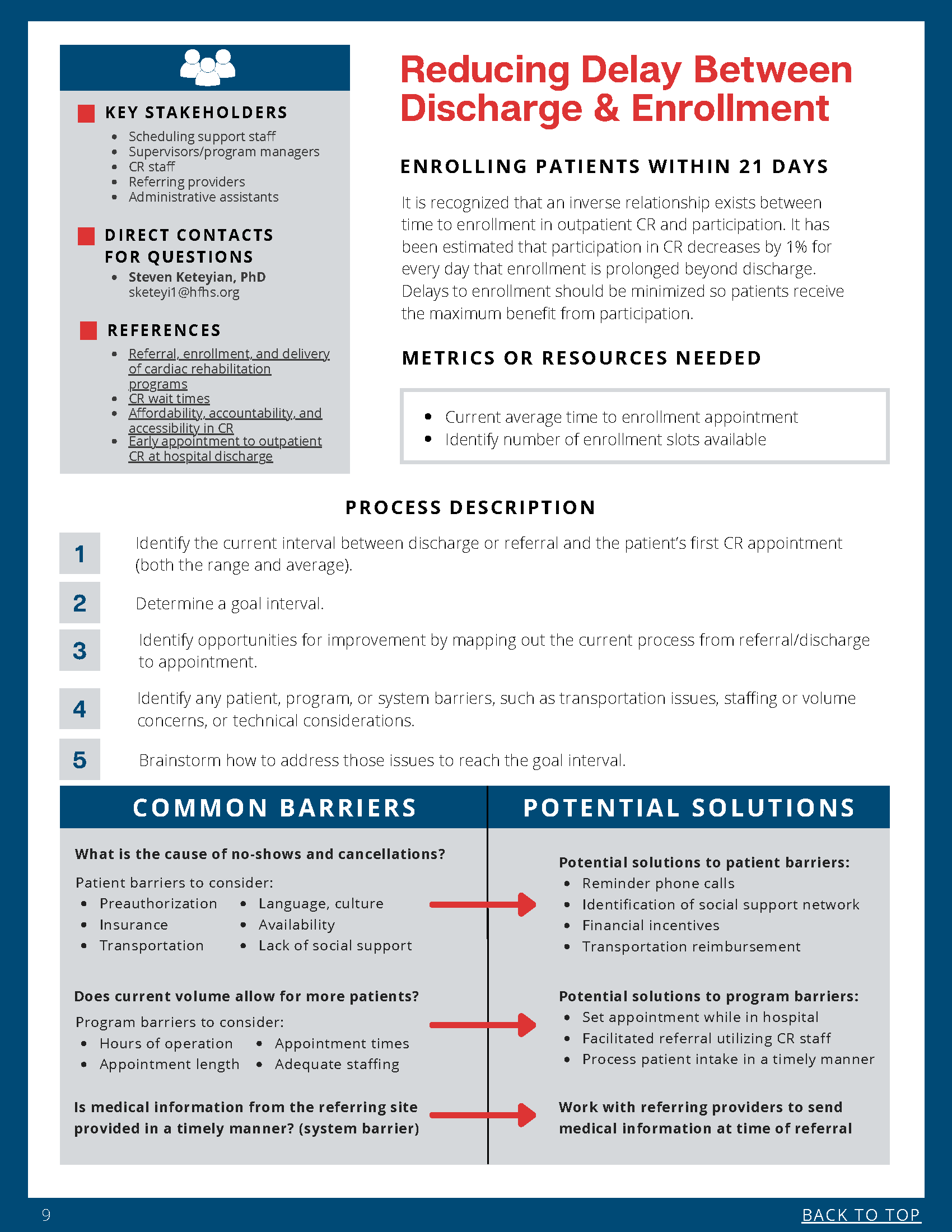
In one of its first coordinated efforts, MiCR worked with CR providers and content experts to create a Cardiac Rehab Best Practices Toolkit, which was launched in April. It outlines initiation, maintenance, and innovation strategies for increasing the utilization of CR (see Figure 2 for a sample page). MVC encourages members to turn to this tool as they work to encourage the enrollment of more patients.
Figure 2. Sample Page from MiCR Best Practices Toolkit
The partner CQIs behind MiCR also released new statewide goals for improved CR utilization. Currently, 30% of patients utilize CR following transcatheter aortic valve replacement (TAVR), surgical aortic valve replacement (SAVR), coronary artery bypass graft surgery (CABG), percutaneous coronary intervention (PCI), and acute myocardial infarction (AMI). The first goal is to reach 40% CR utilization for TAVR, SAVR, CABG, PCI, and AMI patients. In addition, only about 3% of congestive heart failure (CHF) patients currently utilize CR. The second statewide goal is a collaborative-wide utilization rate of 10% for CHF patients. Progress on these goals will be shared by MVC in its CR reports sent every six months.
The two CQIs will also continue with their respective activities in the CR space. MVC supports CR participation in two primary ways. One is providing opportunities for MVC members to collaborate, and the second is the preparation of reports using its unique multi-payer data sources. The MVC team supports collaboration through stakeholder meetings and workgroups, which allow sites and clinicians to share solutions for common challenges. The reports MVC prepares analyze member claims data with time-specific hospital-level information on CR enrollment and completed visits within one year of discharge. This allows hospitals to benchmark their performance against peers and identify areas for improvement. MVC will also share unblinded data on CR rates with members at its May semi-annual meeting in one week, which is meant to drive conversation and encourage best practice sharing across the collaborative. The MVC team hopes that its outreach and resources help members to save lives by providing strong endorsements for CR and addressing barriers that may limit patient participation.
For more information on MVC’s CR efforts, visit MVC’s Value Coalition Campaign webpage. For more information about CR, view this MVC video or visit the Million Hearts website. If you have questions about any of the above activities or resources, reach out to the Coordinating Center at michiganvaluecollaborative@gmail.com.