Earlier this spring, the Michigan Cardiac Rehab Network (MiCR) hosted its virtual spring meeting with 74 attendees joining from cardiac rehab programs and hospitals across the state. MiCR was glad to host two guest presenters for the meeting, including Alexis Beatty, MD, MAS, Co-Director of the UCSF Cardiac Rehab and Wellness Center, and Brett Reynolds, MPH, ACSM, CEP, Supervisor of Cardiology for Corewell Health East. The primary goal of MiCR meetings is to support shared learning, practice sharing, and networking among professionals working with cardiac rehabilitation programs across Michigan.
The meeting began with MiCR team updates provided by Co-Director Mike Thompson, PhD – most notably the introduction of Dr. Jessie Golbus, MD, MS, as the new co-director of MiCR (see Figure 1). Dr. Golbus is an Assistant Professor of Internal Medicine in the Division of Cardiovascular Medicine at Michigan Medicine.
Figure 1.
Dr. Thompson also announced a new grant from the University of Michigan's Frankel Cardiovascular Center awarded to Healthy Behavior Optimization for Michigan (HBOM) and MiCR for their new Heart-to-Heart initiative. Heart-to-Heart is a new initiative aiming to amplify the real, diverse voices of Michigan patients who have experienced cardiac rehabilitation. Patient stories told through compelling audio, visual, and written storytelling will foster broader conversations about the life-changing impact of cardiac rehabilitation and inspire those considering attendance. HBOM and MiCR previously partnered on the development of NewBeat materials. Following the virtual meeting, BMC2 published a blog introducing the new Heart-to-Heart initiative.
Dr. Thompson then provided insights into improvements in cardiac rehabilitation utilization in Michigan since the inception of MiCR. The network is committed to boosting enrollment to 40% across all eligible conditions except heart failure, for which it has a lower target of 10% enrollment. Dr. Thompson noted encouraging trends observed since 2020, with overall enrollment rising to 35% from just under 25%. Although heart failure patient enrollment remains low at approximately 4%, efforts are under way to improve enrollment in this population in the future.
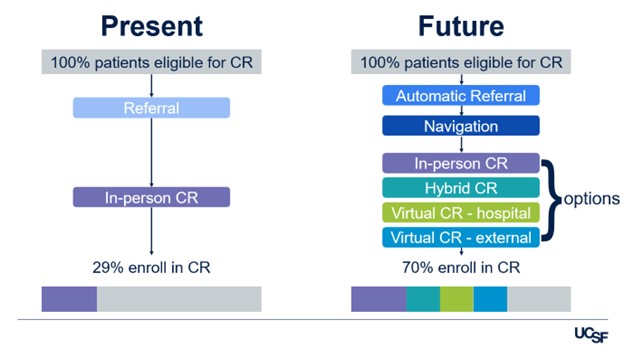
Dr. Alexis Beatty, MD, MAS, co-director of the UCSF Cardiac Rehab and Wellness Center, delivered the first guest presentation on the transformative potential of telehealth in cardiac rehabilitation. She highlighted the advantages and potential of integrating telehealth and hybrid models with traditional center-based programming to increase accessibility and participation (see Figure 2). Since adopting a hybrid model during the COVID-19 pandemic, UCSF reported substantially improved completion rates in virtual and hybrid programs compared to exclusively in-person sessions. Furthermore, patient outcomes related to exercise capacity, risk factor management, and quality of life were consistent across all formats.
Figure 2.
Dr. Beatty also introduced an online delivery model toolkit (available at UCSF Cardiac Rehab Toolkit), crafted using human-centered design methods to aid in telehealth program development. This toolkit includes adaptable templates for exercises and safety and is already utilized by clinics in Michigan and beyond, allowing for flexibility to meet local patient needs. Dr. Beatty’s full slide presentation is available online.
In the second presentation, Brett Reynolds, MPH, ACSM, CEP, supervisor of cardiology at Corewell Health East, showcased their "Weight of Heart Failure" quality improvement initiative. Funded by a MiCR mini grant, the project sought to improve engagement and outcomes for heart failure patients. This initiative was a response to declining cardiac rehabilitation enrollments among heart failure patients. Grant funds were used to purchase 100 Corewell Health-branded scales for daily weight monitoring, accompanied by educational materials to aid in health management. The project also included follow-up calls two weeks post-discharge to verify if patients were monitoring their weight and had scheduled follow-up appointments.
Reynolds reported that of the 156 heart failure patients reached, 110 follow-up calls were completed, with 65% consistently tracking their weight and 83% scheduling follow-up appointments. This proactive approach seemed to have contributed to an increase in participation.
Despite the success, Reynolds acknowledged persistent challenges, such as referral system barriers and limited physician awareness regarding cardiac rehabilitation eligibility for heart failure. However, the initiative's efficacy in enhancing follow-up care and patient involvement highlighted the potential impact of targeted interventions in heart failure management. The full Corewell Health slide presentation is available online.
The webinar concluded with announcements of upcoming opportunities to engage with the network and collaborate to improve cardiac rehabilitation care in Michigan. Most notable among these opportunities is MiCR’s upcoming in-person fall meeting, which is set to take place on Thurs., Nov. 13 at Corewell Health Troy. Those interested in attending can register now.




