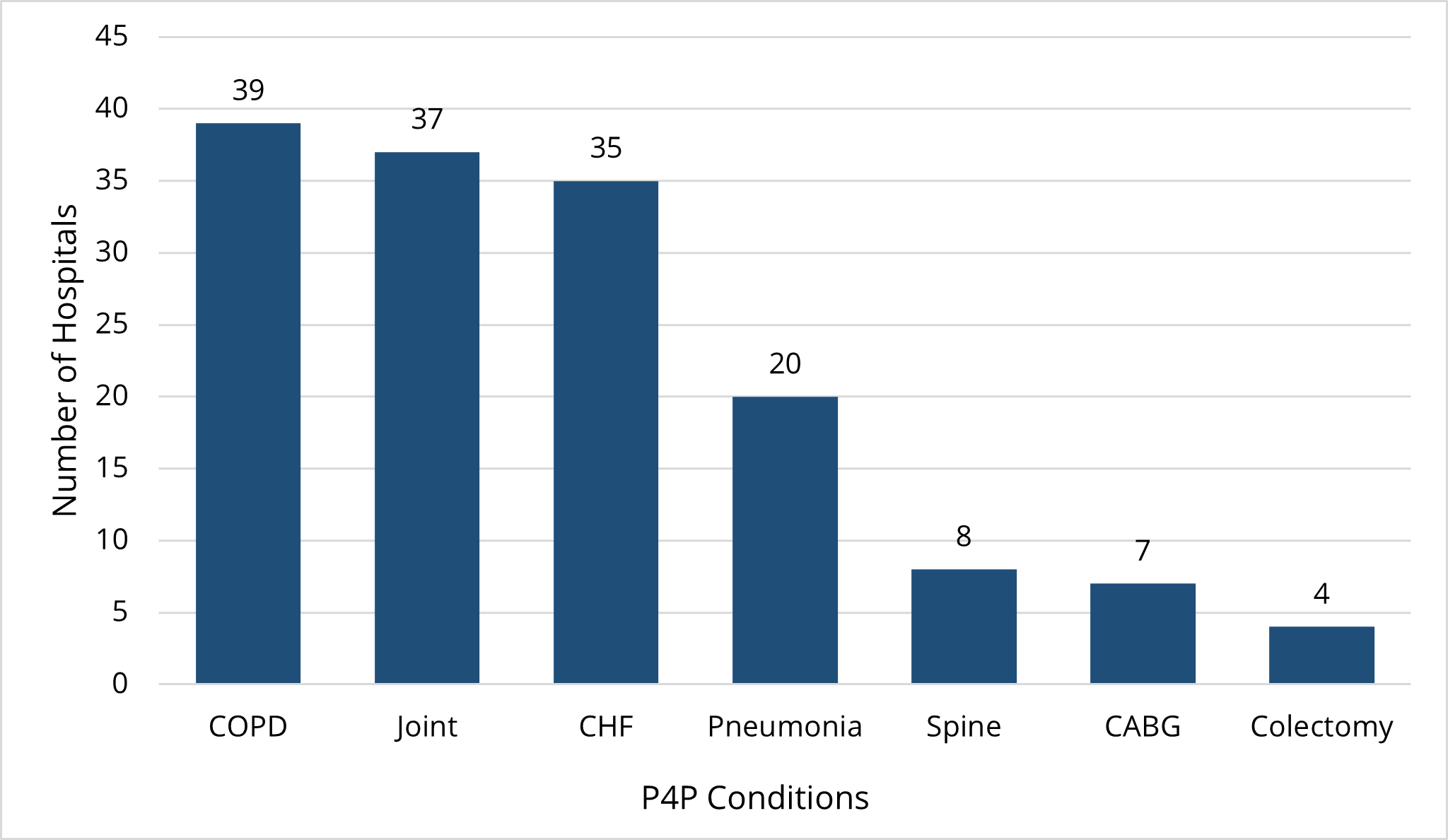
This week the Michigan Value Collaborative (MVC) Coordinating Center distributed the Mid-Year Scorecards for Program Year (PY) 2022 of the MVC Component of the Blue Cross Blue Shield of Michigan (BCBSM) Pay-for-Performance (P4P) Program. These were the first scorecards for the new two-year program cycle for PYs 2022 and 2023.
PY2022 evaluates the index admissions from 2021 as the performance year against admissions in 2019 as the baseline year. MVC is using an improved z-score methodology to calculate both improvement and achievement scores. Hospitals will continue to receive the better of the two scores for each of their two selected conditions. For a description of how the program has changed from the last two-year cycle see the Change Document.
Additionally, this cycle offers hospitals bonus points for completing and submitting a survey for each selected condition by November 1, 2022. These surveys will be used by the MVC Coordinating Center to improve the program for future years and elicit improved best practice sharing between members. The full methodology for the new program can be found in the PY2022-2023 Technical Document.
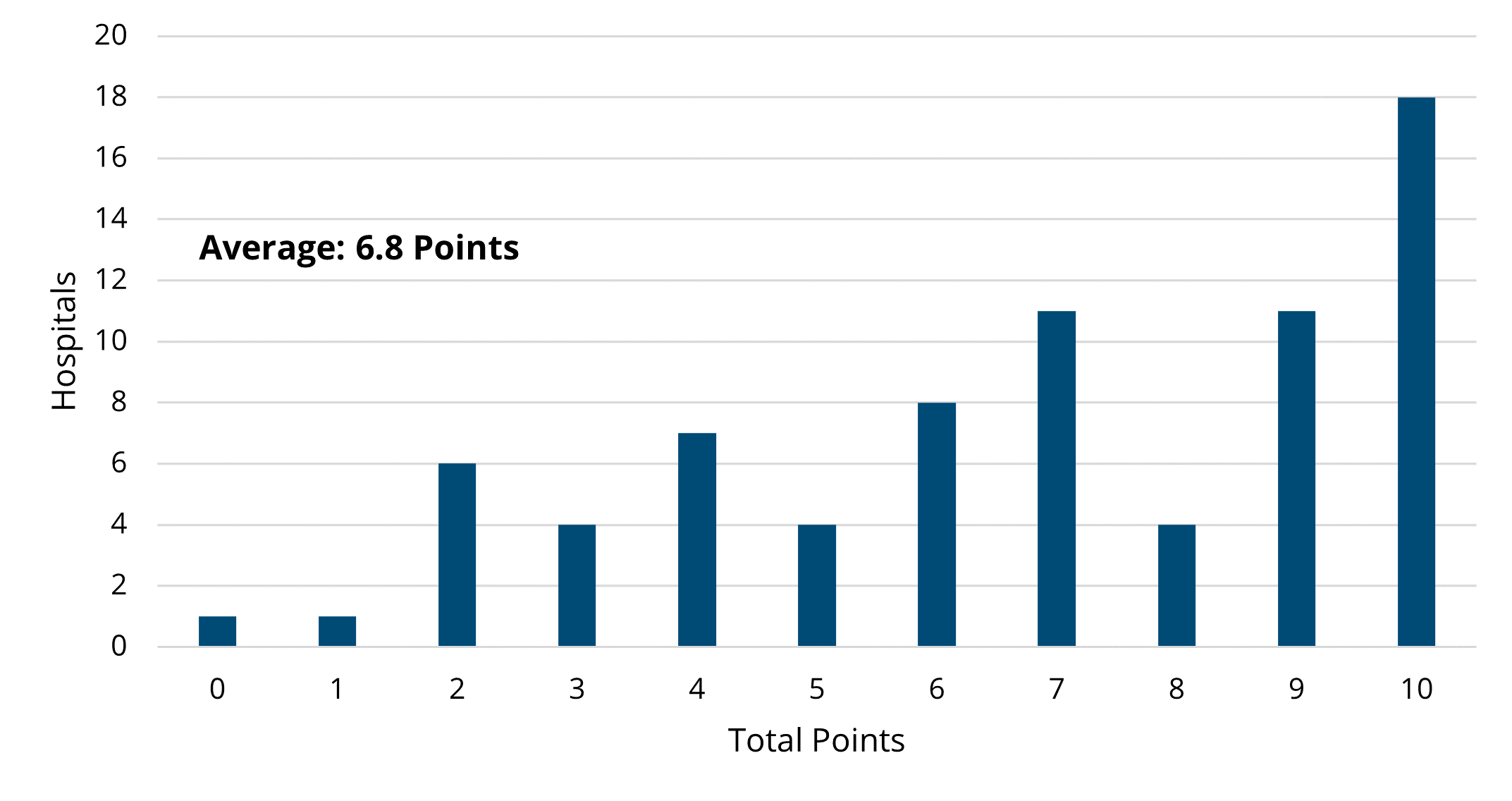
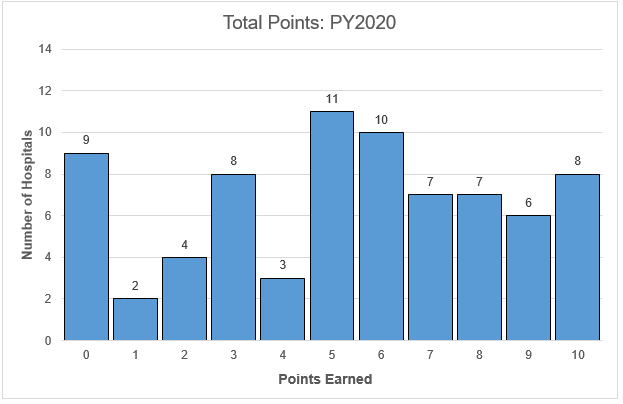
Figure 1 below illustrates the distribution of total hospital points out of 10. The average points scored for the Mid-Year Scorecards was 5.9/10 before including the survey bonus points. This is 0.9 points higher than the average points scored at the conclusion of PY21 excluding all bonus points.
Figure 1.
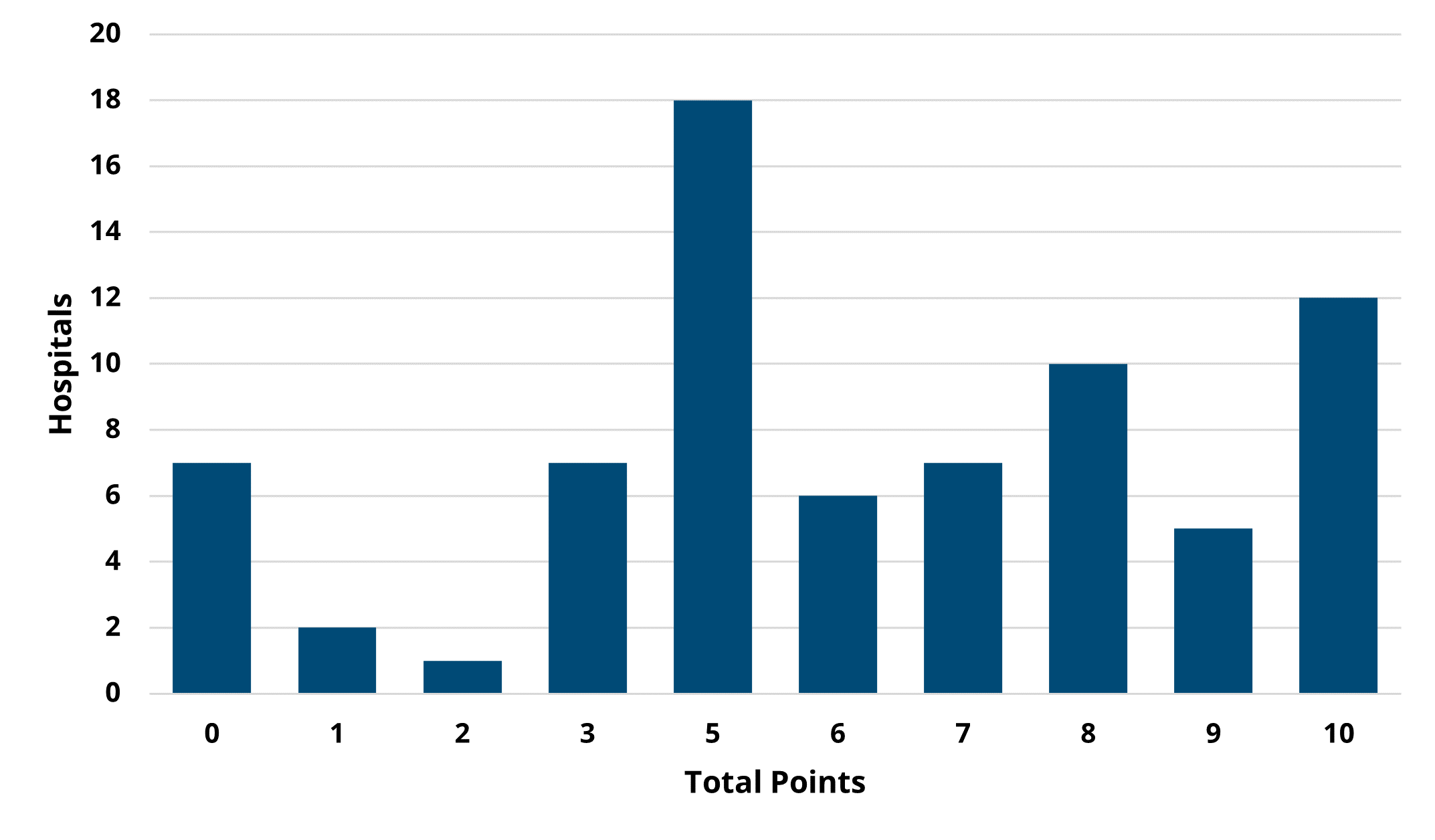
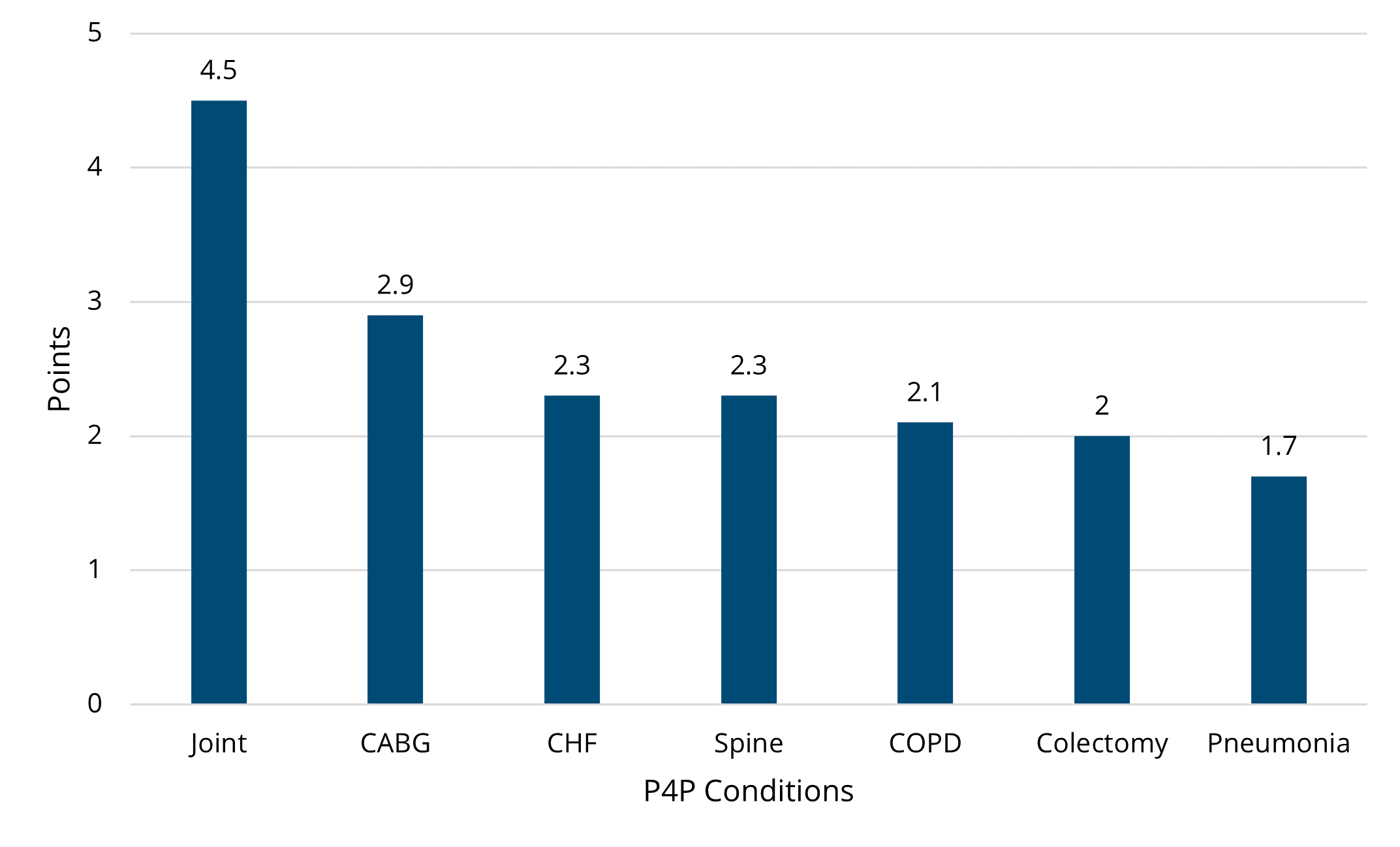
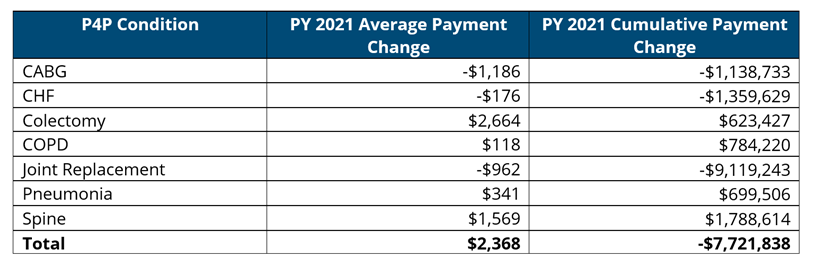
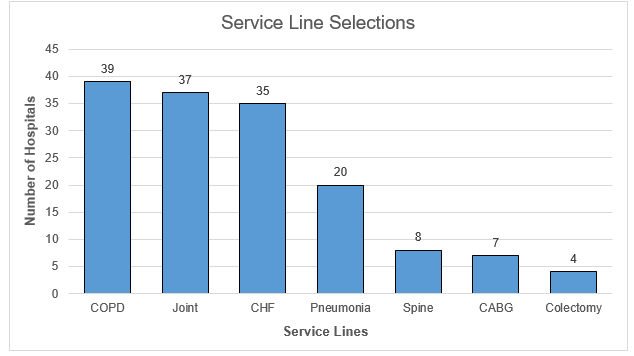
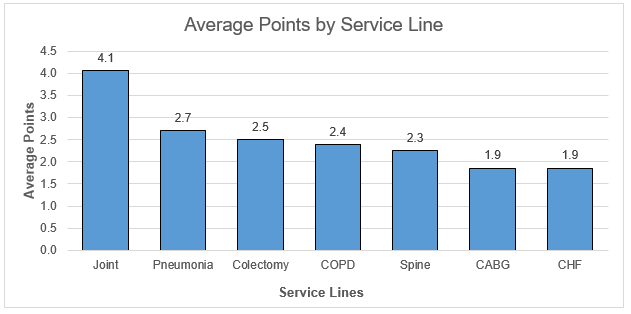
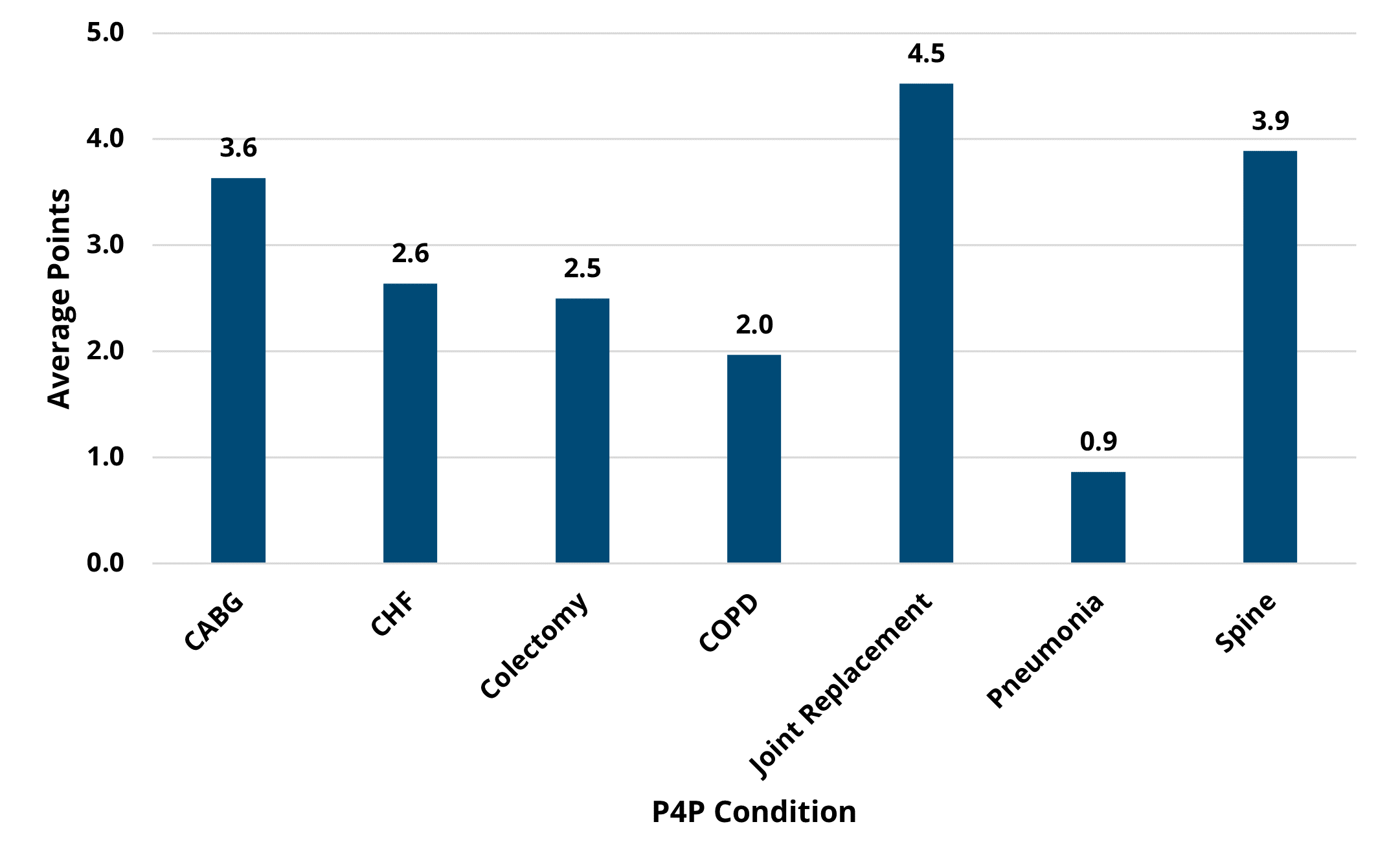
Figure 2 below illustrates the breakdown of average points by condition out of five. Consistent with previous years, joint replacement was the highest scoring condition with an average of 4.5 points earned. The success of the joint replacement condition can be attributed to the shift from post-acute care in skilled nursing facilities (SNF) to home health and the move towards outpatient surgeries. Pneumonia was the lowest scoring condition with hospitals earning less than one point on average. The MVC average payment for a 30-day pneumonia episode increased by $792 from the baseline in 2019 to the performance year in 2021. The largest contributors to this increase were the base payment and readmission payments.
Figure 2.
The Mid-Year P4P scores are subject to change as new data is added. The final scorecards will be distributed after all 2021 claims have been added to the data in quarter one of 2023. Hospitals can track their score through the new P4P PY2022-2023 reports on the MVC registry. These new reports provide all relevant scoring information for both improvement and achievement points in one place except for the survey bonus points. They can be filtered by selected conditions to make the tracking of P4P points easier. For a walkthrough of your hospital’s Mid-Year P4P Scorecard or P4P registry reports, please contact the MVC Coordinating Center.