In 2019, more than 71,000 people died from drug overdoses, making it a leading cause of injury-related death in the United States. Nearly 70% of those overdoses involved a prescription or illicit opioid. The economic cost of the U.S. opioid epidemic was estimated to be $1,021 billion as of 2017 and rising. It is for this reason that clinicians and health systems have adopted evidence-based practices for reducing the number and amount of opioid prescriptions ordered for their patients. It is both clinically and economically significant, then, that the Michigan Value Collaborative (MVC) was recently part of an analysis that estimated over $4.8 million in avoided opioid prescription spending after kidney stone surgery.
MVC identified these savings in partnership with the Michigan Urological Surgery Improvement Collaborative (MUSIC), a physician-led quality improvement collaborative comprised of urology practices across the state of Michigan. MUSIC works to evaluate and improve the quality and cost-efficiency of urologic care. Since 2011, the MUSIC team has led prostate-related quality improvement activities such as improving patterns of care in the radiographic staging of men with newly diagnosed prostate cancer, reducing prostate biopsy-related hospitalizations, and enhancing the appropriateness of treatment decisions. In 2016, MUSIC expanded its scope of work to kidney stone surgery and in 2017 to small renal masses.
With kidney stone incidence on the rise affecting both men and women, MUSIC created a program focused on Reducing Operative Complications from Kidney Stones (ROCKS). It focuses on improving the quality of care for kidney stone patients, particularly by decreasing modifiable emergency department (ED) visits for expected symptoms and side effects of ureteroscopy (URS) or shockwave lithotripsy (SWL) surgeries that are typically avoidable. MUSIC ROCKS aims to minimize these by developing resources that help patients manage their pain and urinary tract symptoms following kidney stone surgery.
Since its formation, the MUSIC ROCKS initiative led to the development of stent omission appropriateness criteria, a URS vs. SWL patient-provider shared decision aid, standardized patient education, and recommendations for postoperative pain control regimens. The ROCKS pain control optimization (POP) guidelines were developed in 2019 and recommended prescribing no opioids following kidney stone surgery. The goal of these guidelines is to minimize opioid use in patients undergoing kidney stone surgery while maintaining patient safety and satisfaction.
The MUSIC Coordinating Center reached out to MVC in 2022 to help assess the impact of its ROCKS initiative on opioid prescription use following surgery. The goal was to estimate MUSIC ROCK's impact on opioid utilization and prescribing rates following URS or SWL kidney surgeries in Michigan, as well as the related impact on the value of care.
METHODOLOGY
Data Sources & Study Population
MVC kidney stone surgery episodes were used for this analysis, which compared outcomes between URS and SWL procedures for MUSIC and non-MUSIC providers. It was restricted to kidney stone surgery claims for Blue Cross Blue Shield of Michigan (BCBSM) and Blue Care Network (BCN) Commercial and Medicare Advantage plans between Jan. 1, 2015 and July 31, 2022. The cohort was further restricted to BCBSM/BCN-insured patients with no opioid prescription fills in the 90 days prior to their surgery who were continuously enrolled in a prescription sub-plan 90 days prior to surgery through 30 days post-surgery. The final cohort used in the opioid analysis included 14,967 Michigan patients.
Methodological Approach
The study population was identified using professional claims for MVC kidney stone surgery episodes that occurred within the index dates of the surgery. All professional claims missing a provider NPI on the claim were excluded. The remaining NPIs were characterized by information derived from the National Plan and Provider Enumeration System (NPPES) data set. Claims of providers or facilities outside of the state of Michigan were also excluded. The remaining NPIs were then categorized into MUSIC and non-MUSIC categories. Opioid utilization was assessed through the presence of paid outpatient opioid prescription claims in the 30 days following surgery.
Limitations
Approximately 90% of Michigan urologists participate in MUSIC. However, only 58% of all MVC kidney stone surgery episodes were identified as being performed by a MUSIC provider via National Provider Identifier (NPI). Some MUSIC providers may be performing these procedures on patients with an insurance plan not reflected in MVC data. It could also be related to MVC's episode structure. Episodes are mutually exclusive; therefore, if a patient were to have a hospitalization prior to their surgery that resulted in an MVC episode creation, their care would not be classified as a kidney stone surgery episode. It is also possible that billing NPI was not always a reliable field.
Second, MVC only has outpatient prescription claims for BCBSM and BCN patients with a prescription sub-plan. For this analysis, only BCBSM-insured patients were assessed. As a result, only about 35% of MVC's URS and SWL episodes were included in assessing opioid utilization. Furthermore, the analysis is of opioid utilization, not provider prescribing patterns. Given that a claim is only generated once a prescription is filled, this analysis cannot provide a full picture of changes in provider prescribing patterns.
FINDINGS & NEXT STEPS
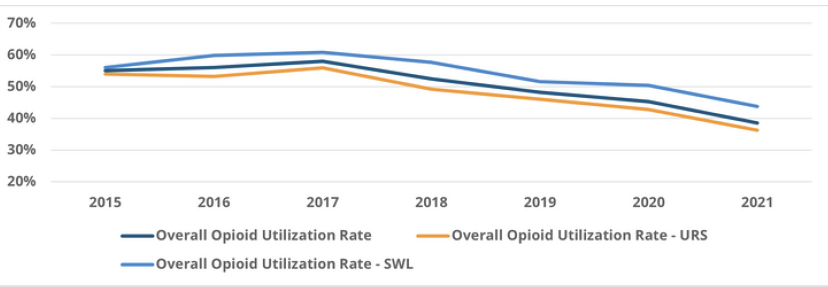
Among the BCBSM/BCN-insured patients who underwent kidney stone surgery between 2015 and 2021, 50.3% of patients on average filled an opioid prescription within 30 days of surgery, with a higher average opioid utilization rate among SWL patients (54.9%) than among URS patients (47.4%). There was a strong decline in opioid utilization after 2017 across Michigan for both types of procedures (Figure 1), with lower utilization following URS.
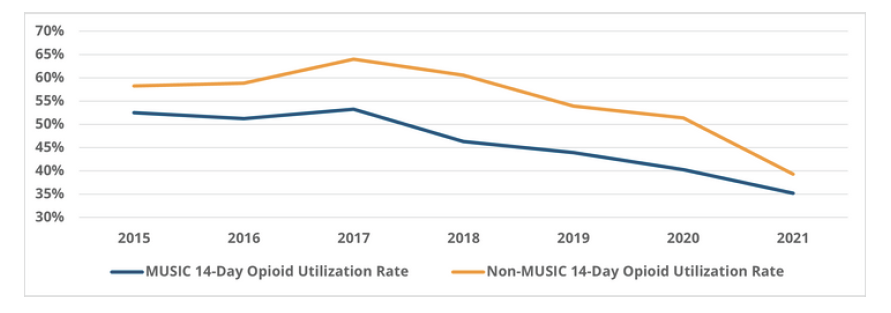
Notably, the rate of opioid utilization after kidney stone surgeries performed by MUSIC providers is consistently lower than those performed by non-MUSIC providers (Figure 2). For example, among URS procedures performed by MUSIC providers after 2016, 43.8% resulted in an opioid fill on average, whereas an average of 53.8% of procedures performed by non-MUSIC providers resulted in an opioid fill. In addition, the absolute decrease in opioid prescription fill rates was greater for MUSIC providers. These trends were similar for SWL surgeries, with consistently lower average opioid utilization rates among patients treated by MUSIC providers (52.1%) vs. non-MUSIC providers (60.9%).
MVC further estimated cost savings from the reduction in opioid prescription fills by examining differences in 365-day prescription payments among the MUSIC cohort. The changes in opioid prescribing resulted in an estimated yearly average savings of $2,712 per patient from reduced opioid prescription fills post-surgery. Using this estimated savings, MVC multiplied the number of URS procedures performed each year by MUSIC providers combined with the yearly percent reduction from baseline in opioid prescribing to further estimate a savings of over $4.8 million from avoided opioid prescription payments since 2016.
The notable decreases in both prescribing rates and prescription payments demonstrate the substantial impact of the MUSIC ROCKS initiative on opioid utilization after kidney stone surgery, including a likely reduction in the total number of filled opioids circulating in the Michigan community as a result of fewer patients receiving prescriptions. MVC completed a similar analysis in partnership with MUSIC looking at prescribing patterns after prostate surgery, and estimated that MUSIC providers helped avert an estimated $1.6 million in avoided opioid prescription spending.
MVC’s expertise and data frequently result in partner projects like this; MVC completed several CQI impact assessments last year, as well as several more so far in 2024. MVC also participates in collaborative activities with peer CQIs through new condition and report development, data analysis and metric consultation, and data matching exercises that pair clinical and claims-based data. To request a copy of any of MVC’s completed CQI impact assessments, please contact the MVC Coordinating Center.