When most people think about healthcare, the images that come to mind include a trip to their local provider’s office, lab, or hospital for services such as physicals, blood tests, and procedures. However, medical professionals and their patients are increasingly transitioning to more remote services that leverage our advances in communication technologies, resulting in the burgeoning “tele” world of healthcare. But are these services reaching everyone?
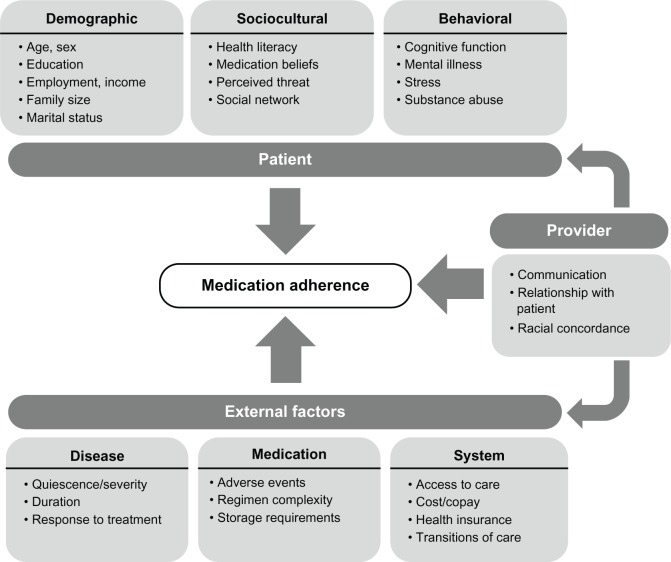
Telemedicine, telehealth, and telecare are three examples of remote, interactive services that allow patients to receive healthcare from within their own homes. Although these terms are often used interchangeably, they in fact refer to different aspects of healthcare delivery. Telemedicine applies to physicians who use technology to support the delivery of medical, diagnostic, or treatment-related services. Telehealth is like telemedicine but applies to a broader collection of providers, such as nurses or pharmacists. Telecare (see Figure 1) is generally more consumer-oriented by providing the patient with technology to manage their own care safely from home, such as health apps or digital monitoring devices.
Figure 1. Telecare Slide from MVC Workgroup Presentation

The adoption of “tele” services saw incredible growth in 2020 in response to the pandemic. A report found that Medicare telehealth visits increased 63-fold recently, from 840,000 in 2019 to 52.7 million visits in 2020. However, now that adoption of these services (and the platforms needed to host them) are more commonplace, providers are asking whether it benefits their most vulnerable patients and who may be left behind.
These questions drove the discussion of the most recent MVC workgroup on chronic disease management. Over the course of the session, attendees were particularly interested in how telecare improves elderly care, and whether patients over the age of 65 could adequately access such services. For those older adults utilizing telecare, evidence from the ongoing COVID-19 pandemic identified convenience and affordability as telecare’s primary strengths. In addition, research evidence suggests that the two most effective telecare interventions in this population are automated vital sign monitoring and telephone follow-up by nurses.
Some of the challenges often cited for this population include lack of appropriate internet access or devices, limited digital literacy, medical conditions that may impede participation (i.e., hearing or vision impairments, dementia, etc.), and the need to regularly monitor vitals in very high-risk patients. Although the authors compiling these challenges specifically reference older adults, they could just as easily apply to people experiencing poverty, people with disabilities, and people with more limited language and literacy skills.
Some recommended strategies to address common challenges include tablet delivery services, “mobile medical assistants” who perform video set-up for the patient, assistance from an on-site caregiver, practice or “mock” video visits prior to the appointment date, partnerships with community health workers to support or train patients in their homes, and providing self-monitoring devices. Other simple considerations include the size of the text displayed on the page (use larger text to enhance readability), providing adequate instructions in advance and in multiple languages, and engaging experts in user experience design.
In addition to these considerations, some researchers suggest that, in general, the adoption of new technologies can be predicted in part by Everett Rogers’ Diffusion of Innovation Theory. One study incorporating this theory found that the chances of telecare adoption were highest for three types of older adults: those already receiving long-term or nursing care, those living alone, and those who have fixed daily telecare points of contact.
Increased integration of technology in healthcare is inevitable as advancements continue and we shift to a more digital world. Since the number of people in the U.S. who are age 65 or older will more than double over the next 40 years, it is imperative that older adults are not left behind when transitioning to such services. Rather than fear the challenges, researchers and practitioners are seeking ways to find solutions and help all patients benefit from healthcare access within their own homes.
The MVC Coordinating Center encourages its members to collaborative with one another to benefit from peers’ success stories and lessons learned. If your hospital or physician organization has developed an age-friendly telecare protocol, please consider sharing your story with the MVC Coordinating Center at michiganvaluecollaborative@gmail.com. To catch up on the recent MVC workgroup discussion about telecare, watch the chronic disease management workgroup recording here.