In August, MVC hosted two virtual workgroup presentations – a preoperative testing workgroup focused on planning and evaluation of an initiative to reduce unnecessary preoperative testing, and a health in action workgroup on the Michigan Department of Health and Human Services (MDHHS) behavioral health initiative. The MVC Coordinating Center hosts workgroup presentations twice per month on a variety of topics including post-discharge follow-up, sepsis, cardiac rehabilitation, rural health, preoperative testing, and health in action.
Preoperative Testing Workgroup - Holland Hospital
On Aug. 12, MVC hosted a preoperative testing workgroup with a presentation by Amy Poindexter, BSN, RN, from Holland Hospital. Poindexter is the Performance Improvement Analyst in Holland Hospital’s quality department and played an integral role in their quality initiatives over the past 16 years. Her work includes data abstraction for Core Measures, Michigan Hospital Medicine Safety Consortium (HMS), Michigan Surgical Quality Collaborative (MSQC), and the Multicenter Perioperative Outcomes Group (MPOG) Anesthesiology Performance Improvement and Reporting Exchange (ASPIRE) registry.
Holland Hospital’s quality initiative focused on reducing unnecessary, routine preoperative testing within 30 days of low-risk elective surgeries. Conditions included in the project were elective hernia, lap cholecystectomy, and breast lumpectomy. The types of testing that were considered included electrocardiograms (ECG), transesophageal echocardiogram (TEE), cardiac stress test, chest x-ray, urinalysis, labs (CBC, BMP, coagulation tests), and pulmonary function tests (PFT). Baseline data used for this initiative was based on Blue Cross Blue Shield of Michigan (BCBSM), Medicare, and Medicaid patient episodes from January 2023 – March 2023. The initiative goal was to reduce unnecessary preoperative testing by 20% through December 2023.
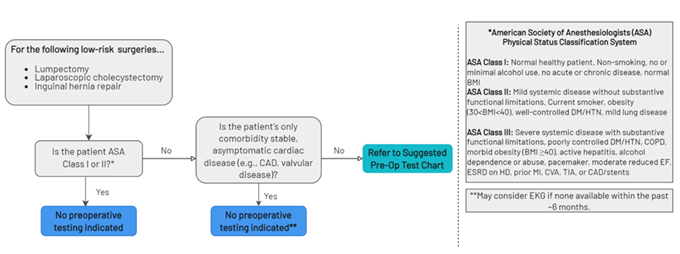
The parameters for selecting the preoperative tests were based on recommendations from several well-known medical societies. The American Society of Anesthesiologists recommends not obtaining baseline laboratory studies in patients without significant systemic disease (ASA I or II). The American College of Cardiology recommends avoiding performing ECG screening as part of the preoperative cardiovascular risk assessment in asymptomatic patients scheduled for low-risk non-cardiac procedures. Guidelines to not perform chest x-rays on patients with unremarkable history and physical exams, which are provided by the American College of Radiology and American College of Surgeons, were also used to establish preoperative testing parameters. Holland Hospital used the RITE-size decision aid (Figure 1) to guide testing logic:
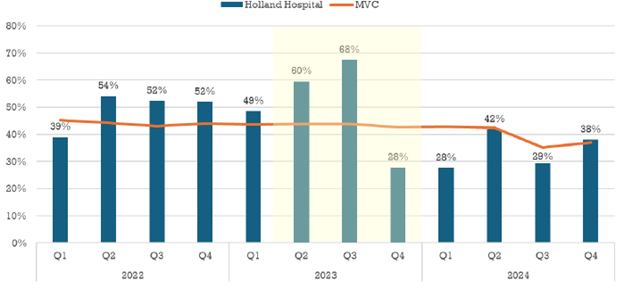
Prior to implementing the quality initiative to improve preoperative testing rates, Holland Hospital worked with MVC claims data and MSQC abstracted clinical data from Q1 2023 to develop a baseline data visualization tool. The hospital found that their preoperative testing rates for low-risk surgeries were approximately 10% higher than the MVC All average. According to the sampled cases from MSQC, their average baseline rate was approximately 33%. Holland Hospital set a goal of reducing preoperative testing by 20% (the average rate would need to be less than or equal to 26%) by the end of December 2023.
Planning Phase
During the pre-implementation phase of planning, the hospital formed a multi-disciplinary team including pre-admission testing (PAT) staff, surgery providers, hospital leadership, anesthesiologists, and quality improvement staff. The team focused on their pre-admission testing lab draw (basic chemistry panel) policy, which was focused on general and major anesthesia of male and female patients ages 65 – 74 and patients aged 75 and older for specific types of labs such as epidural, spinal, regional, and brachial plexus. Initially, labs were drawn within one month of the procedure, but with the revised policy, patients undergoing low-risk general procedures such as elective hernia or lap cholecystectomy only required labs within 60 days of their procedure. In addition, the process shifted to establish the pre-admission assessment as the trigger for the preoperative testing decision chart.
Evaluation
After analyzing the percentage of preoperative screening tests ordered for the associated low-risk procedures, Holland Hospital found that in 2022 they were ordering preoperative tests at a rate of approximately 52% (MVC All rate equaled approximately 45%). With further investigation of preoperative test ordering practices, the site found that of the physicians ordering the tests, 71% were surgeons and 29% were primary care providers (PCPs). Interestingly, the PCP orders would often fall within the 30-day window as the turnaround time from PCP appointment to surgery appointment was happening within a month. It was discovered that physicians had been following old guidelines that were given to them when they were initially onboarded at the hospital in prior years. This finding initiated the implementation of provider education and a slight change in ordering practices.
To improve ordering accuracy, the PAT team was assigned the responsibility of checking and ordering any preoperative tests needed instead of the surgeons ordering them. As shown in Figure 2, the preoperative testing rates remained above average through September 2023 until provider education and process changes were fully implemented at the end of Q3. After implementing provider education, testing rates showed a significant reduction through the end of 2023.
Figure 2. Holland Hospital Preoperative Testing Rates in 30 Days Prior to Admission for Low-Risk Surgery – Pre-Implementation through Post-Implementation of QI
Workgroup participants asked Poindexter whether other staff had the ability to order preoperative lab tests (such as anesthesia staff) and whether surgical or anesthesia staff were internal or external contracts (Holland Hospital has a mix). Participants were also curious to know how internal or external contracts impacted consistent education. Poindexter noted the education piece was an easier lift at their smaller site, since they only have a few surgical physicians. Participants discussed best practices such as having an updated preoperative testing education program in place for physicians and surgical teams, utilizing RITE-size resources, and including an editable letter and related resources for PCPs about preop testing guidelines and procedures.
MVC Preoperative Testing Workgroup: Aug. 12, 2025
Health in Action Workgroup - MDHHS
On Aug. 28, MVC hosted a health in action workgroup with a MDHHS presentation by Lindsey Naeyaert, MPH, Director of Behavioral Health Transformation in Health Services, and Leah Julian, Innovation in Behavioral Health Specialist in Health Services. Naeyeart leads and directs policy development and changes, program operations, analysis, research, and reporting of integrated health models at MDHHS. Julian is responsible for planning, implementation, and oversight of the Innovation in Behavioral Health (IBH) Model in partnership with the Centers for Medicare & Medicaid Services (CMS). Naeyaert and Julian presented the three programs currently offered through MDHHS: Behavior Health Home, Certified Community Behavioral Health Clinics, and the Innovation in Behavioral Health Model.
Behavior Health Home (BHH)
The BHH is one of the longest running Medicaid optional state plan benefits, authorized under the 1945 US Social Security Act. This plan allows for more flexible funding towards care for serious and complex chronic conditions of Medicaid beneficiaries. The purpose of the BHH plan is to serve the “whole person” by including physical, behavioral, and social services through an interdisciplinary care team. The goal of this program is to integrate care, create cost-efficiencies, and increase participant health status. This plan is available for people with Medicaid who have two or more chronic conditions, or one chronic condition and are at risk for a second condition.
In 2014, MDHHS launched a county model of BHH and revamped the design in 2020. The updated program targeted beneficiaries with a diagnosis of Serious Mental Illness (SMI) or Serious Emotional Disturbance (SED). The service area includes 79 counties and 40 home health providers including community mental health services programs, federally qualified health centers, hospital-based clinical practices, rural health clinics, and tribal health centers. In fiscal year (FY) 2024, there were 4,399 people enrolled with ages ranging from 4-86.
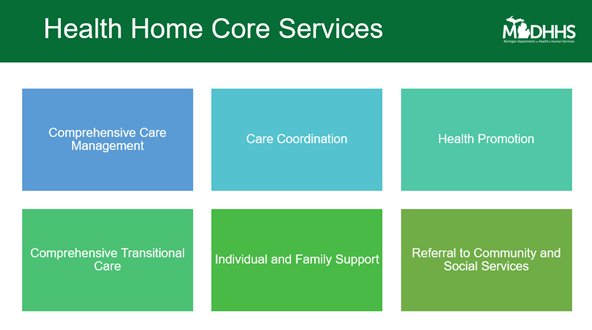
Under this plan, interdisciplinary team members can now be reimbursed for services provided under Health Home Core Services (HHCS) that in the past could not be billed. For example, if the team meets to discuss a patient’s treatment plan it can be billed under care coordination through HHCS (Figure 3). Other covered services include comprehensive care management, health promotion, comprehensive transitional care, individual and family support, referral to community, and social services.
Figure 3. Health Home Core Services
Since the implementation of the program, there have been several positive outcomes observed such as increased post-discharge follow-up for mental illness or intentional self-harm episodes, increased care coordination between physical and mental health providers, increased control of high blood pressure, and increased access to preventive/ambulatory health services.
Certified Community Behavioral Health Clinics (CCBHCs) Demonstration
CCBHCs are non-profit or local government agencies that must meet robust state certification criteria (200 standards). These sites must serve all people, regardless of insurance status or ability to pay, and are required to work with local hospitals as part of their certification criteria. These sites use a state-developed and clinic-based prospective payment system model for reimbursement. There are currently 35 demonstration sites across the state of Michigan. The primary objectives of CCBHCs are to increase access to high-quality services that use evidence-based practices; coordinate behavioral health, physical health, and social needs; promote the use of evidence-based practices; and establish statewide standardization and consistency using the same criteria across all certified clinics.
In year three (FY 2023) through four (FY 2024), MDHHS added 17 CCBHC sites in Michigan and expects to add 10 more sites by FY 2025. Data collected through FY 2024 shows positive impacts on participating patient populations and CCBHCs. Overall, CCBHCs have seen a 77% increase in individuals served since development year two, with 81% of participating patients enrolled in Medicaid. Some patients with commercial health plans have been able to see providers at CCBHCs as well. Data also shows that 23% of CCBHC patients were children 18 years old and younger. This suggests that parents are bringing their children to see the same providers they do, making it easier for them to access care for all family members in one location. Additional findings show that even though they may have other clinics closer to home, 11% of patients were served outside their county of residence, meaning they are specifically seeking CCBHCs for treatment.
Naeyeart shared that CCBHCs exceeded statewide averages for Medicaid beneficiaries in the following areas:
- Follow-up after emergency department visit for mental illness
- Follow-up after emergency department visit for alcohol and other drug dependence
- Follow-up after hospitalization for mental illness
- Diabetes screening for people with schizophrenia or bipolar disorder who are using antipsychotic medications
- Adherence to antipsychotic medications for individuals with schizophrenia
- Plan all-cause readmission rate
- Initiation and engagement of alcohol and other drug dependence treatment
Innovation in Behavioral Health (IBH) Model
The newest program launched is the IBH model. Julian shared that Michigan had been selected to participate in the IBH model in 2024 and began participation on Jan. 1, 2025. This is a cooperative agreement with CMS focused on improving the quality of care and behavioral and physical health outcomes for adults enrolled in Medicaid and Medicare with moderate to severe mental health conditions and substance use disorder. The goal is to assist in minimizing barriers to high quality integrated care.
The core elements of the IBH framework include:
- Care Integration – Behavioral health practice participants will screen, assess, refer, and treat patients as needed for the services they require.
- Care Management – An interprofessional care team led by the behavioral health practice participant will identify and address multifaceted needs of patients for ongoing care.
- Health Information Technology – Expansion of health information technology capacity through targeted investments in interoperability and tools (e.g. electronic health records) will allow participants to improve quality reporting and data sharing.
The primary objectives of this program are to improve quality and delivery of whole person care, align care delivery and payment systems between Medicare and Medicaid, explore Medicaid payment strategy, develop value-based payment methodologies, and improve health information systems to improve quality and data sharing.
This program aims to work with providers who are integrated and engaged with CCBHC or BHHs, sites that are Medicaid entities, providers that serve at the outpatient level with at least 25 people enrolled in Medicaid per month, and sites that provide mental health and or substance use disorder services at the outpatient level of care. The model has an eight-year performance period, including three years of planning (2025-2027) and five years for implementation (2028-2032). In the current planning phase, the focus is on building the structure for the model’s framework identifying stakeholders (e.g., state personnel, practice participants, community organizations, etc.), developing a recruiting strategy, designing a care delivery framework, establishing a Medicaid payment approach, and designing an effective health information technology plan.
Workgroup participants inquired about any intention of collaborating with other CQIs like the Michigan Mental Health Innovation Network for Clinical Design (MI Mind) or community-based organizations like Salvation Army or the Young Women’s Christian Association (YWCA) system. Workgroup participants expressed significant interest in being involved with this model as participant partners.