The Michigan Value Collaborative (MVC) Coordinating Center disseminated it’s long-running customized cardiac service line report to hospital and physician organization (PO) members on February 23, 2021. These reports provide hospital-level information on congestive heart failure (CHF), acute myocardial infarction (AMI), and coronary artery bypass graft (CABG) conditions. To receive information on any one of these conditions, a hospital must have at least 20 cases per year over the three-year reporting period (1/1/17 – 12/31/19).
Since the last iteration of the cardiac service line report sent in June 2020, the Coordinating Center has defined four distinct regions within Michigan, allowing members to make regional comparisons. These comparisons have been incorporated into the 30-day risk-adjusted total episode payment trend chart, the post-acute care utilization bar graph, and the 30-day readmission rate trend chart of the reports as shown in the following AMI figures for a fictional institution, Hospital A.
Acute Myocardial Infarction Figures. Hospital A
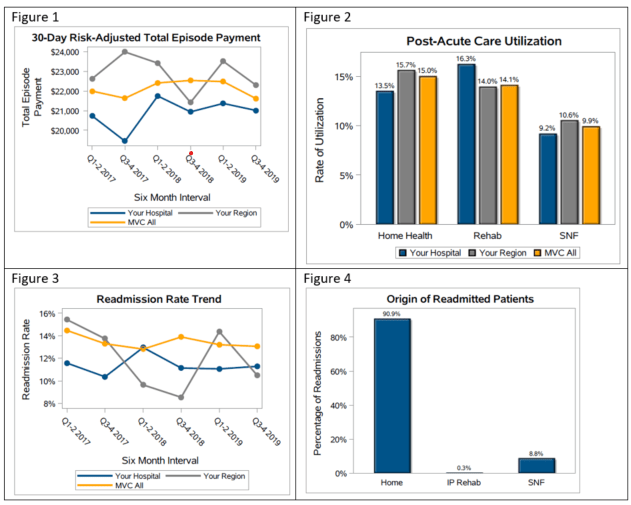
Figure 1 shows the 30-day risk-adjusted total episode payments broken up into six-month intervals, illustrating that episode payments for AMI hold steady across the Collaborative at an average of around $22,000. Please note that as with all MVC reports, this represents price standardized dollars to allow for fair comparisons between hospitals. The price standardized dollars can be thought of as a measure of utilization as opposed to true dollar amounts.
Figure 2 displays the percentage of AMI patients who utilized home health (15.0% across MVC), rehab (14.1% across MVC), or skilled nursing facilities (9.9% across MVC). Figure 3 illustrates that, between 2017 and 2019, approximately 14% of AMI patients were readmitted within 30 days. Finally, Figure 4 shows Hospital A that based on the most recent claim before a readmission occurred, 90.9% of readmitted patients were coming from home, 8.8% were coming from Skilled Nursing Facilities (SNF), and very few were coming from inpatient rehabilitation (0.3%). Hospitals can use this information to observe if they are an outlier in any of the categories and where they may have an opportunity to improve, to benchmark themselves against the MVC all and regional averages, and to notice trends in their performance
These combined-payer push reports are distributed twice a year, meaning the next iteration is likely to be sent out in the summer of 2021. In the meantime, single-payer information is always available on the MVC registry, allowing for continued monitoring of these metrics. Data is added every month for Blue Cross payers and quarterly for Medicare. Michigan Medicaid data will be live on the registry at the start of Q2 this year.
If you need registry access, if you have ideas on how these reports can be made more versatile, or if you are using these data for a quality improvement project at your institution, please contact michiganvaluecollaborative@gmail.com. Additionally, please reach out if you want further information in the way of custom analytics.