The Michigan Value Collaborative distributed refreshed push reports this week for its sepsis service line, providing hospital members with updated figures and measures since the last refresh in April.
The version shared with members this week compares MVC hospitals on 90-day risk-adjusted total episode payments, inpatient length of stay, Intensive Care Unit (ICU)/Cardiac Care Unit (CCU) utilization, inpatient mortality and discharge to hospice, 90-day post-acute care utilization, and 90-day readmission rates. Each figure presented reflects 90-day episodes with index admissions from 7/1/18 – 6/30/21 for Medicare Fee-For-Service (FFS), Blue Cross Blue Shield of Michigan (BCBSM) PPO Commercial, Blue Care Network (BCN) Commercial, BCBSM PPO Medicare Advantage (MA), and BCN MA. Most of the measures also include comparison groups for the "MVC All” average across the collaborative as well as the average for each hospital’s assigned geographic region of Michigan.
This week’s reports stratified many measures by BCBSM/BCN Medicare Advantage and traditional Medicare FFS to investigate differences in outcomes and utilization between these two patient groups. MA saw large increases in yearly enrollment over the last decade, resulting in a growing interest in the difference in quality and cost measures compared to traditional Medicare FFS. Recent research suggested that MA patients experience better outcomes and cost less. This held true for some of the measures in MVC’s latest report. Despite the fact that the MA population is older (77 years) than the Medicare FFS population (72 years), the 90-day readmission rate (see Figure 1) among Medicare FFS sepsis patients was higher (33%) than that of MA sepsis patients (27%).
Figure 1.
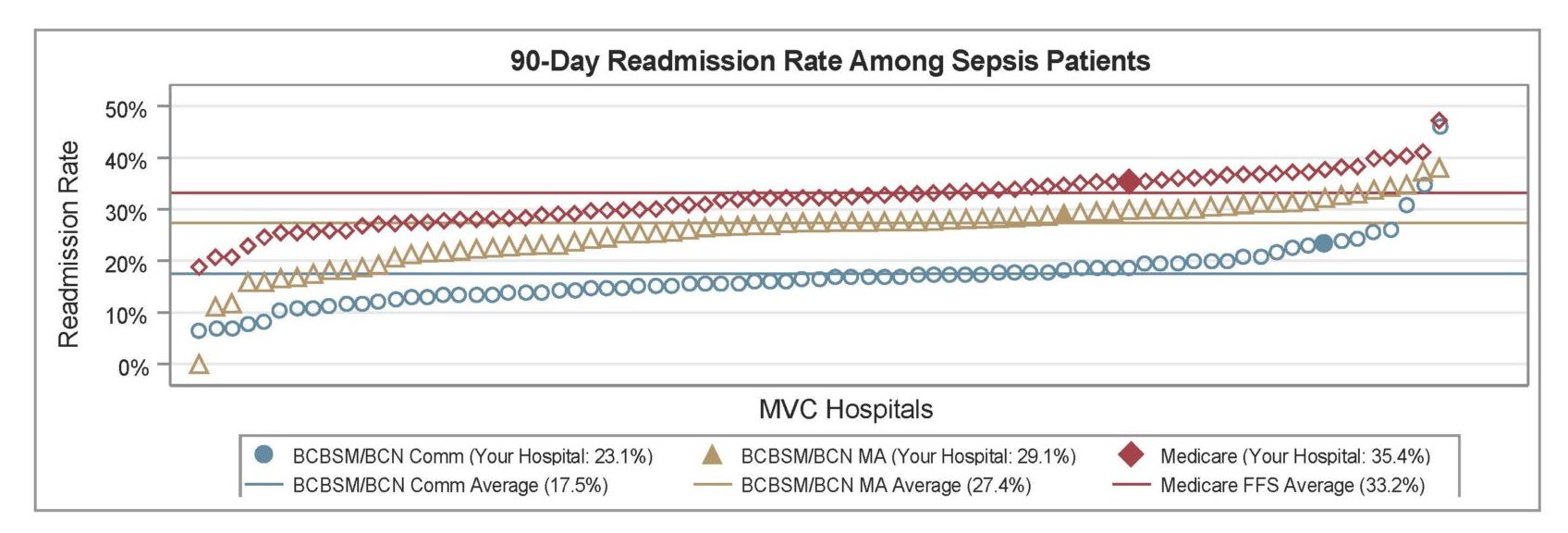
Other noticeable differences between the patient populations included disease burden and social barriers. The Medicare FFS population had a greater comorbidity burden than the MA population; 57% of MA patients had three or more comorbidities whereas 61% of the Medicare FFS population had three or more comorbidities. The Medicare FFS population was also more likely to reside in an at-risk or distressed Zip code according to the Distressed Communities Index (37% vs. 31%).
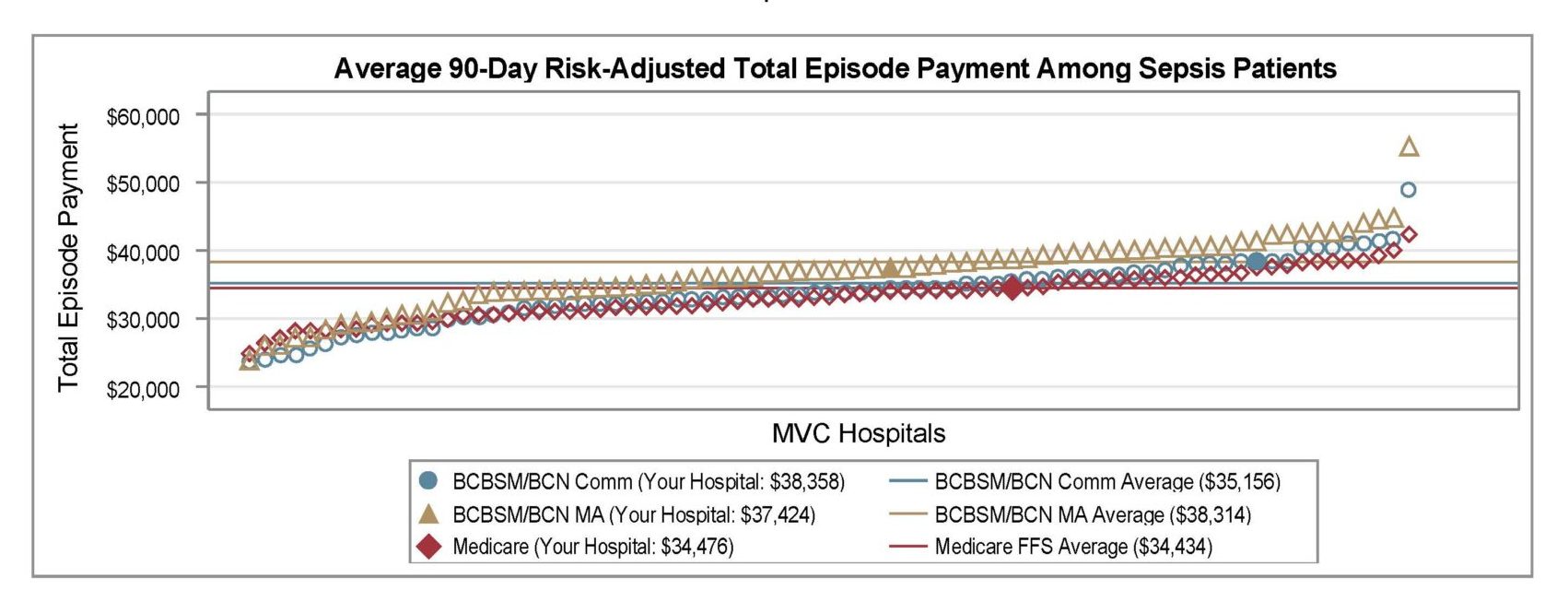
Interestingly, the average 90-day risk-adjusted total episode spending payment among sepsis patients was higher for MA ($38,314) than Medicare FFS ($34,434) (see Figure 2). However, the claims data used in MVC’s report were both price standardized and risk adjusted, so dollars are actually a proxy for healthcare utilization. When taking into account patient factors and payer, BCBSM/BCN MA sepsis patients used more resources than Medicare FFS sepsis patients. Without taking patient factors and payer into account, Medicare FFS sepsis patients used more resources than BCBSM/BCN MA sepsis patients.
Figure 2.
Hospitals can learn more about the differing demographics of these two populations and their BCBSM/BCN commercial counterparts in their patient population snapshot table, a figure that was carried forward from the April reports. The latest reports included additional rows for the rate of septic shock and for the percentage of patients living in an “at-risk” or “distressed” Zip code. The latter is determined by the Economic Innovation Group’s Distressed Communities Index (DCI) data set, which incorporates economic indicators such as education, employment, and income to categorize patient Zip codes as prosperous, comfortable, mid-tier, at-risk, or distressed. The population snapshot table was intended to help hospitals better understand their sepsis patient population. The other demographics included were race, mean age, top three patient Zip codes, the most frequent and average number of comorbidities, and the proportion of patients with a confirmed diagnosis of COVID-19.
The inclusion of COVID-positive patient percentages is an important statistic in the patient population snapshot table since the report included COVID patients. Knowing this percentage could help hospitals understand the extent to which their data is driven (or not) by patients with a confirmed COVID-19 diagnosis.
The latest sepsis reports were also distributed to members of the Michigan Hospital Medicine Safety Consortium (HMS), which partnered with MVC on the original development of this service line for MVC’s registry. MVC plans to provide system-level versions of the latest sepsis report in the coming weeks.
If you have suggestions on how these reports can be improved or the data made more actionable, the Coordinating Center would love to hear from you. We are also seeking feedback on how collaborative members are using this information in their quality improvement projects. Please reach out at Michigan-Value-Collaborative@med.umich.edu.